Abstract
If not treated timely, cardiac arrest presents a significant problem for patients in the intensive care unit (ICU). Nurses’ skills and use of advanced knowledge greatly influence cardiopulmonary resuscitation – the use of capnography, for example, is considered to improve CPR results. The purpose of this quantitative, quasi-experimental pretest-posttest project is to determine to what degree the implementation of capnography during cardiopulmonary resuscitation (CPR) when compared to the current practice would impact nurses and increase the use of capnography during CPR for adult ICU patients at an acute care hospital in New Jersey. The project is based on Lewin’s change theory; the author proposes that any change process has three main steps: unfreeze, change, and refreeze. The quantitative methodology was selected due to its ability to address clinical questions with meaningful, quantifiable, and transparent results. The project utilizes a quasi-experimental design to choose the sample and manipulate the independent variable, the nursing training program of capnography use during CPR, to influence the dependent variable, the number of CPR cases with the use of capnography. The population under investigation is adult patients who had a cardiac arrest and underwent CPR while in the ICU. The data, obtained from the Nurses’ Knowledge on Capnography Test and EHR, were analyzed with a paired sample t-test and Gain’s score to note pretest-posttest differences in nurses’ use of capnography before and after training. [data results and implications to be added later]
Introduction to the Project
Nurses’ knowledge pertaining to clinical devices used for monitoring, assessing, and treating patients with heart conditions is an important factor for achieving quality of patient care and organizational effectiveness (Cook & Harrop-Griffiths, 2019). Studies conducted by Linet al. (2017), Novais and Moreira (2015), and Pantazopoulos et al. (2015) alluded to the lack of knowledge among nurses in using capnography as recommended by the Advanced Cardiac Life Support (ACLS) to capture pertinent information about a patient’s end-tidal carbon dioxide (ETCO2) condition.
They found that such low awareness of this approach presents uncertainties and poor clinical monitoring practices. Low-quality nursing practices are exemplified by the lack of awareness in using capnography; especially, when success in patient care is dependent upon the practice knowledge and use of innovative devices such as capnography in a clinical setting (Hamrick et al., 2017).
In another study, Hamrick et al. (2017), Heradstveit and Heltne (2014), and Kodali and Urman (2014) linked the importance of using capnography in monitoring and gathering patient information during cardiopulmonary resuscitation events to the critical role of nursing practitioners and the knowledge in using capnography to improve patient quality care.
The scholarly debate persists regarding the complexities in instituting clinical monitoring devices in the clinical setting and the lack of knowledge to effectively use the device. The rationale for this project lies in its potential beneficial effects on increasing the use of capnography in the intensive care unit (ICU) setting. Finally, the findings presented could be used to enhance the awareness about the project and its objectives.
Background of the Project
Cardiac arrest poses a significant threat to patients in intensive care units and is a significant factor that can subsequently lead to a patient’s demise if not addressed timely (Hartmann, Farris, Di Gennaro, & Roberts, 2015). As a result, the use of capnography to improve the outcomes of patients during cardiac arrests has been widely studied in the literature (Edelsonet al., 2014; Mader, Coute, Kellogg, & Harris, 2014). According to Cereceda-Sánchez and Molina-Mula (2017), capnography has been developed as a measurement for monitoring coronary perfusion pressure (CPP) and coronary blood flow.
Recent studies have shown the effectiveness of capnography in patients’ treatment with chronic hypercapnic respiratory failure, hypoventilation, severe hypothermia, and metabolic changes clinical (Darocha et al., 2017; Cereceda-Sánchez & Molina-Mula, 2017; Chhajed et al., 2016). However, Leppink, O’Sullivan, and Winston (2016) noted that despite the existence and widespread use of capnography in practice improvement, many nurses still show some levels of uncertainty due to the reduced awareness in the knowledge and application of capnography in clinical settings.
Recent studies conducted by Dioso (2014) and Duckworth (2017) amplified the importance of equipping nurses with the knowledge of the application of capnography as a technique to manage cardiac arrest incidence amongst patients. This training approach should address knowledge barriers about capnography and its applications in improving the patient’s quality of care (Israel, 2014; Jaffe, 2017; Kuisma et al., 2017; Nassar & Schmidt, 2016). The strategic application of capnography is to improve patient care, and the paradigm shifts are often conflicted among nurses introduced to clinical monitoring tools such as capnography.
The major concern for healthcare practitioners is to minimize the negative impact created by the uncertainties and the lack of knowledge by nurses in using capnography. This relationship between nurses’ adoption of capnography, clinical uncertainty, lack of knowledge to use capnography in clinical settings, and its impact on patient care remains understudied (Kodali, 2013; Whitaker & Benson, 2016). Additionally, Sandroni, De Santis, and D’Arrigo (2018) argued that the lack of knowledge among users monitoring such as capnography could result in fatality.
The scholars also uncovered a gap in the literature pertaining to nursing practices in the use of this monitoring device to minimize medical errors in a clinical setting, as well as nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge for using capnography in a clinical setting. Further investigation, as described herein, could expand the understanding of the nurses’ role in adopting capnography and investigate the levels of clinical uncertainties resulting from the lack of device monitoring knowledge in the healthcare industry.
Problem Statement
It is not known to what degree the implementation of an evidence-based intervention impacts the use of capnography during CPR, when compared to current practice among adult ICU patients undergoing cardiopulmonary resuscitation in the ICU. Previous studies conducted by Hassankhani, Aghdam, Rahmani, and Mohammadpoorfard, (2015) and Kiekkas, Stefanopoulos, Konstantinou, Bakalis, and Aretha (2016) showed that nursing practice pertaining to the application of evidence-based technology such as capnography is essential in managing cardiac-related incidents.
In addition to the above mentioned studies, the perception exists that if nurses possess sufficient knowledge pertaining to the use of capnography during cardiopulmonary resuscitation (CPR), they can achieve better outcomes for the patient; especially in monitoring patients heart conditions and reducing risks of complications during a direct peritoneal resuscitation (DPR) (Hassankhani et al., 2015). The general clinical problem in nursing practice is the lack of knowledge about how to use new innovations such as capnography. Specifically, the clinical problem in this project is that managers do not understand the relationship between nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge to use capnography in a clinical setting.
To that extent, it is not apparent if or to what degree the implementation of an education and a standardized process for the use of capnography during CPR with nurses from a 20 bed ICU (8-10 bed capacity) at a 240-bed acute care hospital in New Jersey, would impact the rate of use of capnography during CPR when compared to current practice among patients undergoing cardiopulmonary resuscitation in the ICU. It is also not clear whether the nurses’ lack of knowledge impedes the application of capnography in clinical settings (Kiekkaset al., 2016). Therefore, these pressing questions will become the center of this project.
Purpose of the Project
The purpose of this quantitative, quasi-experimental pretest-posttest project is to determine to what degree the implementation of capnography during cardiopulmonary resuscitation (CPR) when compared to the current practice would impact nurses and increase use of capnography during CPR for adult ICU patients at an acute care hospital in New Jersey. The independent variable identified in this project is the intervention program designed to improve nurses’ knowledge of capnography use. The dependent variable is the number of instances of the use of capnography during resuscitation. The nurses practicing in the United States at clinical centers within or around New Jersey will be the target population for this project. The selected sample group will be appropriate for the project because of their clinical exposure to the use of capnography.
In examining the level of knowledge, this project will be focused on ascertaining the strength, vulnerabilities, and weaknesses specific to the nursing awareness about the use of capnography during cardiopulmonary resuscitation. Additionally, the author of the project will attempt to examine the correlation between such knowledge and the use of capnography during CPR and determine if any connections exist between nursing knowledge and their resistance against the use of capnography in the cases of CPR.
In addition to addressing the dearth or deficiencies in research on this topic as it pertains to the scholarly work and as well as the necessary insight for clinical managers, this project will also attempt to provide some understanding of the differences in the nursing knowledge in using capnography during cardiopulmonary resuscitation. Moreover, it will offer new information to achieve efficiency in the adoption of capnography in managing patients with CPR. The outcomes of this project include a positive clinical nursing practice change in which clinical managers use the results of the initiative to moderate nurses’ adoption of clinical devices in the hospital setting.
Clinical Question
The use of capnography by nurses is a strategic approach to achieving positive clinical outcomes. It has been discussed previously that the lack of knowledge and the inability of nurses to adopt innovation such as capnography can result in unintended consequences such as clinical uncertainties, medical error, and even patient fatality in a clinical setting. The central clinical question that guides this project is:
To what degree does implementation of an evidence-based intervention on use of capnography during cardiopulmonary resuscitation (CPR) impact use of capnography during CPR when compared to current practice, among adult ICU patients in an acute care hospital setting in New Jersey within a four-week period?
Advancing Scientific Knowledge
The outcome of the proposed project could contribute to the development of population health outcomes of patients suffering from cardiovascular diseases. This will be accomplished by the abilities of the investigator to provide clinical practice evidence pertaining to the results of the project and its effect on coronary care. The findings in the proposed quantitative pre-test post-test study could be used by clinical managers to moderate nursing practices in the adoption of new clinical devices such as capnography. Edelson et al. (2014), estimated that over 200,000 people suffer cardiac arrest annually, and more than 80% of them do not survive to discharge (p. 353). Kodali and Urman (2014), and Mader et al. (2014) found that thousands of people die from cardiac arrest in the United States every day. It appears from these numbers that cardiac arrest is a common problem the continues to affect various demographic populations in the United States. Thus, the proposed project is relevant and important to the current sphere of medical science.
Studies by Kiekkas (2016) and Lui, Poon, and Tsui (2016) advanced the knowledge for the use of capnography in the clinical settings to monitor and improve survival rates of cardiac-related incidents. However, the research outcomes surrounding the cases in which nurses lack the knowledge to use capnography have proven to be inconsistent, thus creating difficulties and uncertainties for targeted practice improvement measures (Dioso, 2014). To improve capnography practices in clinical settings, nurses and clinical managers must understand the relationship and importance of using capnography to improve patient outcomes. This project has the opportunity to close the gap in the information about nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge to use capnography in a clinical setting. It is also a contribution to the larger body of literature and application to nursing practices.
The theoretical foundation for the study will be based on the model of change introduced by Kurt Lewin in the 1940s. The author’s theory proposes that all change projects happen in three steps – unfreezing, moving, and refreezing (Lewis, 1951). Lewis (2003) further that each stage is invaluable, meaning that they all play a role in the new structure or objective becoming a part of the existing system. This theory implies that people are resistant to change, especially if they do not understand why it is necessary (Burnes & Bargal, 2017). Moreover, the process of a change’s introduction can be influenced by using the elements outlined in the “unfreeze” step.
Lewin’s (1952) view of change projects will provide a helpful concept to explain the processes and ideas relating to the adoption of new techniques, applications, and systems in varieties of organizational settings such as health care centers. In the case of nursing knowledge and capnography, this theory demonstrates that the complexity of an innovation and its compatibility with the existing system are crucial in the success of its implementation. Thus, the project that targets nursing training can use this approach to measure the correlation between knowledge and use of the procedure and provide insight into nurses’ changing attitudes towards capnography in CPR.
Significance of the Project
From current observation, it is not known whether increased nurses’ knowledge of capnography is associated with the increased use of capnography during cardiopulmonary resuscitation. The significance of the project lies primarily in addressing the inconsistent findings in the scholarly literature on capnography and nurses’ knowledge regarding its use during cardiopulmonary resuscitation (CPR) in the intensive care unit. The studies discussed above, including those by Kodali (2013) and Whitaker and Benson (2016), show that there exists a gap in understanding how nurses’ awareness of capnography affects their choice of using it during CPR. Furthermore, as evidenced by the analysis of current research, articles on capnography focus mostly on the outcomes and implementation of capnography within this healthcare setting (Kalmar et al., 2018; Langhan, Shabanova, Li, Bernstein, & Shapiro, 2015; Turle, Sherren, Nicholson, Callaghan, & Shepherd, 2015). To facilitate the effective use of capnography, it is essential to determine individual factors that impact nurses’ knowledge and the understanding behind the readiness to use capnography into practice.
This project aims to explore the link between nurses’ knowledge and the use of capnography during CPR further, thus providing the basis for further practice improvement and future scholarly work in this area. The results of this initiative could also lead to the improvement of practice approaches in capnography and an enhancement in the quality of patient outcomes in the intensive care unit setting. This project differs from other studies in the field of capnography use in terms of its focus, while it also builds on other research concerning the nurses’ perspectives on capnography and its importance in promoting successful patient outcomes (Lin et al., 2017; Novais &Moreira, 2015; Pantazopoulos et al., 2015).
Furthermore, the project fills in the gaps pertaining to the literature reviews on the topic by correlating them with the data provided by quantitative studies of capnography and the nurses’ knowledge of the topic as well as its application within the present intensive care unit setting. The critical implications of the project exist for a variety of stakeholders, including nurses, managers, patients, and the industry as a whole. The results of the data collected during this project’s duration rely on practice improvements in education and training. This, in turn, would contribute to population health by enhancing clinical practices in CPR and the improvement of capnography efforts within this setting. Also, it would decrease uncertainty during resuscitation procedures and practices that can stem from a lack of knowledge by nurses, reducing stress and promoting guideline compliance within the intensive care unit. Overall, the project would add value by providing information in support of nursing education and training in capnography, which would help to advance the practice and improve population health.
Rationale for Methodology
The quantitative method was chosen for this project due to its features in addressing clinical questions using the collection of meaningful information on the capnography use and nurses’ knowledge. In this quantitative methodology, data gathering will be the primary strategy for getting information from the project participants (Kiekkas et al., 2016). The quantitative method was considered for this project because the investigator needed to examine the relationships between individual factors affecting capnography use and nurses’ knowledge during cardiopulmonary resuscitation (CPR) practice in intensive care units. Quantitative methodologies have many benefits that are relevant to this project. They provide a high level of validity and certainty of results as they apply statistical tools for data gathering, organization, and analysis. (Ali & Bhaskar, 2016; Center for Innovation in Research and Teaching, 2013a; Heale & Twycross, 2015; Leppink et al., 2016; Watson, 2015). The use of the quantitative method in this project will be strategic in answering the formulated clinical question to clarify and provide some insight to underlying phenomena in the variables proposed in the study (Campbell, 2017; Center for Innovation in Research and Teaching, 2013b; Guo et al., 2016; Nelson, 2018).
