Case Background
Sarah is a 42-year-old professional teacher married with children of ages six and one year. She has been having a depressed mood, anxiety, crying, and feeling of worthlessness. The symptoms made her school give her an off, during which she was prescribed some antidepressants that proved ineffective. Despite stating that she finds value in heling others, she is exhausted from taking care of her father-in-law and children without assistance from her husband. Moreover, her work is monotonous, and she rarely finds time for self-care and friends.
Formulation
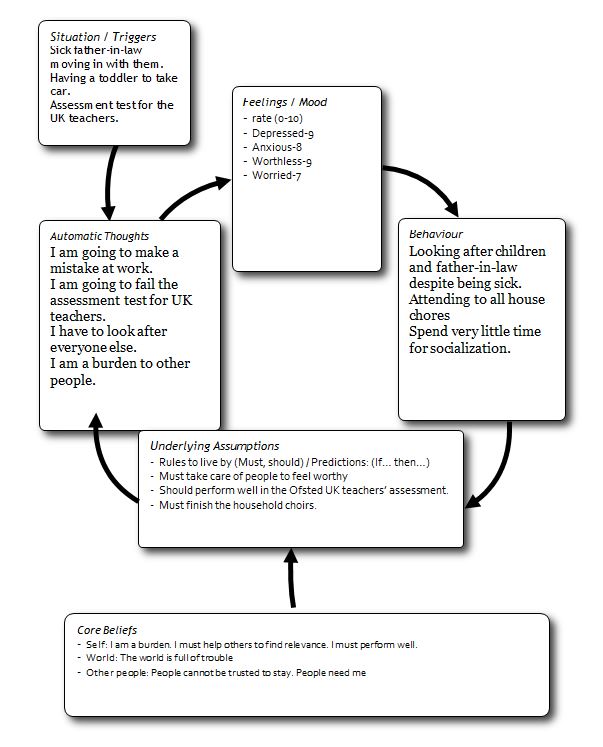
Factors Contributing to the Problem
Life Experience
One of the factors contributing to the problem is a traumatic childhood experience where her mother became sick and died while she was staying with her aunt, and soon after, the father left and rarely kept in touch with her. According to Humphreys (2018), when children lack a nurturing and committed caregiver, they may have social difficulties, internalize psychopathology and have cognitive and language deficits. Sarah believes that since she was abandoned, she is a burden and must work for others to be worthy. Thus, when she fails, she starts feeling worthless and possibly worried about being left.
Social
Her husband is not helping her with caring for their toddler and father, which leaves her with the significant burden. Moreover, she has challenges achieving a work-life balance due to many responsibilities both at school and at home. Burnout is common for informal caregivers who often feel fatigue and cannot complain because of a sense of responsibility to care (Gérain & Zech, 2019). The other challenge is that she rarely has time to go out with friends who help in improving her mood.
Psychological
There is a possibility that Sarah is experiencing postpartum depression, which often occurs in women after childbirth. Noteworthy, Sarah is depicting related symptoms such as crying, anxiety, worry, feeling of worthlessness, and a low mood (Bauman et al., 2020). Lack of time with her husband is further exacerbating her symptoms because she has no person to share her burden. The loss of her mother may, and abandonment by her father may have been traumatic, causing her to develop attachment problems.
Strengths, Capabilities and Resilient Factors
Personal Factor
Sarah explains that she loves and enjoys being a teacher despite the challenges that she has been having. In addition, she loves being a mother and is compassionate towards other people, which implies that she can overcome her depression. In addition, she has gone through challenging experiences like the death of her mother in the past, and she managed to survive and find a positive reason to offer selfless service for others. The ability to bounce back from hardship is an important skill in life since resilience develops over time (Hurley, 2019). The implication is that Sarah has, over the years, developed a capacity to overcome her troubles and continue pursuing her dreams.
Social Factors
Sarah is married to a good man whom she loves, and the relationship has been good except recently when each of them became preoccupied with their busy schedule. As stated by Becker et al. (2018), communication is a very important tool in the relationship between employees and spouses. If Sarah’s husband is a good man, then it is apparent that if told the plight of his work, he will understand and offer to assist her with some caregiving roles. Moreover, Sarah’s school appears to be understanding as they even allowed her to go for leaf when she was showing symptoms of psychological conditions. Her friends are another positive influence as each time she sees them brings positive moments in her life.
