Diabetes is a challenging condition that requires careful monitoring and constant action to support health, ensure a normal standard of living, and prevent complications. The number of adult patients living with diabetes is constantly increasing and is expected to grow to 629 million by 2045, compared to the recent 425 million (Nikitara et al., 2019). The risk of hospitalization for patients with diabetes is 3.5 times higher than for people without such a condition (Nikitara et al., 2019). If mismanaged, diabetes can lead to heart disease, kidney disease, retinopathy, and leg wounds (American Diabetes Association [ADA], 2022). Given the danger of such a condition and the importance of managing it effectively, patient education and coordination of efforts to support them become critical tasks for personnel diagnosing diabetes.
Nurses can make a significant contribution by offering workflow improvements, as their effectiveness enhances the provided services’ quality. McBride and Teitz (2022) suggest using diagrams to create workflow maps and find improvement opportunities. This paper offers a map for coordinating an education plan and resources for a person newly diagnosed with adult-onset diabetes. The process requires attention to many details, is therefore complex in implementation, and requires constant refinement.
Creating a map requires understanding the process and highlighting key roles and actions that medical personnel need to take. Critical specialists involved in patient education following diagnosis of diabetes include primary care physician (PCP), nurse, diabetes specialist nurse (DSN), and nutritionist. They can also give referrals to other specialists whose involvement will be required in the future for regular screenings – podiatrists, ophthalmologists, dentists, mental health specialists, and fitness specialists (ADA, n.d.). Each expert has their responsibilities in the process of teaching patients.
After receiving the results of analyses confirming diabetes, the nurse orders additional tests to be performed to establish the type of diabetes. The specialist also checks for comorbid conditions, studies medical history to assess risks, develops a treatment plan and creates referrals to DSN and the nutritionist. Based on patient assessment, the PCP highlights what resources need to be mobilized, which specialists to visit, and includes prescriptions for necessary drugs. The nurse manages the patient’s information in the electronic health record (EHR) and, after confirming the type of diabetes, offers the patient the necessary training programs.