The qualitative methodology will not be used in this project because it contains some limitations that could possibly influence and hinder the reliability of data findings. Qualitative methods are concerned with abstract concepts, and thus their ability to provide objective information is limited (Flick, 2018; Green & Thorogood2018). This is one of the core concepts behind their use and their limitations in understanding the participants’ behaviors and attitudes rather than specific activities, or knowledge levels can affect the results of the data (Austin & Sutton, 2014; Barnham, 2015; Flanagan, Greenfield, Coad, & Neilson, 2015; Gunnell, 2016). In addition, qualitative instruments are usually not checked for validity and reliability, which increases the risk of bias. This is partially due to the fact that qualitative studies allow for subjective collection and analysis of data in which the researcher is also a participant in the study (Katz-Buonincontro & Anderson, 2018; Rowley, 2014).
The use of a qualitative method would contradict the purpose of the project and affect the opportunity to use its results for practice improvement. Based on the information above, the chosen approach of a quantitative study proves to be more effective than its qualitative alternative at answering the selected clinical question. The central question posed for the project considers the participants’ level of knowledge and its connection to the use of capnography. By addressing the chosen question with quasi-experimental analysis, not only will the data provide the answers to address the gaps in the project’s design, but it will also address the questions into whether improvements in nursing knowledge in the use of capnography has any significance in influencing its use within the coronary care environment.
Nature of the Project Design
The quasi-experimental pre-test post-test analysis is selected as the primary design for this project. Pre-test post-test design is selected because it contains specific procedures that will be executed to align the project with its purpose and the identified clinical statements. The focus of the project is to assess the degree of capnography use in particular scenarios (CPR) by nurses, depending on their existing and acquired knowledge about the procedure. The clinical question introduces a connection between these two variables as well as the comparison between the outcome before and after the intervention, which leads one to propose their contest and correlation as the center of the project. Furthermore, the use of capnography is juxtaposed with the current practice, which further invites one to compare these variables and evaluate their interrelatedness with nursing education. This research design relies on quantitative data collection and analysis methods to examine the relationship between two or more variables (Ingham-Broomfield, 2014). The variables used in quasi-experimental research, such as nurses’ knowledge and the use of capnography, closely reflect the true experiences and perceptions of the participants in a study (Price, Jhangiani, Chiang, Leighton, & Cuttler, 2017).
The sample, according to the project’s questions, includes patients in the ICU of a hospital located in New Jersey. A sampling of the population in the project will require extracting of a subset from the general frame to be examined. It is vital for the participants to come from a unit where cardiopulmonary resuscitation (CPR) have occurred – the patients have to have experienced CPR in the unit. The sample size is based on the fact that the ICU usually has 20 licensed beds, but has been operating at an 8-10 bed capacity. There are 32 nurses working in the unit, which is necessary to know to prepare the educational program.
Structured questionnaires containing the selected survey instruments will be used for data collection in this project. First, some demographic data will be collected in order to create some features for grouping and the participants’ analysis, but no identifying data will be recorded for the project. Some data collection procedures that are necessary to address the clinical question include testing the nurse’s knowledge in the use of capnography in cardiopulmonary resuscitation procedures. These survey questions will be relevant to providing to answer the sub-questions framed in this project’s premise as well as its main purpose (Campbell, 2017; Kiekkas et al., 2016; Nelson, 2018).
Definition of Terms
This section provides a brief overview of the operational terms of the project:
- Capnograph. The instrument used to measure and display the amount of cardon dioxide in one’s breath (Kiekkas et al., 2016).
- Capnography. Capnography is a non-invasive technique to monitor the concentration of partial pressure of carbon dioxide (Kiekkas et al., 2016). It can aid the nurse in tracking the patient’s progress and support one’s decision-making during cardiopulmonary resuscitation.
- Cardiac arrest. This term is defined as “the cessation of cardiac mechanical activity confirmed by the absence of a detectable pulse, unresponsiveness, and apnea” (Tobi & Amadasun, 2015, p. 132). Cardiac arrest leads to the patient’s death if the appropriate care is not provided immediately, and this adverse outcome, as well as the tools aiding its solution, are the focus of the present project.
- Cardiopulmonary resuscitation (CPR). This term identifies the process of restoring the patient’s blood flow during a cardiac arrest using chest compression and artificial ventilation (Kodali & Urman, 2014). There are specific, detailed guidelines on how to perform cardiopulmonary resuscitation that provide the foundation on which the assessment of the nurses’ knowledge regarding this technique will be based in this project.
- Electronic Health Record (EHR). A digital version of a patient’s record that contains information about patients recorded and updated in real time (Lin et al., 2018). An EHR allows hospitals to collect, systematize, share, and use patient data for diagnosis and treatment.
- Pretest-posttest design. A type of quasi-experimental design, in which the dependent variable is measured before and after the independent variable is implemented (Valente & MacKinnon, 2017). This gap in examination allows one to see the impact of the intervention or treatment on the dependent variable.
Assumptions, Limitations, Delimitations
Assumptions. The following methodological assumptions were made as part of designing the project:
- The information gathered from the participants will reflect the overall situation in an ICU of a 240-bed hospital in New Jersey. Although the sample is small, and there may be individual differences among the participants, it is assumed that their attitudes and perspectives will match those of nurses working within a similar setting under similar situations. It is likely that the hospital has similar standards, training, and equipment available for its medical staff.
- The nurses selected for the project will have time to participate in the testing portion of the proposed clinical question. The chosen quantitative methodology implies that each participant will complete the NKCT (“Nurses’ Knowledge about Capnography Test”) chosen for testing nurses’ knowledge of capnography use (Kiekkas et al., 2016). This test will assess the nurses’ education and information retention on the subject and how they perceive the importance of this procedure within the clinical setting. Nurses have a busy schedule, but an expectation is that their participation in the project will help one to obtain the appropriate data and improve patient outcomes as a result.
Limitations. The project limitations are:
- The lack of funding prolongs the data collection process. Providing compensation to nurses for taking part in testing would increase the response rate and nurses’ willingness to participate in the project.
- The project’s question and methodology raise some ethical considerations. While conducting studies involving human subjects, scholars face many ethical challenges (Sanjari, Bahramnezhad, Fomani, Shoghi, & Cheraghi, 2014; Zyphur & Pierides, 2017). For example, it may not be possible to conduct observations or test participants as planned. Moreover, the issue of information privacy always exists in quantitative research where one’s results should not affect their career and organizational environment.
Delimitations. The proposed delimitations within this project are as follows:
- Institutional support for recruiting and testing participants is necessary. This type of help could help to improve nurses’ willingness to participate in the project and remove the obstacles to conducting observations.
- Contingency planning for ethical compliance in performing an analysis could help to identify potential ethical constraints and plan for using alternative tools or techniques if necessary.
Summary and Organization of the Remainder of the Project
Overall, cardiopulmonary resuscitation is an essential process in coronary care settings, and additional techniques could increase the chances of survival. As shown above, the rates of people suffering from cardiac arrest annually are high, while the rate of survivors is low (Edelson et al., 2014). Capnography proves to be a valuable addition to the standard CPR procedures in monitoring the patient’s condition and predicting adverse events (Hamrick et al., 2017; Heradstveit & Heltne, 2014; Kodali & Urman, 2014; Venkatesh & Keating, 2017). The examination of the available data reveals the need to explore the barriers to the consistent implementation of capnography use and its effects. Furthermore, the previous research also demonstrates the importance of examining the nurses’ knowledge and attitude toward capnography in CPR and their utilization of these concepts in practice. Some studies suggest that many nurses are hesitant to apply such techniques due to the lack of proper training and experience (Lin et al., 2017; Lin et al., 2015; Novais & Moreira, 2015; Pantazopoulos et al., 2015).
This topic has limited evidence in the works of literature and thus continues to create gaps in data on how nursing knowledge affects their readiness to use capnography while complying with standard procedures. The project aims to advance the knowledge in this area, and the insight gained could be useful for nurses in the improvement of patient outcomes and practice. This present DPI project will seek to address this problem by establishing the relationship between nurses’ knowledge, the use of capnography, and how they correlate into contributing to positive patient outcomes.
The literature review provided in Chapter Two will present an in-depth view of the barriers associated with capnography use as they relate to nurses’ knowledge through the examination of scholarly findings on the topic and its importance within the clinical setting. Chapter Three of the project will explore the selected quasi-experimental methodology for data collection and analysis. The data analysis will be documented in Chapter Four, which will also demonstrate the calculations of the study in visual form. Finally, Chapter 5 will provide a discussion of the project and consider its connection to the existing scholarship and practice environment.
Literature Review
Introduction
At the present time, capnography is applied as a monitoring tool in a variety of clinical settings, including the operating theater and intensive care units (ICUs). Its main purpose is to help nurses assess patients’ end-tidal carbon dioxide (ETCO2) levels (Conway et al., 2018). This information allows one to understand the efficiency of a person’s metabolic and respiratory functions while under medical care. Additionally, during cardiopulmonary resuscitation (CPR), capnography provides an evaluation of both the cardiac function and organ perfusion, allowing monitoring of the effect of CPR efforts and predictions regarding the restoration of spontaneous circulation (ROSC). The purpose of this quantitative project is to examine the application of capnography usage within the ICU setting during CPR and show how its application can impact patient outcomes and nursing practices when compared to current practice. Thus, the literature review’s main themes are concerned with the use of capnography, especially when performing CPR, nursing knowledge, and patient outcomes.
The present literature review considers the information from peer-reviewed journals, conference proceedings publications, and books gathered by the author, with the focus on research articles. Academic journals were the foundation of the project’s investigation, as their recent knowledge showed the current use of capnography as well as the aspects (weaknesses, strengths, and potential problems) of its introduction to the clinical sphere. The collected articles contained the analyses, debates, arguments, and discussions pertaining to contrasting and similar reviews relating to the use of capnography in a clinical setting.
After the introduction, the literature review offers a brief background into the use of capnography in clinical settings. This part shows the information on the procedures’ history, the evolution of the question posed in this project as well as potential gaps in the literature identified in the scholarship. Then, the review of the literature offers several sections and subsections in which the selected articles were divided. The topics (sections) discussed in this project include:
- the use of capnography in different settings and relevant protocols;
- the effect of various capnography measurement models on patient outcomes;
- the impact of nurses’ knowledge on patient outcomes;
- the connection between nurses’ knowledge and improvement of practice;
- the correlation between CPR and capnography application;
- the perception of capnography application during CPR.
These topics offer an academic, logical, and rational discussion of reviews on nurses’ use of capnography as part of clinical practice in relation to patient management during cardiopulmonary resuscitation. They include subsections that discuss alternatives to capnography, nurses’ attitudes to CPR and capnography, and the impact of change on nurses and patient outcomes.
The search for the appropriate studies included in this review involved the author’s ability to search using key words such as capnography, resuscitation, cardiopulmonary, resuscitation, innovation, clinical setting, cardiac. These key words were utilized when searching through several databases, including but not limited to Elsevier, NCBI, and PubMed, and ProQuest Central. Prior to being selected, all articles were appraised according to their relevance to the project’s topic, date of publication, clinical question(s), methodology, quality of evidence, and limitations acknowledged by the investigators. The online library offers capabilities that increase one’s access to recent studies from many institutions and research centers.
The understanding of capnography invention, its initial use, and current trends help enhance the knowledge of the implications of its application and the prospects for the future development of capnography. From a historical perspective, capnography is a relatively new approach to evaluating a patient’s health state. The introduction of capnography to the clinical setting in the United States occurred in 1978, and registered nurses began using this tool in recent years to aid patient care (Harper, 2005). However, capnography as an instrument was developed in the 20th century, indicating a long history of using capnography in medicine. Hence, one can see the early onset of the problem of the uses that capnography can have in medical care.
One of the main issues considered in literature is the use of capnography in emergency and nonemergency situations as well as different units of the hospital. Wright (2017) argues that although capnography has been used in the clinical setting for many years, the actual use of this approach was limited. Anesthesia procedures and the practice of using capnography instruments for monitoring cardiac attacks have gained attention in its application in the healthcare setting. Gravenstein, Jaffe, Gravenstein, and Paulus (2011) state that capnography can be used to measure CO2 levels, metabolism, circulation, and other useful metrics, providing an extensive assessment of a patient’s well-being that is useful not only in emergency care but also in day to day monitoring of patients. Therefore, capnography as a monitoring tool provides medical personnel with a better understanding of patient health state because the interpretation of waveforms can serve more purposes than that of the measurement of ETCO2. This DPI project hopes to share a light on this statement, strengthening the argument that capnography’s uses are wide in the ICU.
Theoretical Foundations
The theoretical foundation of the present project is Lewin’s change theory. Originally introduced by Kurt Lewin in the 1940s, the model is still used by businesses and other organizations to this day. It is an approach to change that is based on three main stages: unfreeze, change, and refreeze (Lewin, 1951). Each of these steps contains a list of specific actions that aim to lower participants’ resistance to change and increase its chance of becoming the new standard. The first stage, unfreezing, implies that the current order of operation has to be uprooted in order to introduce new objectives. Here, the change is to be viewed as necessary – the organizational beliefs can be challenged with evidence, information dissemination, planning, and refocusing (Morse, 2017). Next, the step of changing involves all processes that are needed to institute the new order in the place of the old status quo. Here, the evidence transforms into the project, and its elements are completed to create the new system. Finally, the refreezing stage ensures that people continue to embrace change and that any problems are addressed timely.
The seminal work by Lewin that describes these steps and outlines them in detail was published in 1951, after his passing. In it, the author introduces the stages and discusses the importance of them, showing how unfreezing and refreezing affect the attitude of involved persons towards change. Many contemporary researchers analyze the change model and show how it is still relevant to management. Burnes (2004) and Cummings, Bridgman, and Brown (2016) consider this model one of the most valuable business and management theories that were ever created. They note that Lewin’s change model has roots in both psychological and business ideologies, acknowledging people’s resistance to new information and change and devising approaches that address this barrier. Hussain et al. (2018) and Burnes and Bargal (2017) show that the simplistic formula of three steps can be questioned, but its role in innovation is valuable for all industries and spheres where employees play a significant role in the success of the system.
Lewin’s model of change was chosen as a theoretic foundation for this project due to the abundance of medical research using this approach and their results in its implementation. According to Udod and Wagner (2018), this approach is widely used in healthcare. Its use of steps and the view of employees as vital members of the process can help nurses to adjust to the new procedure. Capnography is the tool that is known among nurses, but its use can be limited due to the staff’s knowledge and perception (Kaminska, Wieczorek, Dabrowski, Nadolny, & Smereka, 2018). The clinical question posed in this research looks at how this barrier can impact patient outcomes and how new practice can lead to positive results. Thus, as change burdened by negative perceptions lies at the core of this project, Lewin’s change model appears to be the most suitable theory to achieve results.
Review of the Literature
The complications connected to varied airway events often occur outside the operating theater and result in high mortality rates. Kerslake and Kelly (2016) state that in around 70% of explored cases application of capnography would help mitigate the adverse impact of airway complications or prevent deaths of patients. These statistics are valid for patients dependent on artificial airway support. In addition, capnography application in ICU units can provide valuable input in monitoring ETCO2 levels during resuscitation. The following subsections will examine the evidence suggesting the necessity of utilizing capnography during CPR and the current evidence relating to nurses’ knowledge of this instrument as well as data relating to its application.