Psychological Needs
Sarah has a psychological need for unconditional love and a sense of belonging where she will be appreciated for who she is rather than what she can give. She needs to feel that she is important and enough by virtue of being human. In addition, Sarah has a psychological need for safety since she was separated from her parents and her aunt made her appear as a burden leading to the development of dysfunctional thought patterns. Noteworthy, many family caregivers suppress their feelings when tired because they feel guilty admitting that caring for a loved one is taking a toll on their social and personal life (Merlo et al., 2020). Sarah needs to be told that her feelings are valid so that she can express her frustrations instead of suppressing which cause more psychological harm.
Treatment and Management Options
Option One
Tell Sarah to take a break from all her caregiving roles and focus on self-care as other people take over the work that she has been doing. The rationale is that one of the dysfunctional thought patterns that she has is finding value and self-worth in selfless service to others. Sarah needs to know that she is enough and does not have to burden herself to the point of mental breakdown. Moreover, burnout is a common issue with family caregivers due to exhaustion (Gérain & Zech, 2019). Her husband can help her with the task, or she can ask her friends to help her out as she recovers.
The suggestion upholds the principle of integrity, which requires being honest with the client to expose the root cause of malfunctioning behavior and psychopathology. By telling Sarah to take a rest and restructure her mindset on self-worth, the focus of the intervention is patient-centred. In addition, it upholds the principle of responsibility Medical health practitioners have an obligation to advocate for what is best for the client. For Sarah, taking a break from all her caregiving role will allow her to rest and enhanced self-esteem.
Option Two
Ask her to learn and practice relaxation therapy to help calm down her nerves when feeling anxious or depressed. According to Jia et al. (2020), relaxation techniques are comparable to psychotherapy in the level of effectiveness in alleviating depressive symptoms. Notably, when people are afraid or stressed as is common for depression and anxiety episodes they are likely to experience muscle tension and psychosomatic disorders. Such symptoms can be lowered through progressive muscle relaxation where the patient tense up specific muscle and slowly relax them in a consistent and rhythmic manner (Jacob & Sharma, 2018). The method is effective and can help in slowing down though process and being in charge of the situation.
The ethical principle that the management upholds is competence. The relaxation technique is a proven CBT technique for curbing depression. Based on the symptoms depicted by Sarah it is clear that she is depressed. Moreover, it demonstrates respect because it offers a solution by asking the client to think of taking a different regime and not forcing her.
References
Bauman, B. L., Ko, J. Y., Cox, S., D’Angelo, D. V., Warner, L., Folger, S., Tevendale, H. D., Coy, K. C., Harrison, L., & Barfield, W. D. (2020). Vital Signs: postpartum depressive symptoms and provider discussions about perinatal depression — United States, 2018. MMWR. Morbidity and Mortality Weekly Report, 69(19), 575-581. Web.
Becker, W. J., Belkin, L., & Tuskey, S. (2018). Killing me softly: Electronic communications monitoring and employee and spouse well-being. Academy of Management Proceedings, 2018(1), 1-7. Web.
Gérain, P., & Zech, E. (2019). Informal caregiver burnout? Development of a theoretical framework to understand the impact of caregiving. Frontiers in Psychology, 10(1), 1-12. Web.
Humphreys, K. L. (2018). Future directions in the study and treatment of parent–child separation. Journal of Clinical Child & Adolescent Psychology, 48(1), 166-178. Web.
Hurley, K. (2019). What is resilience? Definition, types, building resiliency, benefits, and resources. EverydayHealth.com. Web.
Jacob, S., & Sharma, S. (2018). Efficacy of progressive muscular relaxation on coping strategies and management of stress, anxiety and depression. The International Journal of Indian Psychology, 6(1), 106-124. Web.
Jia, Y., Wang, X., & Cheng, Y. (2020). Relaxation therapy for depression. Journal of Nervous & Mental Disease, 208(4), 319-328. Web.
Lynch, S. H., Shuster, G., & Lobo, M. L. (2017). The family caregiver experience – examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging & Mental Health, 22(11), 1424-1431. Web.
Malhi, G. S., Morris, G., Bell, E., & Hamilton, A. (2020). A new paradigm for achieving a rapid antidepressant response. Drugs, 80(8), 755-764. Web.
Merlo, E., McNabney, S., Frisone, F., Sicari, F., Paunica, M., Motofei, C., & Settineri, S. (2020). Compassion and suppression in caregivers: Twin masks of tragedy and joy of caring. Journal of Mind and Medical Sciences, 7(1), 61-68. Web.
Sabo, K., & Chin, E. (2021). Self-care needs and practices for the older adult caregiver: An integrative review. Geriatric Nursing, 42(2), 570-581. Web.