Introduction
The rate of cervical cancer prevalence in Australia is 7 cases per 100,000 women (Cervical Cancer: What is Cervical Cancer? 2014). Cervical cancer has been cited as the cause of approximately 1.7% of all deaths caused by cancer in Australia (Cervical Cancer: What is Cervical Cancer? 2014). Its prevalence in Australia declined significantly after the introduction of the National Cervical Screening Program (Cervical Cancer: What is Cervical Cancer? 2014).
Cervical cancer is a preventable disease with early diagnosis and proper utilisation of diagnostic procedures. Precancerous lesions undergo several stages of growth before they develop into invasive cancer that is difficult to treat. Understanding the role of imaging and radiation therapy in the diagnosis and treatment of cervical cancer is important, especially for effective prevention and management. In addition, it can contribute significantly toward the reduction of deaths and new cases of cervical cancer reported every year in Australia and other parts of the world. Imaging is one of the procedures conducted during diagnosis to determine whether cancer has spread to other parts of the body (Cervical Cancer in Australia, 2016).
Radiation therapy is a treatment remedy that involves the use of high-energy radiation to annihilate cancerous cells. In certain cases, radiation therapy is used as the only treatment method. Proper treatment is based on proper cancer staging that is conducted using medical imaging technologies. Evaluation of past research studies and medical literature will be conducted in order to obtain more information regarding the topic.
Imaging
Advances in imaging technology have improved the diagnosis of cervical cancer by enhancing the precision of determining its spread to other body parts. Advanced diagnosis methods have lowered their prevalence. The incidence of cervical cancer in Australia in 2015 is shown in the table below.
Table 1: 2015 prevalence of cervical cancer in Australia by age group (Cervical Cancer in Australia, 2016).
The most common imaging technologies used in the diagnosis of cervical cancer include computed tomography (CT), Ultrasound (US) and magnetic resonance imaging (MRI). Others include positron emission tomography (PET), ultrasonography, and lymphangiography.
Role of imaging in cervical cancer diagnosis
Ultrasonography is used to identify uterine and cervical leiomyomas and evaluate the urinary tract for the incidence of obstruction in cases where cancer has spread to other body organs (Saksouk, Coombs, Reuter, & Lin, 2015). In addition, it is used to determine the size of the cervix. It has low contrast resolution. Therefore, it is not an effective imaging technique to visualise tumours. Computed tomography is now widely used and has become a common technique because of technological advancements.
However, it has several limitations that include contrast enhancement, inconsistency in the direct visualisation of primary cancer tumours, inaccuracy with regard to detection of tumours that invade the bladder, and inclusion of metastasis in images of normal-sized lymph nodes. A CT is performed by taking several cross-sectional images of the cervix and adjacent organs.
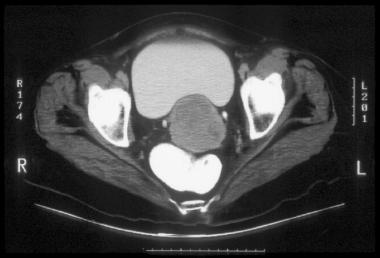
The roles of CT in cervical cancer staging include evaluation of cervix size and detection of abnormalities involving lymph nodes (Choi, Ju, Myung, & Kim, 2010). It is also useful in determining whether cancer has spread to other body regions and organs. In addition, it facilitates the identification of obstruction in the ureter (Cervical Cancer in Australia, 2016). Its effectiveness and efficiency are limited by the use of tissue discriminator media because it does not aid in the determination of lymph nodes’ architecture.
MRI is used by many doctors because of its cost-effectiveness and ability to produce high tissue contrast resolution. The main role of MRI in diagnosis is the determination of cervix size and identification of cervical invasion (Saksouk et al., 2015). Moreover, it is used to study the characteristics of lymph nodes. MRI is performed using radio waves that are absorbed by affected tissues and released to form a pattern that is translated by a computer to form a detailed image of the body parts imaged (Rigon, 2012).

PET is effective in the detection of abnormalities in lymph nodes regions (Saksouk et al., 2015). It can be used together with CT to determine the dimensions of cancer tumours (Choi et al., 2010). It is conducted using glucose that contains radioactive atoms that are absorbed by cancer cells. Lymphangiography is used to identify the presence of abnormalities in lymph nodes as well as their sizes and architecture. This method is highly effective because the contrast material used during imaging remains in the lymph nodes for a significant period of time. Therefore, doctors can use the lymph nodes with the contrast material to make plans regarding radiation treatment.