Capnography and alternatives in resuscitation. In the United States, the American Heart Association advises on using capnography during CPR (“2015 international guidelines on CPR,” 2015). In Europe, the NAP4 guidelines, which are published for medical institutions both in Europe and the United Kingdom, use of capnography is obligatory for patients subjected to anesthesia, regardless of the devices used for airway support (Kerslake & Kelly, 2016; Soar et al., 2015; Link et al., 2015). Additionally, patients receiving advanced life support should also receive continuous capnography monitoring to detect any life-threatening changes. While this suggests that capnography can be helpful in preventing mortality or airway complications in patients within varied clinical settings, the use of capnography during resuscitation procedures is the topic that requires additional exploration.
The history of capnography in resuscitation. Capnography, as an instrument, has been applied in medical settings for over forty years. At first, it was applied for patients under anesthesia – to monitor their coronary condition in the sedated state (Kalenda, 1978). In Holland, it became a standard of safety in the middle of the 20th century. Nevertheless, the use of capnography during CPR remained under question, and it continues to be a center of debate in the medical field. As the present studies show, the evidence that supports the use of capnography during CPR has been published since 1978, and some of the most recent articles show similar findings in 2018.
The first use of capnography during resuscitation. The first article describing the application of this monitoring tool in a clinical setting, more specifically during resuscitation, was published by Kalenda (1978). In it, the author suggests that monitoring pulmonary perfusion during cardiac massage performed for patient resuscitation can enhance the outcomes. The patient cases presented by Kalenda (1978) suggest that changing resuscitating strategies reduces patient mortality rates. This article shows that the presence of a capnography tool allows nurses to control the process more accurately and adjust the cardiac massage as necessary, affecting the efficiency of the resuscitation efforts.
Capnography as a source of data for CPR. Similar to the evidence presented by Kalenda (1978), more recent literature such as the article by Hartmann et al. (2015), suggests that applying capnography during resuscitation helps decrease mortality rates. Hartmann et al. (2015) present a systematic review and meta-analysis of the evidence showing what role ETCO2 measurements play in CPR. Their review considers 27 studies and finds that the transparency offered by capnography allows nurses to see the threshold for ETCO2 goals during resuscitation. This analysis reveals the important place of capnography in supporting the success of CPR and patient outcomes.
Capnogram-based ventilation detection in CPR. The article by Gutiérrez et al. (2018) explores how capnography use during CPR can be enhanced to report more reliable data. In this text, one can see that the positive impact of capnography is undisputed. The authors collect cardiac arrest defibrillator recordings with capnograms and compare the performance of algorithms with and without a filter for capnography. They find a way to make capnography show more accurate data to increase positive patient outcomes, further arguing that capnography is a valuable tool for the procedure of resuscitation. It should be noted that other studies such as the one by Lampe (2017) also advocate for improving the process of monitoring ventilation using capnography.
Alternatives to capnography and their limitations. Capnography is not the only method for evaluating these vital signs, but it is more efficient when compared to others, which impacts the quality of care and is especially crucial during CPR, where timing and efficiency of actions can affect the likelihood of survival. According to Gravenstein et al. (2011), capnography is “the continuous recording of CO2 partial pressure [pp] in inspiratory and expiratory gases” (p. 418). A similar method titled capnometry exists; however, it does not provide an opportunity to monitor a patient’s CO2 levels, instead of giving a numerical assessment at a given point in time.
Old and new studies review the use of this tool during resuscitation efforts, consistently finding that the information capnography provides to nurses is invaluable to their knowledge about the patient’s coronary health as well as their chances for success. Thus, research from the last five decades shows that capnography should be an integral part of the ICU setting (Gutiérrez et al., 2018; Hartmann et al., 2015; Kalenda, 1978). The history of capnography reviewed with the help of these articles support the place of capnography in the ICU and situations outside of the usual use during anesthesia.
Different uses of capnography. The history of capnography shows that this tool has been widely used in a variety of medical spheres. It is essential for many areas outside of resuscitation, and its first creation did not intend for this instrument to be utilized in the way the present topic considers. Nonetheless, with time, capnography also gained recognition in several sphere, including emergency situations and resuscitation.
Capnography outside of resuscitation. Examining the scholarly articles on the topic of capnography for other emergencies and non-emergency situations in the hospital setting can help evaluate the current best practices using evidence-based suggestions and understand the methodology and specifics of the chosen approach. While the discussed literature analyzes the utilization of capnography in various settings, further research can help improve the application of this tool in a clinical setting during CPR. The following articles demonstrate the broad scope of areas to which capnography is a valuable addition.
Capnography and anesthesia. In general, capnography is helpful in the operating theatre during anesthesia; this non-operative practice allows the monitoring of patients. According to Pantazopulus et al. (2015), “low ETCO2 levels may indicate hyperventilation, apnea, esophageal intubation, occlusion of the endotracheal tube, leakage in the ventilation system, poor systemic and pulmonary circulation, hypothermia, massive pulmonary embolism, or ineffective chest compressions” (p. 1053). The systematic literature review conducted by the authors outlines two main themes connected to the application of this tool exist – implementation and interpretation of results. The latter is especially relevant for the issue of resuscitation because a nurse or other medical professional has to be capable to quickly assess and interpret the results of monitoring to adjust resuscitation or change the inhalation tubes for patients. The use of capnography in ICU resuscitation can improve the number of successful patient cases. However, filtering practices allowing medical personnel to receive reliable results from capnography tools must be implemented since fast oscillations connected to chest compressions can obstruct the resuscitation.
Opioid-induced respiratory issues and capnography. A study by Stites, Surprise, McNiel, Northrop, and De Ruyter (2017) revealed that capnography could reduce the number of opioid-induced respiratory issues. The clinical setting observed by the authors implemented the utilization of capnography, and the outcomes suggest a statistically significant improvement in the PCA efforts. The methodology used by the authors of the explored studies suggests that short-term cohort research is the best practice for approaching the issue. Most researchers explored evidence by examining patient records, implying that retrospective studies are conventional approaches to discussing this topic.
Respiratory depression and capnography. Langham, Li, and Lichtor (2016) consider capnography outside of anesthesia and suggest that children should be monitored using this tool to detect hypoventilation and apnea, which is also supported by Subramani et al. (2017). In this case, the cross-sectional study demonstrates the broad application of capnography and its ability to monitor patients whose health is not directly related to anesthesia. The authors find that routine monitoring can improve patient health, thus showing that capnography has many uses, including those in the ICU.
Capnography and metabolic changes. Cereceda-Sánchez and Molina-Mula (2017) reviewed the prospects of using capnography in the ED setting for detecting metabolic changes in patients. Since the article is a systemic literature review, the methodology that the authors used involved an examination of 17 studies focusing on the specifics of capnography. The findings suggest that this tool is efficient and cost-effective, which further promotes the need to develop and implement strategies promoting the use of it in the hospital setting.
Capnography allows monitoring the concentration of the carbon dioxide (CO2) in the respiratory gases of the patient. In medicine, this tool is currently used during anesthesia or in intensive care units, while some new studies suggest that using capnography ICU can improve patient outcomes. Capnography allows the medical personnel to monitor the inhaled and exhaled gases. Another benefit of this approach is that it presents an indirect assessment of the patient’s partial pressure in the arterial blood. The importance of using capnography not only in the operating theatre but also in resuscitation or other emergencies is connected to its ability to detect airways complications in patients.
Capnography and resuscitation. The general theme of the literature is that capnography has a statistically significant impact on patient outcomes in many areas, including during CPR. The present studies show why capnography is invaluable during resuscitation. Some of them also introduce this tool to improve the outcomes of CPR and lower the risks related to it. A specific practice problem is the impact of nurses’ knowledge on the practice of using capnography in ICU during CPR. Hence, the topic of this paper is practice improvement that will help nurses use capnography tools and interpret results for adjusting resuscitating efforts in the ICU.
Capnography in critical care. While capnography is not the only approach to measuring CO2 levels in a clinical setting, it is the most efficient and accurate. It improves the nurse’s ability to diagnose respiratory issues and mitigate them, which is especially crucial during CPR. The main principle of capnography tools’ work is the evaluation of CO2 levels, which is useful in determining the production of CO2, lung perfusion, patient’s respiratory patterns, and alveolar ventilation. The capnometer measures the CO2 concentrations using a gas sample collected from a patient (Kerslake & Kelly, 2016). Capnography trace or waveform is the graphic representation of results with time and partial CO2 pressure displayed on X and Y-axes. Hence, the authors conclude that the continuous monitoring that this instrument provides is vital in the context of the CPR set.
Capnography for death prevention. Cook and Garrop-Griffinth (2019) argue that the utilization of capnography in the varied clinical setting can serve as a measure for preventing deaths. The authors base their conclusions on a study of contemporary practices applied in hospitals. The results suggest that a large percentage of individuals are dying due to misplaced tubes or esophageal intubation, which can be prevented by using capnography. The common reasons cited by the authors are the failure to use capnography and the lack of education about this tool that would allow medical personnel to use it in case of emergencies.
Capnography and out-of-hospital cardiac arrest. Lui et al. (2016) consider the value of accumulating data about ETCO2 during patient resuscitation in out-of-hospital cardiac arrest cases. The authors perform a cross-sectional study of adults and find that the information that capnography provides can diagnose cardiac arrest and help nurses to determine the patient’s state. Their findings align with those of Elola et al. (2019), Sheak et al. (2015) and Gong, Lu, Zhang, Zhang, and Li (2015). This study shows how one’s knowledge of circulation can help with CPR and notes that capnography is essential in such procedures, further strengthening the place of this tool in resuscitation efforts.
Capnography for reducing chest compression. Capnography can be used to reduce chest compressions when resuscitating patients. This methodology was developed by Leturiondo et al. (2019) and Merckx, Lambert, Cantineau, and Duvaidestin (1992) and incorporated capnography-based chest monitoring tailored for the purposes of cardiopulmonary resuscitation. The issue with the approach currently used in medical establishments is that chest compressions affect the accuracy of automated ventilation detection, which can endanger the patient. Leturiondo et al. (2018) developed an algorithm that considers this issue and allows detecting insufficiencies in patient ventilation. Hence, the accuracy of results and reliability of capnography affects the outcomes of resuscitation efforts (Ruiz de Gauna et al., 2018). This methodology suggests that while applying capnography during resuscitation helps improve the patient state, more developments, and evidence-based research is required to develop practice improvements.
Potential barriers to using capnography in CPR. Capnography has solidified itself as a preventative measure in accessing CO2 levels, but its use within these types for CPR should be researched further. De Caen and Maconochie (2018) argue that “recent systematic reviews suggest, however, that using specific EtCO2 values to guide patient care during adult cardiac arrest is based upon low-quality evidence” (p. 2). Hence, the lack of high-quality literature and reliable data regarding cut-offs and respiratory patterns measured with capnography can explain why the perception of this technique and its use by nurses during CPR is insufficient. Regarding outcome predictions, several studies suggest that capnography can be applied when determining the patient’s state upon CPR.
Current application of capnography. It is also necessary to understand that nurses in different departments can use capnography, and the decision-making process should incorporate a variety of patient-related factors. Bullock, Dodington, Donoghue, and Langhan (2017) examine patient cases of resuscitation in a pediatric department to identify whether the guidelines by the American Heart Association (AHA) in 2010 are applicable and the specifics of utilizing capnography depending on patient characteristics. The research methodology involved a retrospective review of charts assessing data such as trauma, sex, age, capnography results, and patient outcomes. The conclusions suggest that the use of capnography in CPR procedures is inadequate since it was applied in only 13% of cases (Bullock et al., 2017). Moreover, the case reports indicate that individuals who had CPR with capnography were more prone to have a spontaneous circulation in comparison to patients not receiving it. The overall duration of CPR procedures was longer in cases with applied capnography, suggesting that this instrument improves the accuracy of patient prognosis. This study contributes to the posed clinical question as it highlights the benefits of capnography and the lack of its proper application in hospitals.
As a result, the present studies show how capnography can prevent avoidable deaths due to unsuccessful resuscitation. According to Cook and Garrop-Griffin (2019), “expired carbon dioxide is routinely detectable during the management of patients with recent cardiac arrest, even in the absence of chest compressions” (p. 439). This evidence provides support for the use of capnography in the ICU. It also raises the question of why this topic is still the subject of debate and presents some inquiries into nurses’ perception of capnography as a valuable instrument during CPR.
Nursing knowledge and patient outcomes. Education of medical personnel regarding capnography use and the interpretation of results has an impact on the use of this tool. While capnography has been used in a clinical setting for almost fifty years, some literature findings suggest the need to dedicate more attention towards educating medical personnel to use this method appropriately for monitoring a patient’s health state and detecting possible heart failure (Langham, Li, & Lichtor, 2017; Long, Koyfman, & Vivirito, 2017). This is a vital component that helps ensure that medical professionals can interpret the capnography traces adequately (Kerslake & Kelly, 2016). Another aspect is the attitudes and perception of nurses that may view capnography as an unnecessary tool that impedes rather than assists their performance.
Nurses’ knowledge about capnography and other procedures. Nurses and factors relating to their work have a direct impact on patient outcomes, and improvement of practice approaches or hospital environment can enhance health-related metrics in patients. This idea suggests that a variety of factors, including the availability of capnography tools, is hospitals, skills that allow nurses to use and interpret waveforms, personnel perceptions of the technique, and the overall attitude of a healthcare organization can affect the practice of using capnography in the ICU (Jaffe, 2017; Darocha et al., 2017). The methodology used in studies by Gong et al. (2015), Chhajed, et al. (2017), Darocha et al. (2017), is a mixed design, incorporating a qualitative assessment of nurses’ opinions, hospital managers perception of capnography, and quantitative analysis of patient data. The literature findings relating to these issues allow designing a questionnaire that will account for all aspects that obstruct or facilitate the utilization of capnography by nurses, making this DPI more comprehensive.
Nursing knowledge and patient survival outcomes. Assessment of death associated with failure to apply tools such as capnography can provide an insight into the severer of the problem. Pantazopoulos et al. (2015) argue that only 20% of patients that receive resuscitation survive, despite the recent advancements in the techniques and technology application used to monitor the process and improve the outcomes. Moreover, in the setting outside the hospital, the statistics suggest a survival rate of only 10% (Pantazopoulos et al., 2015). Hence, determining the issues that contribute to the high mortality and possible best practices to help reduce the number of adverse incidents can help design guidelines for medical practitioners. One aspect is the application of capnography, which provides continuous monitoring of the patient’s respiratory system and helps to prevent or reduce the risk of emergency situations.
