Creating a Concept Map
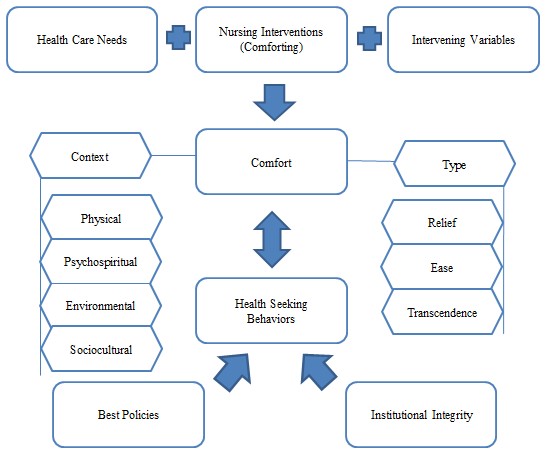
The comfort theory first introduced by Katharine Kolcaba in the 1990s is one of the widely recognized middle-range theories in nursing (McEwin & Wills, 2019). It includes several concepts, including the four basic nursing conceptual components: health, person, environment, and health. The framework also introduces concepts unique to the theory – comfort, health care needs, intervening variables, health-seeking behaviors (HSBs), and more (Gray et al., 2017). The connection between these ideas can be shown with the help of concept mapping that places concepts in relation to one another (Veo, 2010). The following concept map outlines the main concepts of the comfort theory and its relational statements.
Problem and Purpose Statement
As can be seen from the concept map, comfort is the central concept of the theory – it is influenced by several variables while also influencing health-seeking behaviors (HSBs) and healthcare organization policies. The relationship between nurses’ comforting interventions and the patients’ comfort is the foundation of the theory. The problem is that patients’ health is influenced by their level of comfort, and nurses need to make decisions to facilitate enhanced comfort. Thus, nursing is defined by assessing patient needs and actions to influence and evaluate patient comfort (Faria et al., 2018). The purpose of the comfort theory is to establish the link between nursing interventions and patients’ comfort.
Relational Statements’ Description
The first group of relational statements is the influence of various factors on the creation and improvement of comfort. First, the health care needs are defined either by the patient or the family influence the level of comfort (McEwin & Wills, 2019). Second, the nurses’ interventions are the actions that nurses take to make sure that the patient is comfortable (McEwin & Wills, 2019). As noted above, they include assessment of the patient’s needs, the selection of an appropriate intervention, and the evaluation of the patient’s comfort level (Berntzen et al., 2020). Finally, the patient’s comfort is also influenced by intervening variables – a set of factors that cannot be controlled or are unlikely to change. Intervening variables may include the patient’s prognosis, their social-economic status, family support, and others.
HSB and comfort are two interlinked concepts that influence one another. On the one hand, Kolcaba poses that the improvement of comfort can lead to patients expressing more desire to enhance their health. As higher comfort reduces the tension the patient experiences due to their health problems, it also creates a better foundation for healing (McEwin & Wills, 2019). On the other hand, it is possible to pose that health-seeking behaviors increase the patients’ ability to experience comfort as they are available for nursing interventions. Finally, the organization’s policies and integrity can positively affect the patients’ HSB. The best policies concept refers to the procedures organizations create based on evidence of best comfort-improving behaviors. Similarly, the financial stability and values of the institution make its integrity. This is the relational statement – best policies and organizational integrity influence patients’ health-seeking behaviors by facilitating comfort improvement.
Conclusion
The middle-range theory of comfort uses the concepts of comfort, nursing interventions, health-seeking behaviors, intervening variables, and others. The central idea is that patients’ comfort is important in their care. Therefore, nurses should develop interventions to improve patient comfort, although other factors can either help or create problems in this process. The theory’s relational statements demonstrate a link between nurses’ behavior, the organization’s environment, and patient outcomes. This ideology can be used in practice for a variety of healthcare problems.
References
Berntzen, H., Bjørk, I. T., Storsveen, A. M., & Wøien, H. (2020). “Please mind the gap”: A secondary analysis of discomfort and comfort in intensive care. Journal of Clinical Nursing, 29(13-14), 2441-2454.
Faria, J. M. S., Pontífice-Sousa, P., & Gomes, M. J. P. (2018). Comfort care of the patient in intensive care – An integrative review. Enfermería Global, (50), 503-514.
Gray, J.R., Grove, S.K., & Sutherland, S. (2017). Burns and Grove’s the practice of nursing research: Appraisal, synthesis, and generation of evidence (8th ed.). Saunders Elsevier.
McEwin, M., & Wills, E. M. (2019). Theoretical basis for nursing (5th ed.) Wolters Kluwer Health.
Veo, P. (2010). Concept mapping for applying theory to nursing practice. Journal for Nurses in Staff Development, 26(1), 17-22.