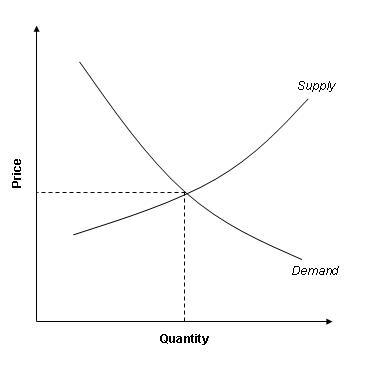
Supply vs. demand is the economic mold of price-fixing and determination; where the amounts needed for purchase and that which the producers or sellers are able to administer to the consumers; level-up to get to a given fixed figure. This model holds that in a market where the conditions of competition are thriving; price will vary to level up the amount of a given product or service, which the producers are capable and willing to supply; and that which the consumers are ready and willing to buy at a given price. The price at which these two quantities which are characteristic with price tension in opposite directions level out at; is basically referred to as the equilibrium price. Within such a market where the conditions are present; it should further be noted that in the case the demand exceeds the supply quantity, prices tend to increase. Further, in the case that the supply quantity exceeds the demand amount, a price drop accompanies the market change (Kleinfeld, 2006).
Medical care on the other hand can be defined as the administration of testing and treatment of patients at a given price. Due to the fact that these services have to be paid for and that not all patients can meet the costs involved especially with the monopolization of the healthcare provider industry; this creates a market status characteristic of profit-maximizing providers and minimal health insurance coverage (Rubin, Altman & Mendelson, 1992).
From research and studies carried out in the U.S, it has been evident that there has been the so-called ‘bed problem’; under which the issue of how to reuse or fill out empty hospital beds is not the issue, but the major issue is that the providers of health care are forced to bent over to the healthcare changes in response. From the recent analysis of the healthcare provision environment within the U.S; it has been indicated that healthcare providers may need to streamline and simplify healthcare provision operations; facilitate emergency handling of healthcare demands, or promote the least expensive environment for the provision of, and delivery of healthcare services. Some of the efforts that the analytical studies provided for; which could help solve the problem at hand include the sharing of healthcare resources like personnel and equipment. In this case, a double usage of these resources will lead to a reduction in the present problems that include the issue of ‘bed problem’ and drug deficiency (Rubin, Altman & Mendelson, 1992).
To be addressed under this study; is the medication required towards the treatment of chronic diseases, which lately have been attributed to the service of bed space. This case recently has been on the increase, especially for the disability and death of 70% of the American population. Among these chronic diseases leading to the death of up to 1.7 million persons each year among the American population are cancer, diabetes and heart-related problems (Rubin, Altman & Mendelson, 1992).
To be reviewed under this study is the high incidence of diabetes mellitus among the American population; which is affecting up to more than sixteen million people currently. It should further be noted that this health problem is rampantly present among Americans; perceived to be on the rise and posing a very heavy burden on the administration and expenditure of the public health allocation. From studies it can be argued that the problem is further on the rise, thus there will be a resultant increased need for preventive, curative and medical measures on the diabetes problem. Some of the signaling factors that lead to the deduction that the problem is on the rise include; the increasing rates of obesity, impaired glucose consumption levels, and the increased take-up of sedentary lifestyles. From studies, it has also been clear that major per-person expenses have been associated with the treatment of diabetic complications; where the trends indicate that death rates among diabetic patients are higher than among non-diabetic ones (Rubin, Altman & Mendelson, 1992).
From the same study, it was also indicated that the provision of healthcare to diabetes patients is less than optimal; therefore there is the need for the improvement of the healthcare provision against this health problem if the problem is to be put under control (Rubin, Altman & Mendelson, 1992).
Some of the factors that can be attributed to the current problem of medication and drug administration to diabetes patients among other diseases include; the conditions explained below. One of the factors leading to this phenomenon is the variedness of patients; which occur due to the absence of insurance plans covering these diseases, and the profit maximization of healthcare providers (Sullivan, 2006).
Another cause for the phenomenon explained; is the changes in the supply of physician availability or the excessiveness of other conditions which promote the deficiency of staff in personnel administration. Based on the problem of personnel shortage discussed; it should further be noted that the current number of five million healthcare professionals serving in the U.S is already deficient; as they are to a great extent not capable of meeting the needs of the current population. Further; according to projections based on research and analysis of the healthcare provision environment in the U.S today; it is clear that by the year 2020 there will be a shortage of 200,000 physicians and one million nurses serving the people of the U.S; therefore making it conclusive that the situation is only getting worse than it currently is (Sullivan, 2006).
Further, the high intake of manufactured chemical-filled foods and the high levels of pollution present within the environment; further makes the problem acute as it increases the instances of obesity which is directly linked to the instance of Diabetes. The American society further makes the affordability of diabetes drugs difficult, as it is rather cumbersome to receive insurance coverage from an employer or healthcare plan; once you are diagnosed with Diabetes especially type two. In the case that a diabetes patient is to receive insurance coverage, then the associated premiums to be paid or associated are too high; which often discourage the enrolment into health insurance plans which further leads to the inability to afford these medications, or having to pay for their costs from personal savings (Rubin, Altman & Mendelson, 1992).
From research, access to ‘clinical endocrinologists’ in the U.S has become a rampant problem facing patients seeking appointments. As a result, this situation has led to an increased cost and difficulty in accessing the care required to keep diabetes under control; as was noted in the New York Times recently (Kleinfeld, 2006). Based on this information, it is absolutely clear that since there are no significant improvements in the access to the practitioners and resources; the supply of these services will further become compromised making many individuals not access diabetic healthcare (Kleinfeld, 2006).
The cost of accessing the healthcare-related to healthcare can be argued out; using the case of a study carried out to estimate the costs involved in administering the healthcare-related to diabetes. According to the study, it was also clear that; U.S dollars 4720 million were used on hospitalization, 1012 million on consultations; and 2508 on consolations among other related expenses. This case was carried out among the diabetes patients of the Caribbean and Latin American districts. From the analysis given above; it is clear and evident that the cost of managing diabetic patients is so high, which simply leads to the inability to supply more than the already supplied healthcare in many areas (Rubin, Altman & Mendelson, 1992).
Based on the explanation given above on the accessibility, costs, and the potential supply of diabetes medication; it is clear that the supply of these drugs and the services related to diabetes medication is limited as compared to the high instances of diabetes. As it is, the instance is further worsened by the high rates of a sedentary lifestyle, environmental pollution and imbalanced diet patterns which are caused by modern lifestyles. Thus based on this rationale, it is clear that the costs of diabetes management and healthcare will continue to rise; as the virtual supply diminishes (Branson & James, 1976).
The Demand-Supply curve within this area of healthcare provision will be like the one shown below.
Reference list
Branson, W. and James, M. (1976). Macroeconomics. New York: Harper Publishers.
Kleinfeld, N. (2006). Diabetes and its awful toll quietly emerge as a crisis. New York: New York Times.
Rubin, R. Altman, W. & Mendelson, D. (1992). Health care expenditures for people with diabetes mellitus, Journal of Clinical Endocrinology and Metabolism.
Sullivan, J. (2006). As diabetes rises, doctors’ numbers fall. Philadelphia Inquirer.