Nursing training and capnography. The ability to apply capnography is also affected by the technical expertise that enables using innovational instruments and tools, and it is essential to ensure that nurses possess sufficient knowledge to implement capnography in the critical care unit. Wright (2017) notes that “with overwhelming lack of proper training related to new technology devices such capnography, a sound developmental training program regarding the use of capnography can positively affect patient safety and outcomes” (p. 10). The author shows that training is an essential aspect in developing improvement practice suggestions since the ability to use the capnography is crucial for adequate measurement of CO2 levels and adjustment of resuscitation strategies in accordance with this assessment.
Training and quality of work using capnography. Saunders, Struya, Pollock, Mestek, and Lightdale (2017) focus on the correlation between education or training and the quality of work displayed by nurses when they use capnography in a hospital setting. Although they do not use this tool during resuscitation in the study’s case, nurses’ training with the instrument impacts their ability to help patients and lower the need for assisted ventilation, according to the findings of the study (Saunders et al., 2017). Thus, one can see how such an aspect as training has clinical value and can impact patient outcomes, and it is suggested to develop and implement education programs that target this problem in CPR.
Implications of capnography in medicine. According to Aramendi et al. (2017), “capnography permits monitoring ventilation, but the chest compressions provided during CPR corrupt the capnogram and compromised the accuracy of automatic ventilation detectors” (p. 41). The authors explored 83 episodes of cardiac arrest both in the hospital setting and outside the clinical setting, to determine the best practices for using capnography in resuscitation. The findings suggest that an approach using only a capnography tool can be a valid strategy in the resuscitation process. The explored evidence suggests that practice improvement guidelines should incorporate strategies for educating and training medical personnel to use capnography in emergencies, for instance, when resuscitating a patient in an ICU unit.
Supplemental training to facilitate capnography use. As was previously mentioned, some researchers point out that the use of capnography, as a part of CPR, requires additional attention because the waveform can be distorted by chest compressions, indicating a need for additional training required for nurses working in ICUs. Leturiondo et al. (2018) state that over 70% of waveforms examined in their study was distorted because of resuscitation efforts. This requires the development of an algorithm specially tailored towards CPR that would mitigate the impact of chest compressions on capnography results, minimizing the distortion. The focus of capnography application during resuscitation efforts is on determining whether the endotracheal tube was placed correctly, ensuring that the performed chest compressions are done correctly, and detecting ROSC. Additionally, Leturiondo et al. (2018) argue that capnography can be utilized to develop a prognosis for patients. Ventilation rate monitoring is essential during CPR because it helps nurses detect hyperventilation and prevent adverse patient events.
Distortion of the breathing patterns. In this study, Ristagno et al. (2015) inspect data from 1617 patients with ventricular fibrillation and find that, in general, visual inspection of the waveform is enough for tracking breathing patterns of individuals. The reliability of results produced through capnography during CRP can be questioned because of distortion, and it is necessary to conduct further research. This article presents some potential risks of using capnography without sufficient training, explaining the potential hesitation of nurses towards this change project, and laying some ground for the first step of the intervention.
This theme was explored because the goal of this DPI project is to explore the relationships between nurses’ knowledge about capnography and its application to the number of adverse outcomes in the ICU. Therefore, the relationship between factors that impact a nurse’s work and professional qualities such as education or skills should be explored to determine the significance of this aspect. While alternative approaches to the issue may suggest that quality of care is facilitated only by the specifics of nurse training, it is evident that other factors contribute to this aspect as well.
Specific protocols for using capnography. Although capnography as an instrument is not difficult to apply in a clinical setting because it is non-invasive and requires only the presence of capnography and a medical professional capable of interpreting the results, there a variety of algorithms and strategies for using this instrument which complicates nursing training. Guidelines for using capnography can influence the ways nurses use this tool, and the following articles explore this connection.
Resuscitation-specific capnography utilization. Capnography is a valuable tool that allows for enhancing the process of monitoring a patient’s respiratory function in an emergency scenario, making it relevant during resuscitation attempts. Examination of the capnography in the emergency department helps outline the basis for interview topics that will be applied for this project. While many studies considered above review the place of capnography in the process of resuscitation, and some guidelines recommend this tool, scholars continue to explore the aspects of this procedure and its application in the ICU.
Guidelines for the application of capnography. Haines (2017) examined guidelines and practices used in emergency departments (ED) to provide a qualitative assessment of the capnography application and its benefits. Patients in the EDs are at high risk of developing complications because of respiratory function impairment. Thus, the information from this study helps improve the DPI by providing explanations of the application and possible reasoning that explains why this instrument is underused in the United States hospitals. Haines’ (2017) findings are complicit with those of other authors arguing that capnography is beneficial during CPR since it allows the medical personnel to provide continuous chest compressions without a need to check the patient’s pulse.
Different outcomes of capnography. Research shows that capnography is more efficient when compared to other respiratory monitoring techniques. For instance, pulse oximetry can be used to detect hypoxia, but the results are not produced continuously (Haines, 2017). Capnography is a non-invasive technique that does not require additional preparations for use, but one should consider different instruments and their appropriateness within the ICU setting. Moreover, the authors considers the variety of method for capnography use.
Two main models of capnography. According to Kellshake and Kelly (2016), currently, two models of applying capnography tools and measuring the CO2 levels exist. The first one is a side stream analyzer, which implies taking a sample of gas from the patient’s respiratory tube and placing it in the humidifier filter. This approach is applied in a setting for non-intubated patients because it is more comfortable, and the equipment required for analysis is less bulky when compared to the other two methods. Mainstream analyzers use infrared light that scans the ventilation circuit. This method is more suitable for monitoring patients during resuscitation.
Combining capnography and other tools. Some researchers explored the different combinations of tools and techniques to develop the best practice of applying capnography, which can be used in practice improvement. Salen et al. (2001) explored the possibility of combining capnography tools with a cardiac sonographer in order to improve the procedure of patient resuscitation. The objective was to measure the accuracy of predicting resuscitation outcomes using the two instruments in the emergency department (ED). The combination did not provide significant improvements, but capnography was shown to be a major predictor of survival (Salen et al., 2001). Thus, its use in resuscitation is supported further by this research.
Overall, there exists an abundance of research that shows how capnography helps during resuscitation. However, many studies also note the difficulties related to this procedure – while it is non-invasive, it requires sufficient experience and knowledge from nurses to produce successful outcomes. From this idea, another subtheme emerges – the necessity of education for nurses to improve the use of capnography in the ICU, namely during resuscitation.
Education to widen capnography use. The focus of this practice improvement project is on intensive care units and resuscitation, but the overview of history suggests that capnography is applied in other hospital units, that have established standard guidelines for using capnography in a clinical setting. In general, capnography is usually utilized during anesthesia to monitor a patient’s respiratory function. Only in recent years, researches and practitioners began exploring the implications and benefits of using this monitoring tool in other hospital units, as shown above. This contributes to the understanding of the specific information that this DPI should investigate.
Patient selection for capnography. First of all, there exists a conversation about which patients can be subjected to capnography. Kerslake and Kelly (2016) state that “capnography can be used both for intubated and non-intubated patients” (p. 178). The diversity of metrics that can be assessed using capnography presents an understanding of the need to dedicate special attention to educating medical personnel about how and when to use capnography and how to interpret the results. According to Kershake and Kelly (2016), capnography “can be used to detect displaced tracheal tubes and tracheostomy tubes and to diagnose inadvertent esophageal intubation” (p. 178). Additionally, the authors argue that this method can be applied to monitor the cardiovascular functions of a human’s body.
Automated monitoring to overcome chest compression. Turle, Sherren, Nicholson, Callaghan, and Shepherd (2015) suggest applying automated respiratory monitoring with specific algorithms that help disregard the impact of chest compressions of capnography results. Their methodology, questionnaires and telephone conversations, informs the approach chosen for this DPI. Out of 211 establishments, only four did not have the equipment necessary to conduct capnography assessment, and only 50% of respondents stated that capnography was used to measure the efficiency of CPR (Turle et al., 2015). These findings indicate the inefficiency of use connected to capnography utilization in the United Kingdom hospitals. In addition, this study suggests that most establishments lacked the necessary equipment to perform the measurement in general wards. Arguably, the application of such a strategy would require an even more in-depth knowledge of technology from nurses who would use this instrument in their practice during CPRs.
Reading capnography results. Nurses’ ability to accurately identify patterns and interpret waveform results can help in preventing adverse respiratory events. Pantazopoulos et al. (2015) state that “airway management, compression depth and chest recoil, hands-off time, and early defibrillation” are the critical measurements that capnography helps assess (p. 1053). Airway management is the primary emphasis of this study since it can be used to adjust other elements of resuscitation efforts. However, Pantazopoulos et al. (2015) suggest that current guidelines on monitoring the CO2 levels in a patient gas sample lack clarity and require further examination to develop best practices. Monitoring end-tidal CO2 is used, which involves evaluating the pressure upon exhale. Hence, the importance of the topic discussed in this project is highlighted by this research because explored evidence suggests that a large number of healthcare professionals lack an understanding of how capnography can improve patient care during resuscitation and affect mortality rates.
Nurses’ use of capnography readings. Zito, Berardinelli, Butler, Morrison, and Albert (2019) focused their attention on how nurses use capnography results to make decisions regarding patient discharges, using confidence levels assessment. This cross-sectional study observed 133 patients before and after ETCO2 assessments and measured nurses’ perception of the patient’s readiness for discharge. In the study, it is evident that nurses change their prognosis based on the outcomes of ETCO2 levels assessment. As was previously mentioned, despite the fact that capnography is mainly applied in the operating theater, most cases of airway complications occur outside this setting. Hence, there exists a need to evaluate the number of such cases and the readiness of nurses to apply capnography in the ICU unit.
Nurses’ Knowledge about Capnography Test (NKCT). An essential aspect of this project is the ability to accurately assess and measure nurses’ knowledge of capnography use in the CUU setting to be able to compare the two variables. Kiekkas et al. (2016) developed a questionnaire that allows accomplishing this goal titled Nurses’ Knowledge about Capnography Test (NKCT). The questions incorporated in this assessment aim to evaluate the understanding of capnography functions, aspects of end-tidal CO2 levels, waveform interpretation, and specifics of using capnography in a clinical setting.
This paper focuses explicitly on emergencies and the prospects of using capnography to improve patient outcomes. The literature suggests that capnography can significantly improve the current practices of resuscitation and CPR. According to the European Resuscitation Council, capnography use enables the detection of ROSC “without pausing continuous chest compressions thereby improving quality of resuscitation and preventing the potential harm caused by administering a further bolus of adrenaline after ROSC” (as cited in Kerslake & Kelly, 2017, p. 180). Therefore, nurses must possess the knowledge regarding capnography in resuscitation and the ability to recognize vital signs associated with ROSC.
Barriers to using capnography during resuscitation. As noted above, the complexity of using capnography outside of its usual setting is based not only on the tool itself or its availability in the hospital, but also nurses’ hesitance in following new evidence and recommendations. While American and international guidelines mention capnography as a valuable addition to the process of resuscitation, the number of cases where it is used remains low (Aramendi et al., 2017). Therefore, one has to look at possible barriers to capnography use outside of resource unavailability and the lack of value.
Improper waveform interpretation. According to Aramendi et al. (2018), capnography use is challenging as not all nurses can see the exact differences between breaths and chest compressions. The researchers were able to develop algorithms that allow medical personnel to use programs in a more advanced way, more specifically, for determining the location of ventilation. This study has several implications for the project; it implies the need to improve their current knowledge by providing them with the described algorithm. This can help enhance nurses’ confidence in using the technique as well. Additionally, this improves the CRP process in general by mitigating risks of hyperventilation, which is often associated with adverse patient outcomes.
Low adherence to clinical guidelines. Nassar and Kerber (2017) argue that despite the significant prevalence of poor outcomes associated with CPR and a large volume of evidence-based research providing guidelines regarding best practices within this domain, the adherence to these suggestions in clinical settings remains low. Nassar and Kerber (2017) state that “feedback devices provide instantaneous guidance to the rescuer, improve rescuer technique, and could impact patient outcomes” (p. 1061). The authors use a systematic review and list several elements that contribute to the improvement of CPR practices. They state that capnography is a critical aspect in monitoring chest compression and tracking the return of spontaneous circulation. This suggestion supports the primary claim of this DPI and highlights the need to determine what factors impact the lack of capnography application during CPR and develop interventions that can address these problems.
Perception of capnography application during CPR. The previous study suggests that the prevalence of capnography use among nurses use during CPR remains low. However, it is possible that other factors, apart from knowledge and perception, obstruct the adoption of this respiration-monitoring tool. Sahyoun, Siliciano, and Kessler (2018) developed a questionnaire for hospital managers to examine whether the hospitals in New York had equipment that would allow them to use capnography during resuscitation. Sahyoun et al. (2018) state that 95% of the respondents had the devices that allow their personnel monitoring ETCO2, and 97% implemented a protocol for applying them. However, only 54% reported having a protocol tailored explicitly for CPR, which is consistent with the findings of studies by Dioso (2017) and other studies mentioned in this review. Thus, despite the availability of capnography, hospital personnel may have difficulty applying these tools because no protocol or guideline that would help them is in place.
The absence of a protocol. One can argue that the lack of guidelines and efforts dedicated to ensuring that hospitals use capnography harms patients when those efforts are not consistent. Carlisle (2015) aimed to develop a standardized protocol for using capnography during resuscitation for opioid-induced respiratory depression (OIRD). This article explicitly targets nurses and their ability to use the tool during CPR. The author also notes the absence of education as a problem for nurses’ resistance to using the guidelines.
The lack of education. Hassankhani, Aghdam, Rahmani, and Mohammadpoorfard (2015) cites education as a vital factor for promoting the utilization of capnography in a clinical setting. The findings are based on the nurse interviews regarding the application of the protocol, and the answers suggest that issues are connected not only to the availability of devices and to the system issues and the lack of patient adherence.
The need for additional training. Whitaker and Benson (2016) indicate that approximately 74% of deaths in intensive care units (ICU) can be prevented if capnography monitoring is implemented as standard practice. The primary goal of this strategy is to improve patient safety; hence, the authors also recommend using a standardized protocol and providing nurses with additional training that would fill the gaps in knowledge and understanding of the interpretation of capnography.
