Conceptual Model
Bedsores and skin lesions are serious problems that require preventive protection measures and subsequent treatment if necessary. Their occurrence is influenced by various factors, including the quality of medical services and the number of staff members who serve patients with bed rest (Breeded et al., 2018). Creating a database is necessary to collect all factors influencing the occurrence of the problem. Figure 1 provides an example of a future conceptual model addressing the problem of bedsores.
Analysis
Entities in the E-R diagram
The entities will be patients who have developed skin ulcers, pressure, and perforations within the past year. This is the target group whose problem-solving is the nurses’ job and an important entity. Then, an established entity in the form of nursing staff. It falls into two categories, nurses and physicians; its use is justified by the need to understand the role and number of staff in solving the key problem.
Finally, an entity in health status is the health parameters of persons with already developed decubitus. This entity is important because it indicates the preconditions for the development of the problem. Figure 2 provides an E-R diagram.
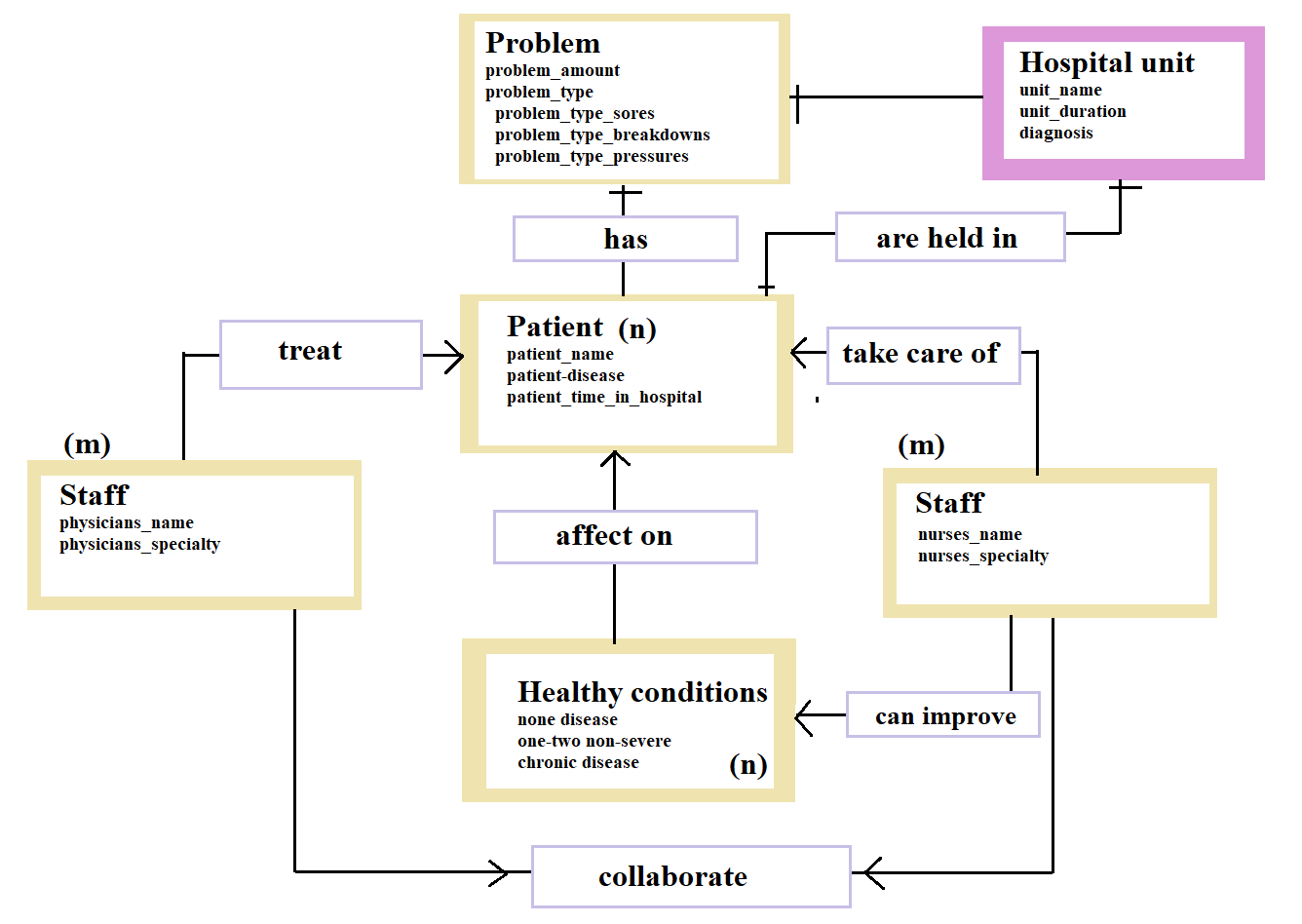
Description of the E-R chart
First, we must consider the relationship between staff (M) and patients (N). Staff directly influence patients’ health, so it is necessary to establish a quantitative relationship between the number of nurses and doctors, patients, and the presence of bedsores and pressure ulcers (Bereded et al., 2018). The ratio of nurses to physicians can also affect patients, so staff are in an unspecified relationship with each other.
Second, some factors are independent of the medical staff and can influence the development of pressure sores. These are expressed in terms of health status (N), which consists of three variations. Healthy people are less likely to become bedsores patients. At the same time, individuals with a single medical condition will have a greater risk of developing bedsores, and those with chronic medical conditions are more prone to bedsores (Al Mutair et al., 2020). Consequently, these correlations explain the premise between a patient’s history and the presence of bedsores.
Third, the relationship between the ward of the hospital in which the patients are held should be taken into account. There can be many such wards: trauma, intensive care, gerontology, cancer ward, and cardiology (Bereded et al., 2018). However, compared to the others, only one will have the most significant relationship with the development of bedsores in patients. This relationship is, in turn, related to health status, which is the intrinsic influence on the development of bedsores.
Questions
- Of the patients admitted in the last year, what percentage developed skin sores, pressure, and breakdowns?
- What is the relationship between the patient-nurse ratio and the likelihood of developing skin breakdowns and pressures?
- What patient health parameters are associated with developing skin sores and pressure ulcers?
Findings
During the work on the future database, a model was developed that considers the study’s key objects. The model indicates the principle of determining the relationships between the objects of the article. The E-R diagram prepared reflects the dependencies between the main entities: doctors, nurses, patients, and health conditions. It also shows the consequences of such dependencies and quantitative relationships, which allows us to evaluate the state of the problem (Al Mutair et al., 2020). A database with data on such relationships will allow the establishment of potential solutions to the problem, its developmental factors, and ways to manage it from different sides.
References
Al Mutair, A., Ambani, Z., Al Obaidan, F., Al Salman, K., Alhassan, H., & Al Mutairi, A. (2020). The effectiveness of pressure ulcer prevention programme: A comparative study. International Wound Journal, 17(1), 214–219. Web.
Bereded, D. T., Salih, M. H., & Abebe, A. E. (2018). Prevalence and risk factors of pressure ulcer in hospitalized adult patients: A single-center study from Ethiopia. BMC Research Notes, 11(1), 847. Web.