Ultrasound is an important technique that aids in cancer staging by showing the presence of tumours in the vagina and adjacent organs (Saksouk et al., 2015). In addition, it is used to evaluate the size of the tumours. This technique is usually applied in advanced stages of cervical cancer. A transabdominal ultrasound is conducted by passing a transducer over the lower belly of a patient, and the sound waves are relayed to a computer screen that transforms them into an image.

Role of radiation therapy in the treatment of cervical cancer
Radiation therapy is one of the approaches used by physicians to treat cervical cancer. It involves the use of high-energy x-rays to destroy cancerous cells (Radiotherapy for Cervical Cancer, 2014). The two approaches used during treatment include internal and external therapy. Internal therapy (brachytherapy) involves the destruction of cancer cells using radiation that originates from implants placed within the body.
Such implants remain in the womb for specific periods of time either hours or days depending on the treatment regimen. They are effective because the affected area receives high doses of radiation without any effect on the skin and surrounding tissues (Radiotherapy for Cervical Cancer, 2014). In contrast, external therapy involves the destruction of cancer cells using radiation from a linear accelerator (linac) outside the body (Radiotherapy for Cervical Cancer, 2014).
The treatment period could last between 5 and 8 weeks depending on the type and location of cancer, general health status, the reason for treatment, and size of tumours. External-beam radiation therapy is the most common radiation technique used by doctors because it does little damage to tissues and focuses radiation more accurately when compared to internal radiation therapy (Rajaram, Chitrathara, & Maheshwari, 2012).
The radiotherapy team develops individualised treatment plans for patients based on their cancer staging results. The plan involves the determination of how much radiation the patient needs and the specific regions or organs of the body that need to be targeted. A treatment plan includes a CT scan that defines the treatment port. Internal radiation therapy involves the insertion and removal of a radiation source into the womb (Rajaram et al., 2012).
External beam radiotherapy involves the use of a linear accelerator. A radiation therapist marks the treatment field using ink for easier and accurate focusing of radiation beams. The amount of radiation administered is dependent on the cancer type and results obtained from the simulation process (Rajaram et al., 2012).
Conclusion
Proper treatment of cervical cancer depends on proper diagnosis. Imaging is an important aspect of cervical cancer diagnosis because it aids in cancer staging. Cancer staging is critical in determining the treatment method to use based on the size and location of cancer. The size and location of the cancer are determined using various medical imaging techniques such as computed tomography (CT), positron emission tomography (PET), ultrasonography, lymphangiography, Ultrasound (US), and magnetic resonance imaging (MRI). Results obtained from imaging are used to choose the best treatment method or procedure.
Radiation therapy is one of the most effective treatment methods that involve the use of radiation to annihilate cancer cells. Imaging uses different techniques to produce images of affected tissues and organs, while radiation therapy destroys cancer cells using high-energy radiation emitted by a linear accelerator. The linac directs a specific amount of radiation toward various treatment ports from different angles.
References
Cervical Cancer in Australia. (2016). Web.
Cervical Cancer: What is Cervical Cancer? (2014). Web.
Choi, H. J., Ju, W., Myung, S. K., & Kim, Y. (2010). Diagnostic Performance Of Computer Tomography, Magnetic Resonance Imaging, and Positron Emission Tomography or Positron Emission Tomography/Computer Tomography for Detection of Metastatic Lymph Nodes in Patients with Cervical Cancer: Meta-Analysis. Cancer Science 101 (6), 1471-1479.
Radiotherapy for Cervical Cancer. (2014). Web.
Rajaram, S., Chitrathara, K., & Maheshwari, A. (2012). Cervical cancer: Contemporary Management. Philadelphia, PA: Jaypee Brothers Publishers.
Rigon, G., Vallone, C., Starita, A., Vismara, M. F., Ialongo, P., & Signore, F. (2012). Diagnostic Accuracy of MRI in Primary Cervical Cancer. Open Journal of Radiology 2, 14-21.
Saksouk, F. A., Coombs, B. D., Reuter, K. L., & Lin, E. C. (2015). Cervical Cancer Imaging. Web.