In-depth knowledge of waveforms and distortions. Kodali and Urman (2014) suggest that universal application this tool during CPR will allow creating a database of waveforms that can be utilized to improve the existing protocols. Hence, the promotion of using this methodology will help further enhance the practice. Kodali and Urman (2014) conducted a literature search to locate evidence supporting the benefits of capnography in resuscitation published from 1960 and concluded that historically the interpretation of outcomes and attitudes regarding the predictions and evaluating that can be made using this approach changed since it is accepted that the “presence of small obtunded CO2 waveforms during CPR reinforces tracheal location of an endotracheal tube” (p. 332). In general, capnography use during resuscitation requires the knowledge of not only waveform interpretation, but also the understanding of distortions caused by CPR. The complexity of using capnography during resuscitation can be a curial factor contributing to nurses’ lack of confidence when using capnography, especially in emergency cases.
To summarize, this theme in academic research demonstrates several barriers that nurses encounter when using capnography during CPR. The most important one is the lack of training, which results in other problems arising when the hospital or unit wants to implement changes. Moreover, the lack of standardized data further increases nurses’ resistance to change, which offers some insight into the basis for the current project.
Summary
Overall, the problem that this project explores is the practice of using capnography in the ICU setting during patient resuscitation and the impact of nurses’ knowledge about the tool on the prevalence of use and CPR outcomes. The origin of the issue is connected to evidence presented by scholars, suggesting that nurses both in the United States and in Europe do not apply capnography to guide cardiac massage and track respiratory patterns of patients, despite the availability of capnography tools (Wright, 2017). This project aims to improve the lack of understanding associated with the perception and knowledge of capnography utilization and patient outcomes. Works similar to the study by Sahyoun, Siliciano, and Kessler (2018) aim to examine the problem of knowledge about capnography, perception, and the frequency of application. However, the sample size is little, suggesting that more attention should be dedicated to the problem of correlation between knowledge and application. The current literature lacks a study that would focus on this factor and use qualitative design.
The empirical evidence on the topic of capnography suggests that in most cases, using capnography during CPR improves the accuracy of cardiac massage and survival chances. The problem has evolved historically since initially capnography was developed as an instrument applied during anesthesia, but current trends suggest that it can make the care better across many domains (Jooste et al., 2019). However, the ability to use capnography is obstructed by the lack of knowledge and training. Capnography allows medical professionals to monitor a patient’s well-being in the ICUsand nurses in these units should receive not only protocols or guidelines but also adequate training on capnography.
In general, the application of capnography across different domains of patient care becomes more popular. The main trends in applying capnography for patient monitoring within the ICU settings are connected to the promotion of using this tool and improvement of result interpretation that can be obstructed by distortions (Aramendi et al., 2017; Chicote et al., 2019). The primary trend that prevails in the literature is the adoption of capnography for use in a different medical setting, including the ICU. The expansion of the use scope for this instrument suggests that many hospitals will want to have capnography available at each ward, further emphasizing the need to examine personnel’s ability to use this tool correctly (Kerslake & Kelly, 2016). In addition, many researchers develop specific algorithms, including computer programs that help enhance the result interpretation or automate the process of monitoring using capnography (Chicote et al., 2019). One can argue that the general trend is the application of capnography across different units and the improvement of application strategies.
Many studies are based on a small research sample of 20-30 nurses or patients, which can mean underrepresentation. The authors generalize the findings to create a conclusion based on the evidence they collect (Kerslake & Kelly, 2019; Jooste et al., 2019). From this perspective, one can argue that the evidence supporting the efficiency of using capnography in the ICU during resuscitation is not justified. However, other studies focus on exploring patient records to determine the effect of resuscitation using capnography on mortality, which can incorporate enough samples. Conflicts in methodology are connected to the prevalence of quantitative studies that assess the availability of capnography tools, the number of cases where it was applied, and outcomes.
Hence, a significant gap in the literature is the lack of evidence that would provide an understanding of nurses’ knowledge of capnography and attitudes towards using this tool. Prior research is done on the topic that explores the chosen phenomena is assessing the prevalence and specifics of nurses using capnography and suggests that in most cases, this instrument is not applied during CPR. Hence, the phenomena explored in this project are nurses’ knowledge, capnography use during CPR, and patient mortality, and the connection between these factors. The majority of the examined studies focus on the advances of using capnography and the specifics of its application (Kerslake & Kelly, 2016). Additionally, it can be argued that a gap in understanding the nurses’ knowledge and its impact on the perception of a tool exists, suggesting that projects such as this DPI can enhance the procedures at hospitals.
The methodologies and design used to explore the topic of capnography for resuscitation range from qualitative discussions to quantitative surveys, both of which can assess nurses’ knowledge regarding the use of capnography. The literature relates to the DPI since it explores the issue of resuscitation and the benefits of using capnography when measuring CO2 levels. While evidence suggests that using capnography, during resuscitation helps decrease mortality rates, some medical professionals do not use this tool and the ability to identify what factors influence this choice can help design interventions and practice improvement strategies that target the problem (Wright, 2017; de Caen & Maconochie, 2018). Since this DPI project is quantitative, the studies were chosen for the literature review that explored the data surrounding capnography as well as some barriers for nurses that the project could acknowledge when planning for change. In this way, the practices and best approaches for using capnography were located that allowed one to understand the specifics of this tool. Besides, the literature review allows comparing and contrasting different methods and the evolution of using capnography in CPR.
The reason for choosing Lewin and his change model as the foundation for this project lies in the gaps identified in the literature review. It is apparent that the equipment for capnography is present in most hospitals, and sufficient data exists to support the use of this tool during resuscitation. Nevertheless, the rates of using this instrument remain low, and nurses express hesitations surrounding this topic. Thus, a change theory that acknowledges people’s fear of change and resistance to new systems is necessary. Lewin’s model offers a simple theoretical base that shows how these obstacles can be overcome.
The quantitative, quasi-experimental methodology with an application of surveys was chosen to connect patient outcomes and nurses’ use of capnography in a calculable and transparent way. The main goal is to determine the degree to which capnography use during resuscitation impacts patient outcomes and nurses’ subsequent implementation of this tool in the unit. The appropriateness of the DPI’s strategies recommended by the similarities of design in the examined studies since the ones relating to the use of capnography in a clinical setting employed questionnaires and knowledge tests, as well as data such as mortality rates, similar to the model chosen for this DPI. Chapter 3 will focus on exploring the clinical question and on the methodology used for this DPI, using findings from the literature.
Methodology
This DPI project focuses on the use of capnography during CPR by nurses, linking their knowledge of capnography techniques and the application of capnography within an intensive care unit (ICU). To validate the arguments set forth, a quantitative method was chosen to explore the relationship between nursing knowledge of the utilization of capnography and how its usage was pertinent in positive outcome generation with the intensive care units (ICU). The questions guiding this project are whether nurses’ knowledge of capnography impacts the frequency of using this tool during resuscitation and whether nurses’ knowledge of capnography influences their compliance with capnography guidelines and procedures. Improving nursing knowledge in capnography is essential in increasing the quality of care and resuscitation efforts in generating positive outcomes for patient success rates and promoting increased patient outcomes. This chapter of the DPI project explores the methodology to be used in greater depth, including sampling procedures, data collection instruments, and data analysis methods in the evaluation of the premise.
Statement of the Problem
The purpose of this quantitative, quasi-experimental project is to determine to what degree the implementation of capnography during cardiopulmonary resuscitation (CPR) when compared to the current practice would impact the use of capnography during CPR for adult ICU patients at an acute care hospital in New Jersey within a four-week period. Nurses working in intensive care units, where the risk of cardiac arrest is high, are required to use evidence-based tools and strategies to reduce patient mortality (Israel, 2014; Jaffe, 2017). Capnography provides details about the patient’s condition and assists care providers in tracking changes in the patient’s condition to avoid complications (Heradstveit & Heltne, 2014; Pantazopoulos et al., 2015). Capnography proved to be effective in promoting increased patient outcomes in the detection of abnormalities associated with fluctuations in CO2 levels and following cardiac arrests (Cereceda-Sánchez & Molina-Mula, 2017; Chhajed et al., 2016; Darocha et al., 2017; Hassankhani, Aghdam, Rahmani, & Mohammadpoorfard, 2015).
The widespread application of capnography during resuscitation attempts within specific clinical settings has yet to be achieved due to the lack of specialized training that focuses on the project and understanding of its use (Dioso, 2014; Duckworth, 2017). This subject has not been addressed in the literature, specifically since most studies focused on the various applications and benefits of capnography. Hence, it is not known whether increased nurses’ knowledge of capnography is associated with improved use of this tool during cardiopulmonary resuscitation
The problem discussed above affects various patient populations who are at risk of a cardiac arrest, including patients in intensive care units as well as those with chronic cardiovascular conditions. The barriers to consistent implementation of capnography use within a critical care setting prevent care providers from delivering the highest quality of care, thus posing a risk for patients’ survival during a cardiac arrest. Hence, it is essential to explore the factors that could hinder the use of capnography in high-risk settings, as this would help to develop evidence-based strategies to enhance capnography use Evidence of a positive relationship between nurses’ knowledge of capnography, their readiness to use this tool, and the rate of capnography use during CPR would help to fill the gap in current literature expanding on the significance of these techniques.
Clinical Question
The following clinical question guides the present quantitative project: To what degree does implementation of an evidence-based intervention on use of capnography during cardiopulmonary resuscitation (CPR) impact use of capnography during CPR when compared to current practice, among adult ICU patients in an acute care hospital setting in New Jersey within a four-week period? This clinical question presents the two main variables that were explored in this DPI project. The independent variable is the implementation of an evidence-based intervention that centers on teaching nurses about the use of capnography during CPR. Consequently, the dependent variable is the expected outcome – the number of cases of CPR where capnography is used by nurses in the selected unit of the hospital, ICU (see Table 1).
Table 1: Characteristics of Variables
The project’s methodology is quantitative, and both variables are represented by numbers. For the independent variable, an existing instrument was used to measure nurses’ knowledge of capnography. Designed by Kiekkas et al. (2016), the Nurses’ Knowledge about Capnography Test (NKCT) provided a validated test for collecting data about the outcomes of the proposed intervention and the knowledge that nurses in the ICU possessed about using capnography. The design was selected as it aligned with the clinical question, and its questions directly addressed nurses’ potential hesitation and overall preparedness for using capnography during CPR. For the dependent variable, the Electronic Health Records was chosen as the main source of data, as it contained all necessary information about patients residing at the unit, the number of codes the unit had in regards to CPR, and how many times the use of capnography during resuscitation was registered.
The quantitative quasi-experimental was selected to answer the posed clinical question. First, the primary purpose of the project was to introduce an improvement to the existing practice, which implies the need for a quasi-experimental or experimental design as opposed to descriptive and correlational studies that examine existing relationships. Second, the investigator did not have the ability to randomly select the sample on assign groups due to the nature of the intervention. Thus, the experimental design could not be used for the DPI project, and the quasi-experimental design was the best possible option to answer the clinical question.
Project Methodology
The methodology selected for the project is quantitative; this is justified by the need to explore the subject from an objective viewpoint. The primary benefits of quantitative methods are that they provide accurate numerical information reducing the risk of bias. The quantitative methodology incorporates mathematical, statistical, and numerical analysis of gathered data using computational techniques (Valente & MacKinnon, 2017). The information can be collected with the help of surveys, questionnaires, and by using existing statistical data or health records and manipulating it with technology. This methodology provides an opportunity to answer the clinical question on the basis of objective calculations, which leads to data generalization across groups of people.
Additionally, according to Jones (2016), quantitative methods focus on providing a vast scope of information rather than on exploring some variables in-depth. This means that such methods could be useful in settings where there is a need to collect as much information as possible and draw sound conclusions from it. In the present case, gathering more information would benefit the project presented by providing more evidence of a connection or lack thereof between the variables and the effect that the intervention could have on the expected outcome. The data collected in quantitative projects is also simplistic in its nature, which makes it particularly useful for observing changes in variables, analyzing data for correlations, and presenting it for review and replication (Ali & Bhaskar, 2016; Heale & Twycross, 2015; Leppink, O’Sullivan, & Winston, 2016; Watson, 2015).
Quantitative data sources are particularly helpful in obtaining evidence about the effects of one variable on another, which was the primary goal of this project. It is more useful and practical than the alternative qualitative methodology for several reasons. In contrast with quantitative data sources, qualitative methods focus on obtaining meaningful information about the participants’ attitudes and beliefs and allow doing so by enhancing the depth of data collected (Austin & Sutton, 2014; Barnham, 2015; Flanagan, Greenfield, Coad, & Neilson, 2015; Gunnell, 2016). Qualitative projects focus on the participants’ perceptions rather than on objective information; they take information that is challenging to measure and draw specific themes based on individual views of the problem and related theories.
In this DPI improvement project, qualitative methods would allow one to explore nurses’ beliefs about their own knowledge about the implementation of capnography use in CPR and its importance. This information, however, would not show how an intervention could affect the use of capnography during CPR and patient outcomes connected to the change (Barnham, 2015). The dependent variable is quantifiable, and the quantitative methodology allows the investigator to see the relationship between nurses’ training and their decision making by analyzing the records and nurses’ knowledge.
The selected methodology is better suited to answer the posed clinical question in two ways. By allowing the evaluation of the level of knowledge about capnography objectively, in contrast with qualitative methods, and establishment of the effect nursing knowledge has on the practice could be examined. Given the nature of the problem at hand, evaluating factual knowledge is more important because it provides more information about the effectiveness of nursing education in capnography. Secondly, quantitative data obtained through the EHR would be more structured, thus making it easier to analyze how nurses’ knowledge translates into their practice.
Project Design
The chosen design for the quantitative project is quasi-experimental. As explained above, this is the most suitable design for the DPI project and the best fit for answering the set clinical question. A quasi-experimental design is similar to experimental projects in that it measures the causal impact of an intervention (Alessandri, Zuffianò, & Perinelli, 2017). However, in contrast to pure experiments, this design does not use a randomized population sample, assuming partial or full control over the sample’s selection instead. Moreover, the unique feature of one-group quasi-experimental projects is that they do not use a control group for comparison, using results from one sample group (Alessandri et al., 2017). Thus, the design allows for more control over the project, but some limitations and potential challenges arise.
The fit of the quasi-experimental design for the current intervention relies on its ability to directly address the clinical question. The latter explores the connection between nurses’ knowledge of capnography under the influence of intervention before and after the program has been implemented and the effect of this initiative on the use of capnography. According to Valente and MacKinnon (2017), the aim of quasi-experimental projects is to examine the impact of such change programs. Furthermore, the increased attention to choosing the sample implies the ability of the investigator to use their desired setting for the project and see how the intervention affects specific populations. In this case, the nurses’ participation in training makes them a necessary part of the project. At the same time, only patients who experienced cardiac arrest and required CPR could be eligible for the project, and randomization of the sample seems inconvenient for exploring the clinical question.
The role of quasi-experimental design is apparent in the variables outlined in the project – the number of resuscitations with the use of capnography before and after the intervention requires a highly specific set of patients in the hospital, the examination of which would be impossible when using other quantitative designs. Similarly, the chosen design explains the use of quantitative methodology and shows how numerical values can be utilized to answer the clinical question. Thus, it further supports the use of quantitative methodology as opposed to qualitative or mixed varieties.
Two sets of data were collected for examination based on the quasi-experimental design, as noted above. The first was the nurse’s knowledge of capnography using the NKCT to demonstrate the effect of the intervention (a training program for nurses about capnography use in resuscitation). The second one was the EHR data about codes that showed the cases of resuscitation in the unit and the use of capnography during these codes before and after the intervention was implemented. The quasi-experimental design allowed the investigator to collect data at points before and after the intervention, employing the pretest-posttest variety of the design, and compare them to demonstrate the effect of change and its significance.
Population and Sample Selection
The setting for the intervention is the ICU of a hospital located in New Jersey, where nurses are under increased pressure to deliver timely care and respond to situations that pose a significant risk to patients’ health. The ICU was chosen because these units have many patients whose health can deteriorate or change rapidly, and they require constant attention and monitoring. Nurses working in the ICU have to act quickly, assisting patients in an environment where each decision may be crucial to their health. Moreover, there is a high incidence of cardiac arrests, and thus nurses are often involved in cardiopulmonary resuscitation (Wright, 2017). The combination of these factors emphasizes the need for the proposed intervention, as the latter aims to increase the quality of care. As a result, the project’s results also present an opportunity for improvement and potential benefits for other units and locations.
The department under examination is a twenty-bed unit that employs 32 nurses and operates at an 8-10 bed capacity. While nurses working at the ICU are not the population for the project, this number is important for investigators as it shows the amount of preparation for training. For instance, this number demonstrates the capacity of nurses to perform CPR and respond to patients’ needs as well as how many days were required to implement the training program and assess nurses’ knowledge of capnography.
The project population includes all patients who were treated at the selected ICU during the project. The sample for the project is patients who experienced cardiac arrest and underwent resuscitation in the intensive care unit of the selected location. The inclusion criteria for the sample requires patients who are treated in the selected unit at the time of the project. Moreover, these patients have to have experienced the code situation (cardiac arrest) and underwent cardiopulmonary resuscitation as a result. Exclusion criteria for the sample are based on age – only adult patients who were older than 18 at the time of the implementation are considered to deliver results that could be generalized for a larger adult population (Mohamed, 2019). Furthermore, patients who had a cardiac arrest but did not undergo resuscitation were excluded as well. Reasons for not performing CPR could include a Do Not Resuscitate (DNR) order.
The size of the sample for patient CPR cases can not be determined preemptively as the number of cardiac arrests is not a measure that can be predicted. The conclusive records about the code situation and the use of capnography can be obtained only after the period of the intervention is over, thus finalizing the project sample size only after the four-week duration of the project’ phase. Nevertheless, the sample size is not controlled or restricted, thus demonstrating the flow of patients and case situations in an environment without the investigator’s influence. The number of nurses who need to complete the NKCT is 32 – as all nurses in the unit are required to attend training.
The selected sample size is rather small for a quantitative project because this design implies collecting data from as many charts and participants as possible (Cronin et al., 2014). This is because the size of the sample in this project is constricted by the geographical location of the project and the focus on intensive care units, which limits the number of cases available for the project. However, since the project does not follow an experimental design, which would require setting the sample size based on power analysis, the selected sample size will likely be enough for a quasi-experimental design (Cronin et al., 2014). Moreover, the focus on ICUs allows one to discuss the connection between the specific department’s setting and nurses’ skill and their treatment of patients.
The geographic specifications of the project mean that nurses will be recruited from a single state; in this case, New Jersey, where the evaluation of this DPI improvement project would be performed. Nurses will not have to travel to take the test; instead, all data collection procedures will be conducted at their place of work in a way that does not impair the workflow. Similarly, patients will not be disturbed to gather data about cases of cardiac arrest – EHR is the main source of information. All data will be anonymized to remove identifying information such as names and occupations.
Instrumentation and Sources of Data
There are two variables for which data has to be collected – the intervention which is described by nurses’ knowledge of capnography and the number of CPR cases with the use of capnography. The type of data for all variables will be quantitative, but the data will come from two different sources. This separation of the instrument and a source of data is required to show the effect of the intervention on the use of capnography.
The Nurses’ Knowledge about Capnography Test (NKCT). The NKCT will be used to collect the required data on the nurses’ knowledge of capnography. This tool was developed by Kiekkas et al. (2016) and included 30 correct and wrong statements about capnography.
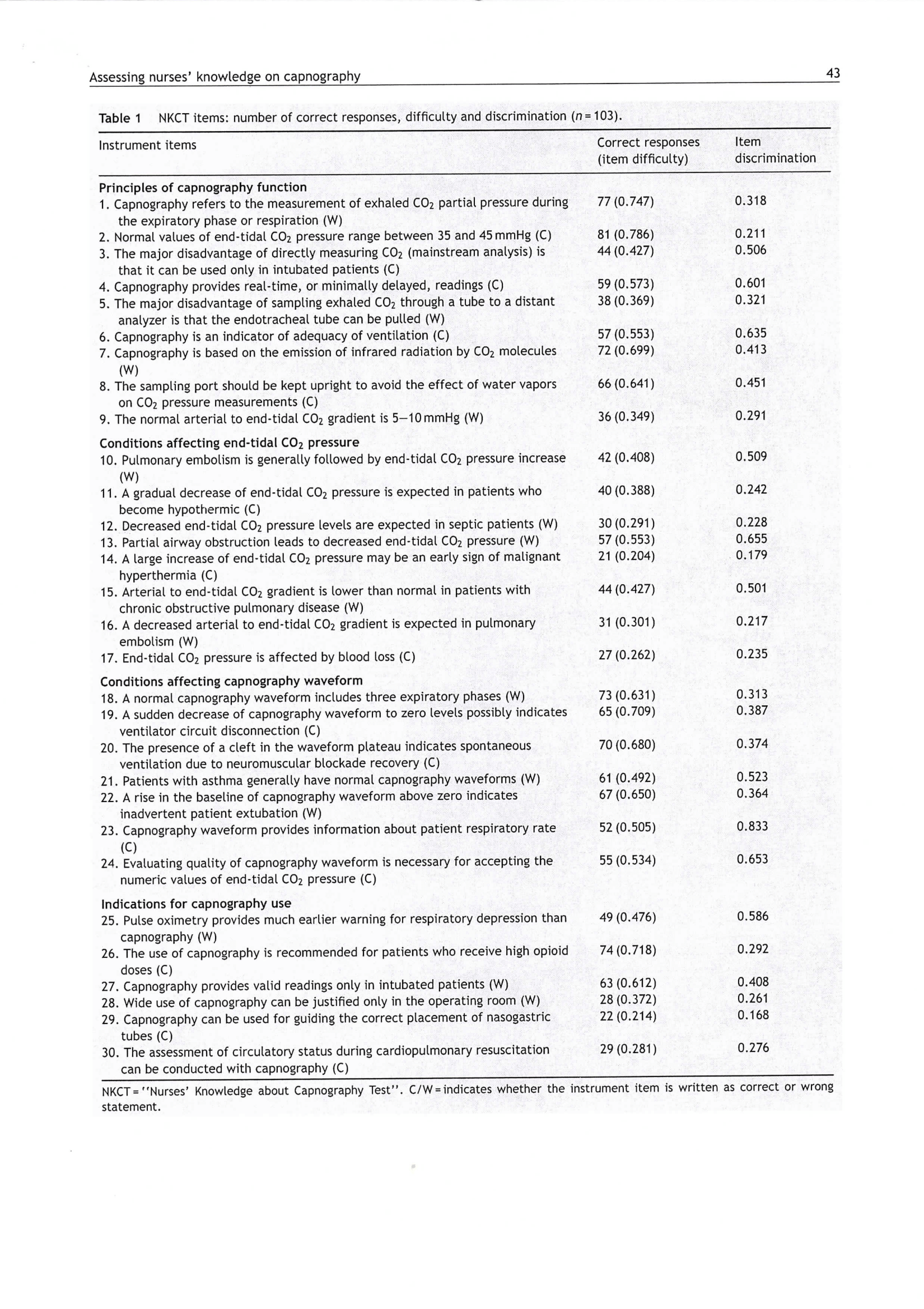
The items are separated into four groups: principles of capnography function, conditions affecting end-tidal CO2 pressure, conditions affecting capnography waveform, and indications for capnography use (Kiekkas et al., 2016). The test will be delivered to all nurses identified through probability sampling (all nurses working at the selected ICU) and marked on correctness to determine the level of capnography knowledge. The test will be scored on a 30-point scale, and thus the results will be quantitative. The NKCT is an established tool for appraising nurses’ knowledge of capnography, thus making it an appropriate selection for this project as a test with proven results.
The Electronic Health Record (EHR) data about the code situation. The second source of data is the EHR of the selected ICU, which contains information about the patients treated at the hospital. The records document patients’ descriptions, including their age, gender, and ethnicity, which will be collected to make the data set more informative. The primary type of data, however, will be the number of cardiac arrests and resuscitations with and without the use of capnography. The data will be collected and stored electronically in an Excel spreadsheet to ensure that each instance is properly documented. The number of code situations with CPR will be recorded as a cardinal number, and each instance of CPR will have a descriptor of “1” and “0” to denote the use (or non-use) of capnography. Thus, the final type of data will be a ratio.
The use of the EHR has high validity and reliability as health records are the main place for the hospital to gather all data related to patients’ health (Lin et al., 2018). It is an official source of information that is handled by the staff, which implies that all code situations have to be in one place. The permission from the hospital to collect and use data will be obtained, and the data will be anonymized to ensure participant’s privacy – patient’s names will be replaced with numbers, and only their age, gender, and ethnicity will be collected to avoid potential identification.
Validity
The NKCT has already been evaluated for its validity specifically in its use to construct validity using techniques designed to test the relationship between NKCT and the knowledge base of nurses in capnography (Kiekkas et al., 2016). The authors used nurses’ experience in the anesthesiology department and the date of introduction of capnography to the said department to determine nurses’ capnography experience, whereas education levels were derived from nurses’ qualifications (Kiekkas et al., 2016). The authors concluded that the evaluated construct validity was high because both characteristics had a positive effect on the NKCT scores as predicted (p=0.038 and p=0.003, respectively). Hence, the use of an instrument with high construct validity will ensure that the data collected on nurses’ knowledge also has high validity.
Secondly, the validity of EHR data depends on the fulness of patient information. According to Lin et al. (2018), high data completeness increases the quality of gathered information and improves the results of the analysis. Most problems arise when projects require patient information from different provides or out-of-hospital situations (Lin et al., 2018). Acknowledging the fact that the present project uses a small part of patient data that pertains to their treatment at the single unit, the validity of the data gathered from the EHR is high.
The DPI project requires only a small set of descriptive characteristics (age, gender, ethnicity) and the code for cardiac arrest and CPR with or without capnography. All needed information is recorded by staff of the department or administrative personnel, and the participation of clinicians outside of the hospital is not necessary to collect this data. Thus, the factor of EHR-continuity does not have a significant influence on the results of the data collection process. The use of the validity score developed by Lin et al. (2018) is, therefore, not needed to ensure the fulness of information, as is does not affect the clinical question’s outcome.
Reliability
Similar to the instrument’s and data source’s validity, the reliability of both data collection methods will be assured to provide reliable outcomes. Concerning the NKCT, the test’s reliability has already been evaluated by its creators. Kiekkas et al. (2016) note that they applied internal consistency and item analysis to determine the reliability of the instrument. Kuder-Richardson 20 coefficient was used based on the type of the test (dichotomous choices). The point-biserial correlation index was also applied, yielding the results from 0.168 (poor item discrimination) to 0.833 (excellent item discrimination), with most items (28 out of 30) having either good or acceptable discriminatory value (Kiekkas et al., 2016). This means that the internal consistency of the test is high, which allows it to collect data with a high degree of reliability. The internal consistency was supported by intra-rater reliability evaluation. Both tests used by the authors provide an adequate degree of certainty, which is why they are used to ensure the reliability of data collected using this instrument.
Data Collection Procedures
Before the data collection begins, obtaining institutional approval from the selected hospital to conduct tests and observations in intensive care units is the first step in initiating the process. Once the approval has been received, data sources requiring a list of all nurses working in the intensive care unit of the selected hospital would be obtained. This would form the basis of the project to access the knowledge of nurses’ working in this setting from a quantitative perspective. The nurses involved in the project will be contacted by e-mail, and information about the results and findings would be explored in detail. The project of nurses knowledge and capnography through quantitative evaluations in the use of the institutional provided data source analysis tool, in addition to the NKCT, have been performed with the relevant documentation and procedures ensuring privacy and confidentiality of the nurses partaking in the project (Cronin et al., 2014; Price et al., 2017).
Due to the nature of the pretest-posttest design, the data collection of nurses’ knowledge of capnography should be completed before and after the educational program has been completed by the participants to demonstrate whether the intervention had an effect on nurses’ perception of capnography. It will employ the NKCT to examine the independent variable in the project (Kiekkas et al., 2016). All participating nurses working within the ICU setting will take the test in a controlled environment, such as in a conference room. The test will be completed either after the nurses’ shift or before so that it would not disrupt their workflow. For any nurses who have difficulties in scheduling, the test will be conducted individually.
The second part of data collection will involve using the hospital’s EHR to gather information about patients and instances of CPR. As noted previously, a small set of patient descriptions is necessary to make the data set more informative. Adding such information as one’s gender, age, and ethnicity can present valuable findings for future studies and show whether the sample is heterogeneous and suitable for generalization. Moreover, each instance of cardiac arrest with CPR will be recorded, noting which of the cases involve capnography. This information for the pretest examination will be collected 28 days prior to the start of the program to form a set of comparative baseline data. The second set of data (for posttest analysis) with similar contents will be requested at the end of the program (28 days after the start of the program). As the data will be collected from digital recordings, minimal manipulation will be necessary to standardize the information and present it in an Excel spreadsheet.
Both data sets do not require informed consent since the intervention involves all nurses, and patient data is collected through the EHR. Nonetheless, the agreement with the hospital about the amount and types of data provided will ensure that the investigator has access to the necessary information. As mentioned previously, all data will be anonymized, and the results of the NKCT and EHR data gathering will be coded to exclude any uniquely identifiable information such as names or positions. The data will be stored digitally or a password-locked computer and destroyed in one year after the end of the project.
Data Analysis Procedures
For the purposes of the present project, data on two variables will be collected: nurses’ knowledge of capnography before and after the intervention and the use of capnography during CPR. For the first variable, quantitative data will be collected using the Nurses’ Knowledge on Capnography Test. For the second variable, quantitative data will be obtained from the EHR (BETP, 2017; Kiekkas et al., 2016). The clinical question to be answered using data analysis is to what degree implementation of an evidence-based intervention on use of capnography during cardiopulmonary resuscitation (CPR) impacts the use of capnography during CPR when compared to current practice, among adult ICU patients in an acute care hospital setting in New Jersey within a four-week period.
Data analysis methods are critical to quasi-experimental pretest-posttest data studies in that they assist in determining any effects that the independent variable may have on the dependent one. Firstly, the difference between pretest and posttest values has to be determined to show whether change happened during the intervention. The use of two measurement points – before and after the intervention – for both variables implies the need for a t-test. The t-test is used to compare the mean of two given samples when the standard and mean deviation are not known (Alessandri et al., 2018). For this case, a paired sample t-test is required to compare the numbers for one group at different points in time.
For the first variable, the t-test will denote any differences between nurses’ scores on the NKCT – two sets of raw data will be collected from the surveys by hand and input into processing software. For the second variable, the rates of code situations with the use of capnography out of all code situations will be calculated and input into processing software. It is essential to present the data in the form of rates, since the initial numbers of resuscitations with capnography may not represent the overall rate of CPR instances during the two periods of data collection. Thus, to start the analysis, the number of code situations of CPR with the use of capnography will be divided by the overall number of CPR during cardiac arrest. This calculation will provide two sets of data, which then can be compared using the t-test to demonstrate a change in the use of capnography over time. The level of statistical significance for the project is set at p=0.05, which is a standard level used in many studies in nursing (Cronin et al., 2014).
The improvement from the results of pretests to the outcomes of posttests is calculated using the Gain score. The results are achieved by subtracting the first score from the second one; positive scores demonstrate gain, while negative scores show loss of knowledge or use of capnography. This data analysis method will help to answer the clinical question posed for the project by identifying the change of nurses’ capnography knowledge and their use of capnography. The information regarding the level of change will also be necessary for examining nurses’ knowledge of capnography use.
For example, if the identified gain is positive and very strong, nursing education that aims to increase nurses’ capnography knowledge is likely to result in significant improvements in the use of capnography. Therefore, the quasi-experimental design will formulate answers by providing meaningful information that could be used in practice improvements. The use of specific statistical tools, such as XLSTAT, will help to ensure the correctness of calculations while also supporting the data analysis process. The chosen data analysis procedure also relates to the purpose of the project as it will explore the possible relationship between nurses’ knowledge of capnography and their use of this tool during resuscitation in great depth.
Potential Bias and Mitigation
The potential risk of bias exists in the stages of data collection and analysis. Taking the test in a controlled environment is important to reduce the risk of bias (Price et al., 2017). If nurses were to take an online test, they would be able to search for additional materials, thus showing a higher level of knowledge than they possess. Hence, the proposed procedure will have a beneficial impact on the quality of the findings. Each test will be completed in the intensive care unit, on paper and marked with the nurse’s identification number to prevent bias in quantitative data results. It is vital to note that nurses’ names will not appear on paper, lowering the risk of a privacy breach.
Another point of bias is the calculation of changes before and after the intervention. The use of the rate of capnography use in comparison to the overall number of CPR is necessary to mitigate this risk as the unit may have vastly different numbers of code situations, thus producing varying results of capnography use. However, the chosen setting implies a high number of CPR performed in the unit, thus lowering the impact of this concern on the project.
Ethical Considerations
The present project involves human subjects, and it is particularly important to protect their rights and conduct the project in an ethical way (Sanjari, Bahramnezhad, Fomani, Shoghi, & Cheraghi, 2014; Zyphur & Pierides, 2017). The key ethical issues relating to the project are the confidentiality and privacy of personal information provided by the participants and the disruption of nurses’ workflow during the project. Both problems mentioned above violate the principles of the Belmont Report since they might cause harm to the nurses and their patients.
In order to address these issues, the project was modeled in a way that minimizes workflow disruptions.
For instance, testing will take place outside of the nurses’ shifts, and data collection will be conducted from the EHR without disturbing patients or staff. Additionally, measures to protect data privacy and confidentiality will be applied. Personal information about the participants will be stored safely on a password-protected device and destroyed after one year by deleting electronic documents and shredding paper documentation. Identifying information, including names and e-mail addresses, will be replaced with identification numbers during data collection and analysis. No contact with patients will be made throughout the project, so no harm to them will be caused.
IRB approval to conduct the project will also be received, which means that the project will be done on a voluntary basis, and nurses will participate based on their motivation. The documentation will provide all relevant information about the project, including the ethical measures taken to protect the participants, their work, and data. No potential conflicts of interest were identified at this stage since the investigator is not connected to the hospital or nurses who will participate in the project. As the project may be published in scholarly journals, precautions will be taken to protect subjects’ privacy and confidentiality at the publication stage. The documents shown to third parties will be checked to ensure the absence of identifying information, and the publication will only reveal the findings and will not contain any identification numbers.
The data shared by the institution and the nurse participants will be stored securely on a password-protected computer, and the participants’ numbers will be used instead of their names during data collection and analysis. The data will be held for one year following the end of the project and will be destroyed. Explanations into the project’s premise would be presented in their entirety to the nurses, and e-mail verification solidifying understanding into the proposed clinical question would prove useful for the setting presented. These precautions are in accordance with the European University Institute guide on data protection practices, and they will help to ensure that the participants’ rights will be preserved throughout the duration of the project (EUI, 2019). Additionally, it is important to note that no contact with patients will be made during the project, and thus patients’ health and well-being will not be affected by the project in any way.
Limitations
While the project has been carefully designed to provide high-quality information on the problem and avoid bias, there are still two limitations related to its methodology. Firstly, the sample size of the project is smaller than in other quantitative studies in nursing (Cronin et al., 2014). New Jersey was chosen as the site of the project because of the need to conduct observations, and thus moving the project to another state would not be feasible. Additionally, the focus is on an intensive care unit, limiting the number of nurses in the sample. Enhancing the scope of the project would not help to achieve project goals because most other groups have a lower frequency of cardiac arrest and would thus provide incomplete data. Hence, the chosen sample size is the best option given the geographic location of the project.
Another limitation is the facility under investigation has only two portable capnography monitors available, which means that nurses will be able to use capnography in two simultaneous code stations. However, it is reported by the unit’s representatives, that it is rare for more than two codes to happen at the same time, so this limitation presents a low risk to the project. If a third code were to occur, the project’s results could be influenced, and these instances have to be recorded to ensure transparency.
Conclusion
The purpose of this quantitative quasi-experimental project is to explore the impact of nurses’ knowledge of capnography on their capnography use during CPR in intensive care units. The quantitative methodology is the best fit for the project’s purpose because it will provide objective data needed to establish the relationship between the variables (Barnham, 2015; Cronin et al., 2014).
Additionally, the quasi-experimental pretest-posttest design of the project is tailored to the needs of the project because it focuses on establishing the level of change and the relationship between the two variables (Curtis et al., 2016). The data collection procedures that involve conducting surveys of nurses’ knowledge about the appropriate use of capnography through NKCT and data gathering from the EHR will provide adequate measurements of the variables presented (Kiekkas et al., 2016).
Descriptive statistics, t-tests, and gain scores will also be applied to draw conclusions from the data sources provided as well (Price et al., 2017). The sequence of procedures chosen for the project will help to respond to the clinical question and fulfill the purpose of the project in evaluating and improving clinical practice.
References
2015 international guidelines on CPR: Recommendations for capnography. (2015). Web.
Alessandri, G., Zuffianò, A., & Perinelli, E. (2017). Evaluating intervention programs with a pretest-posttest design: A structural equation modeling approach. Frontiers in Psychology, 8(223), 1-12.
Ali, Z., & Bhaskar, S. B. (2016). Basic statistical tools in research and data analysis. Indian Journal of Anaesthesia, 60(9), 662-669.
Aramendi, E., Elola, A., Alonso, E., Irusta, U., Daya, M., Russell, J. K.,… Sterz, F. (2017). Feasibility of the capnogram to monitor ventilation rate during cardiopulmonary resuscitation. Resuscitation, 110, 162-168.
Aramendi, E., Lu, Y., Chang, M., Elola, A., Irusta, U., Owens, P., & Idris, A. (2018). A novel technique to assess the quality of ventilation during pre-hospital cardiopulmonary resuscitation. Resuscitation, 132, 41-46.
Austin, Z., & Sutton, J. (2014). Qualitative research: Getting started. The Canadian Journal of Hospital Pharmacy, 67(6), 436-440.
Barnham, C. (2015). Quantitative and qualitative research: Perceptual foundations. International Journal of Market Research, 57(6), 837-854.
Bullock, A., Dodington, J. M., Donoghue, A. J., & Langhan, M. L. (2017). Capnography use during intubation and cardiopulmonary resuscitation in the pediatric emergency department. Pediatric Emergency Care, 33(7), 457-461.
Bureau of EMS, Trauma, & Preparedness. (2017). Procedures: End-tidal carbon dioxide monitoring. Web.
Burnes, B. (2004). Kurt Lewin and the planned approach to change: A re‐appraisal. Journal of Management Studies, 41(6), 977-1002.
Burnes, B., & Bargal, D. (2017). Kurt Lewin: 70 years on. Journal of Change Management, 17(2), 91-100.
Campbell, C. M. (2017). An inside view: The utility of quantitative observation in understanding college educational experiences. Journal of College Student Development, 58(2), 290-299.
Carlisle, H. (2015). Promoting the use of capnography in acute care settings: An evidence-based practice project. Journal of Perianesthesia Nursing, 30(3), 201-208.
Center for Innovation in Research and Teaching. (2013a). Quantitative approaches. Web.
Center for Innovation in Research and Teaching. (2013b). When to use quantitative methods. Web.
Cereceda-Sánchez, F. J., & Molina-Mula, J. (2017). Capnography as a tool to detect metabolic changes in patients cared for in the emergency setting. Revista Latino-Americana de Enfermagem, 25, 1-10.
Chhajed, P. N., Gehrer, S., Pandey, K. V., Vaidya, P. J., Leuppi, J. D., Tamm, M., & Strobel, W. (2016). Utility of transcutaneous capnography for optimization of non-invasive ventilation pressures. Journal of Clinical & Diagnostic Research, 10(9), OC06-OC09.
Chicote, B., Aramendi, E., Irusta, U., Owens, P., Daya, M., & Idris, A. (2019). Value of capnography to predict defibrillation success in out-of-hospital cardiac arrest. Resuscitation, 138, 74-81.
Conway, A., Collins, P., Chang, K., Mafeld, S., Sutherland, J., & Fingleton, J. (2019). Sequence analysis of capnography waveform abnormalities during nurse-administered procedural sedation and analgesia in the cardiac catheterization laboratory. Scientific Reports, 9(1).
Cook, T., & Harrop-Griffiths, W. (2019). Capnography prevents avoidable deaths. BMJ, 364(l439), 1-9.
Cronin, P., Coughlan, M., & Smith, V. (2014). Understanding nursing and healthcare research. New York, NY: Sage.
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Human Relations, 69(1), 33-60.
Darocha, T., Kosiński, S., Jarosz, A., Podsiadło, P., Ziętkiewicz, M., Sanak, T., … Drwiła, R. (2017). Should capnography be used as a guide for choosing a ventilation strategy in circulatory shock caused by severe hypothermia? Observational case-series study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 25(1), 15.
de Caen, A., & Maconochie, I. (2018). EtCO2 measurement during pediatric cardiac arrest: Does the Emperor have no clothes? Resuscitation, 133, A1-A2.
Dioso, R. P. (2014). Compression-only cardiopulmonary resuscitation as an assessment tool for nursing students – An evaluative literature review. Malaysian Journal of Nursing, 6(1), 44-49.
Duckworth, R. L. (2017). How to read and interpret end-tidal capnography waveforms. Journal of Emergency Medical Services, 42(8). Web.
Edelson, D. P., Yuen, T. C., Mancini, M. E., Davis, D. P., Hunt, E. A., Miller, J. A., & Abella, B. S. (2014). Hospital cardiac arrest resuscitation practice in the United States: A nationally representative survey. Journal of Hospital Medicine, 9(6), 353-357.
Elola, A., Aramendi, E., Irusta, U., Alonso, E., Lu, Y., Chang, M.P., … Idris, A.H. (2019). Capnography: A support tool for the detection of return of spontaneous circulation in out-of-hospital cardiac arrest. Resuscitation, 142, 153-161.
European University Institute. (2019). Guide on good data protection practice in research. Web.
Fawcett, J. (2016). Applying conceptual models of nursing: Quality improvement, research, and practice. New York, NY: Springer.
Fawcett, J., & Ellenbecker, C. H. (2015). A proposed conceptual model of nursing and population health. Nursing Outlook, 63(3), 288-298.
Flanagan, S. M., Greenfield, S., Coad, J., & Neilson, S. (2015). An exploration of the data collection methods utilised with children, teenagers and young people (CTYPs). BMC Research Notes, 8(1), 61.
Flick, U. (2018). An introduction to qualitative research. New York, NY: Sage Publications Limited.
Gong, Y., Lu, Y., Zhang, L., Zhang, H., & Li, Y. (2015). Predict defibrillation outcome using stepping increment of poincare plot for out-of-hospital ventricular fibrillation cardiac arrest. Biomed Research International, 2015, 493472.
Gravenstein, J. S., Jaffe, M. B., Gravenstein, N., & Paulus, D. A. (Eds.). (2011). Capnography (2nd ed.). Cambridge, UK: Cambridge University Press.
Green, J., & Thorogood, N. (2018). Qualitative methods for health research. New York, NY: Sage.
Gunnell, M. (2016). Research methodologies: A comparison of quantitative, qualitative and mixed methods. Web.
Guo, H., Kurokawa, T., Takahata, M., Hong, W., Katsuyama, Y., Luo, F., … Gong, J.P. (2016). Quantitative observation of electric potential distribution of brittle polyelectrolyte hydrogels using microelectrode technique. Macromolecules, 49(8), 3100-3108.
Gutiérrez, J. J., Leturiondo, M., de Gauna, S.R., Ruiz, J. M., Leturiondo, L. A., González-Otero, D. M., … Daya, M. (2018). Enhancing ventilation detection during cardiopulmonary resuscitation by filtering chest compression artifact from the capnography waveform. PLOS ONE, 13(8), e0201565.
Haines, L. E. (2017). Continuous-waveform capnography: A crucial tool for ED clinicians. American Nurse Today, 12(1). Web.
Hamrick, J. T., Hamrick, J. L., Bhalala, U., Armstrong, J. S., Lee, J. H., Kulikowicz, E., … Shaffner, D. H. (2017). End-tidal CO2–guided chest compression delivery improves survival in a neonatal asphyxial cardiac arrest model. Pediatric Critical Care Medicine, 18(11), 575-584.
Harper, C. (2005). Capnography: Clinical aspects. Journal of the Royal Society of Medicine, 98(4), 184-185.
Hartmann, S. M., Farris, R. W., Di Gennaro, J. L., Roberts, J. S. (2015). Systematic review and meta-analysis of end-tidal carbon dioxide values associated with return of spontaneous circulation during cardiopulmonary resuscitation. Journal of Intensive Care, 30, 426–35.
Hassankhani, H., Aghdam, A. M., Rahmani, A., & Mohammadpoorfard, Z. (2015). The relationship between learning motivation and self efficacy among nursing students. Research and Development in Medical Education, 4(1), 97-101.
Heale, R., & Twycross, A. (2015). Validity and reliability in quantitative studies. Evidence-Based Nursing, 18(3), 66-67.
Heradstveit, B. E., & Heltne, J. K. (2014). PQRST–A unique aide-memoire for capnography interpretation during cardiac arrest. Resuscitation, 85(11), 1619-1620.
Hussain, S. T., Lei, S., Akram, T., Haider, M. J., Hussain, S. H., & Ali, M. (2018). Kurt Lewin’s change model: A critical review of the role of leadership and employee involvement in organizational change. Journal of Innovation & Knowledge, 3(3), 123-127.
Ingham-Broomfield, R. (2014). A nurses’ guide to quantitative research. The Australian Journal of Advanced Nursing, 32(2), 32-38.
Israel, C. W. (2014). Mechanisms of sudden cardiac death. Indian Heart Journal, 66(1), 10-17.
Izrailtyan, I., Qiu, J., Overdyk, F. J., Ersion, M., Gan, T. J. (2018). Risk factors for cardiopulmonary and respiratory arrest in medical and surgical hospital patients on opioid analgesics and sedatives. PLOS One, 13, e0194553.
Jaffe, M. B. (2017). Using the features of the time and volumetric capnogram for classification and prediction. Journal of Clinical Monitoring and Computing, 31(1), 19-41.
Jones, T. (2016). Outcome measurement in nursing: Imperatives, ideals, history, and challenges. OJIN: The Online Journal of Issues in Nursing, 21(2), 1-11.
Jooste, R., Roberts, F., Mndolo, S., Mabedi, D., Chikumbanje, S., Whitaker, D., & O’Sullivan, E. (2018). Global capnography project (GCAP): Implementation of capnography in Malawi – An international anaesthesia quality improvement project. Anesthesia, 74(2), 158-166.
Kalenda, Z. (1978). The capnogram as a guide to the efficacy of cardiac massage. Resuscitation, 6(4), 259-263.
Kalmar, A.F., Allaert, S., Pletinckx, P., Maes, J.W., Heerman, J., Vos, J.J., … Scheeren, T.W.L. (2018). Phenylephrine increases cardiac output by raising cardiac preload in patients with anesthesia induced hypotension. Journal of Clinical Monitoring and Computing, 1(1), 1-8.
Kaminska, H., Wieczorek, W., Dabrowski, M., Nadolny, K., & Smereka, J. (2018). Knowledge and attitudes of paramedics toward the usage of capnography as a ventilation monitoring tool during resuscitation. The American Journal of Emergency Medicine, 36(6), 1116-1117.
Katz-Buonincontro, J., & Anderson, R. (2018). How do we get from good to great? The need for better observation studies of creativity in education (Opinion article). Frontiers in Psychology, 9, 2342.
Kerslake, I., & Kelly, F. (2017). Uses of capnography in the critical care unit. BJA Education, 17(5), 178-183.
Kiekkas, P., Stefanopoulos, N., Konstantinou, E., Bakalis, N., & Aretha, D. (2016). Development and psychometric evaluation of an instrument for the assessment of nurses’ knowledge on capnography. Collegian, 23(1), 39-46.
Kodali, B. S. (2013). Capnography outside the operating rooms. Anesthesiology: The Journal of the American Society of Anesthesiologists, 118(1), 192-201.
Kodali, B. S., & Urman, R. D. (2014). Capnography during cardiopulmonary resuscitation: Current evidence and future directions. Journal of Emergencies, Trauma, and Shock, 7(4), 332-340.
Kuisma, M., Salo, A., Puolakka, J., Nurmi, J., Kirves, H., Väyrynen, T., & Boyd, J. (2017). Delayed return of spontaneous circulation (the Lazarus phenomenon) after cessation of out-of-hospital cardiopulmonary resuscitation. Resuscitation, 118, 107-111.
Lampe, J. (2017). Improved ventilation monitoring during CPR. Resuscitation, 110, A3-A4.
Langham, M. L., Li, F. Y., & Lichtor, J. L. (2016). Respiratory depression detected by capnography among children in the postanesthesia care unit: A cross-sectional study. Pediatric Anaesthesia, 10, 1010-1017.
Langham, M. L., Li, F. Y., & Lichtor, J. L. (2017). The impact of capnography monitoring among children and adolescents in the postanesthesia care unit: A randomized controlled trial. Pediatric Anaesthsia, 27, 385-393.
Langhan, M. L., Shabanova, V., Li, F. Y., Bernstein, S. L., & Shapiro, E. D. (2015). A randomized controlled trial of capnography during sedation in a pediatric emergency setting. The American Journal of Emergency Medicine, 33(1), 25-30.
Leppink, J., O’Sullivan, P., & Winston, K. (2016). On variation and uncertainty. Perspectives on Medical Education, 5(4), 231-234.
Leturiondo, M., Ruiz de Gauna, S., Julio Gutiérrez, J., M. González-Otero, D., M. Ruiz, J., A. Leturiondo, L., & Saiz, P. (2019). Waveform capnography for monitoring ventilation during cardiopulmonary resuscitation: The problem of chest compression artifact. Cardiac Diseases in 21St Century. IntechOpen. Web.
Leturiondo, M., Ruiz de Gauna, S., Ruiz, J. M., Julio Gutiérrez, J., Leturiondo, L. A., González-Otero, D. M., … Daya, M. (2018). Influence of chest compression artefact on capnogram-based ventilation detection during out-of-hospital cardiopulmonary resuscitation. Resuscitation, 124, 63–68.
Lewin, K. (1951). Field theory in social science. New York, NY: Harper & Row.
Lin, K. J., Singer, D. E., Glynn, R. J., Murphy, S. N., Lii, J., & Schneeweiss, S. (2018). Identifying patients with high data completeness to improve validity of comparative effectiveness research in electronic health records data. Clinical Pharmacology & Therapeutics, 103(5), 899-905.
Lin, T.Y., Fang, Y.F., Huang, S.H., Wang, T.Y., Kuo, C.H., Wu, H.T., … Lo, Y.L. (2017). Capnography monitoring the hypoventilation during the induction of bronchoscopic sedation: A randomized controlled trial. Scientific Reports, 7(1), 8685-8687.
Lin, Y., Guerguerian, A., Laussen, P., & Trbovich, P. (2015). Heuristic evaluation of data integration and visualization software used for continuous monitoring to support intensive care: A bedside nurses perspective. Journal of Nursing Care, 4(300), 2167-1168.
Link, M. S., Berkow, L. C., Kudenchuk, P. J., Halperin, H. R., Hess, E. P., Moitra, V. K., … Donnino, M. W. (2015). Adult advanced cardiovascular life support. Circulation, 132, 444-64.
Long, B., Koyfman, A., & Vivirito, M. A. (2017). Capnography in the emergency department: A review of uses, waveforms, and limitations. Journal of Emergency Medicine, 53, 829-842.
Lui, C. T., Poon, K. M., & Tsui, K. L. (2016). Abrupt rise of end tidal carbon dioxide level was a specific but non-sensitive marker of return of spontaneous circulation in patient with out-of-hospital cardiac arrest. Resuscitation, 104, 53-58.
Mader, T. J., Coute, R. A., Kellogg, A. R., & Harris, J. L. (2014). Coronary perfusion pressure response to high-dose intraosseous versus standard-dose intravenous epinephrine administration after prolonged cardiac arrest. Open Journal of Emergency Medicine, 2(1), 1-7.
Martínez-Mesa, J., González-Chica, D. A., Bastos, J. L., Bonamigo, R. R., & Duquia, R. P. (2014). Sample size: How many participants do I need in my research? Anais Brasileiros de Dermatologia, 89(4), 609-615.
Merckx, P., Lambert, Y., Cantineau, J., & Duvaidestin, P. (1992). Effect of capnography on resuscitation efforts during CPR. Resuscitation, 24(2), 189.
Mohamed, W. K. (2019). Effect of teaching program on nurses’ knowledge and practice regarding measuring end-carbon dioxide by capnography at critical care units. Assiut Scientific Nursing Journal, 7(18), 145-153.
Morse, J. M. (2017). Analyzing and conceptualizing the theoretical foundations of nursing. New York, NY: Springer.
Nassar, B. S., & Schmidt, G. A. (2016). Capnography during critical illness. Chest, 149(2), 576-585.
Nassar, B., & Kerber, R. (2017). Improving CPR performance. Chest, 152(5), 1061-1069.
Nelson, D. (2018). Quantitative observation: Definition and examples. Web.
Novais, P. M., & Moreira, M. M. (2015). Capnography: A feasible tool in clinical and experimental settings. Respiratory Care, 60(11), 1711-1713.
Pantazopoulos, C., Xanthos, T., Pantazopoulos, I., Papalois, A., Kouskouni, E., & Iacovidou, N. (2015). A review of carbon dioxide monitoring during adult cardiopulmonary resuscitation. Heart, Lung and Circulation, 24(11), 1053-1061.
Price, P. C., Jhangiani, R. S., Chiang, I. A., Leighton, D., & Cuttler, C. (2017). Research methods in psychology (3rd ed.). New York, NY: The Saylor Foundation.
Ristagno, G., Mauri, T., Cesana, G., Li, Y., Finzi, A., Fumagalli, F., … Latini, R. (2015). Amplitude spectrum area to guide defibrillation: A validation on 1617 patients with ventricular fibrillation. Circulation, 131(5), 478–487.
Ruiz de Gauna, S., Leturiondo, M., Gutiérrez, J., Ruiz, J., González-Otero, D., Russell, J., & Daya, M. (2018). Enhancement of capnogram waveform in the presence of chest compression artefact during cardiopulmonary resuscitation. Resuscitation, 133, 53-58.
Sahyoun, C., Siliciano, C., & Kessler, D. (2018). Use of capnography and cardiopulmonary resuscitation feedback devices among prehospital advanced life support providers. Pediatric Emergency Care, 1-8.
Salen, P., O’Connor, R., Sierzenski, P., Passarello, B., Pancu, D., Melanson, S.,… Heller, M. (2001). Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Academic Emergency Medicine, 8(6), 610-615.
Sandroni, C., De Santis, P., & D’Arrigo, S. (2018). Capnography during cardiac arrest. Resuscitation, 132, 73-77.
Sanjari, M., Bahramnezhad, F., Fomani, F. K., Shoghi, M., & Cheraghi, M. A. (2014). Ethical challenges of researchers in qualitative studies: The necessity to develop a specific guideline. Journal of Medical Ethics and History of Medicine, 7, 14. Web.
Saunders, R., Struya, M., Pollock, R., Mestek, M., & Lightdale, J. (2017). Patient safety during procedural sedation using capnography monitoring: A systemic review and meta-analysis. BMJ Open, 7, e013402.
Sheak, K.R., Wiebe, D.J., Leary, M., Babaeizadeh, S., Yuen, T.C., Zive, D., … Abella, B.S. (2015). Quantitative relationship between end-tidal carbon dioxide and CPR quality during both in-hospital and out-of-hospital cardiac arrest. Resuscitation, 89, 149-154.
Soar, J., Nolan, J. P., Böttiger, B. W., Perkins, G. D., Lott, C., Carli, P., … Adult Advanced Life Support Section Collaborators. (2015). Adult advanced life support. Resuscitation, 95, 100-147.
Stites, M., Surprise, J., McNiel, J., Northrop, D., & De Ruyter, M. (2017). Continuous capnography reduces the incidence of opioid-induced respiratory rescue by hospital rapid resuscitation team. Journal of Patient Safety, 1-10.
Subramani, Y., Singh, M., Wong, J., Kushida, C., Mahotra, A., & Chung, F. (2017). Understanding phenotypes of obstructive sleep apnea: applications in anesthesia, surgery and perioperative medicine. Anesthesia Analgesia, 124, 179-191.
Tobi, K. U., & Amadasun, F. E. (2015). Cardio-pulmonary resuscitation in the intensive care unit: An experience from a tertiary hospital in Sub-Saharan Africa. Nigerian Medical Journal: Journal of the Nigeria Medical Association, 56(2), 132-137.
Turle, S., Sherren, P., Nicholson, S., Callaghan, T., & Shepherd, S. (2015). Availability and use of capnography for in-hospital cardiac arrests in the United Kingdom. Resuscitation, 94, 80-84.
Udod, S., & Wagner, J. (2018). Common change theories and application to different nursing situations. In J. Wagner (Ed.), Leadership and Influencing Change in Nursing (pp. 155-173). Regina, Canada: University of Regina Press.
Valente, M. J., & MacKinnon, D. P. (2017). Comparing models of change to estimate the mediated effect in the pretest–posttest control group design. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 428-450.
Venkatesh, H., & Keating, E. (2017). BET 1: Can the value of end tidal CO2 prognosticate ROSC in patients coming into emergency department with an out-of-hospital cardiac arrest (OOHCA)? Emergency Medicine Journal, 34(3), 187-189.
Watson, R. (2015). Quantitative research. Nursing Standard, 29(31), 44-48.
Whitaker, D., & Benson, J. (2016). Capnography standards for outside the operating room. Current Opinion in Anaesthesiology, 29(4), 485-492.
Wright, S. (2017). The case for procedural capnography. Web.
Wright, S. A. (2017). The case for procedural capnography (DNP Project, Capella University, Minneapolis, MN). Web.
Yen, P. Y., Kelley, M., Lopetegui, M., Rosado, A. L., Migliore, E. M., Chipps, E. M., & Buck, J. (2016). Understanding and visualizing multitasking and task switching activities: A time motion study to capture nursing workflow. In AMIA Annual Symposium Proceedings (pp. 1264-1273). New York, NY: American Medical Informatics Association.
Zito, A., Berardinelli, A., Butler, R., Morrison, S., & Albert, N. (2019). Association of end-tidal carbon dioxide monitoring with nurses’ confidence in patient readiness for postanesthesia discharge. Journal of Perianesthesia Nursing.
Zyphur, M. J., & Pierides, D. C. (2017). Is quantitative research ethical? Tools for ethically practicing, evaluating, and using quantitative research. Journal of Business Ethics, 143(1), 1-16.