The DSN provides patient training following the national standards of diabetes self-management education and support (DSMES). DSN also introduces the patient to the roles of specialists involved in managing the condition, describes the patient’s actions, and offers the necessary educational materials. The patient also consults with a nutritionist, who teaches the essential changes in eating habits. After initial coordination of resources and training efforts, the patient must enter a care routine but may require additional assistance from other professionals. Figure 1 presents the map of the described process of coordinating resources and education.
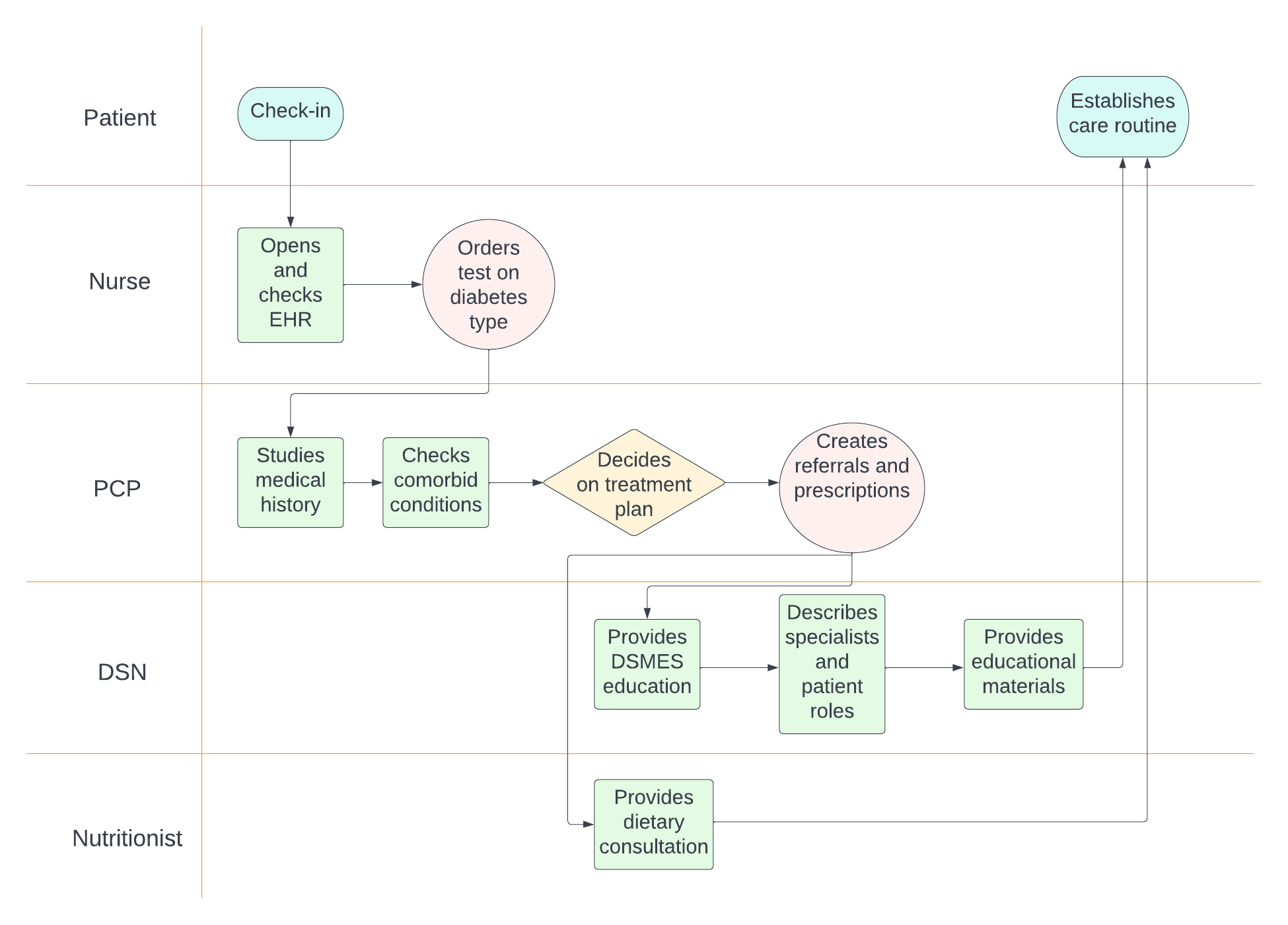
The chart provides an opportunity to explore better the process of coordinating patient education. Notably, the process relies heavily on creating referrals and orders. This aspect may be disrupted by external variables: EHR malfunctioning or the patient’s unwillingness to visit other specialists. To solve the problem, specialists can agree on the appointment time with the patient when creating a referral. Another potential problem is the internal variable – the lack of time; for example, the DSN may not be able to take another patient. In this case, the nurse must also be able to provide the education or choose another specialist. Finally, another challenge is the quality of educational materials, as their complexity often becomes a barrier to diabetes management. The materials must be understandable to patients with different education levels and available in print and electronic form.
Thus, creating a workflow diagram can be a valuable tool for finding weaknesses and opportunities for improvement. Such a map shows the process dependencies, variables, assigned roles, and the necessary actions. The current paper presented a chart of the coordination of the educational process for patients with newly identified diabetes. Its study suggests possible problems with referrals, personnel’s lack of time, and the quality of educational materials.
References
American Diabetes Association. (2022). Standards of medical care in diabetes-2022: Abridged for primary care providers.Clinical Diabetes, 40(1), 10–38. Web.
American Diabetes Association. (n.d.). Get to know your diabetes care team. Web.
McBride, S., & Teitz, M. (2022). Nursing informatics for the advanced practice nurse: Patient safety, quality, outcome, and interprofessionalism. Springer Publishing Company.
Nikitara, M., Constantinou, C. S., Andreou, E., & Diomidous, M. (2019). The role of nurses and the facilitators and barriers in diabetes care: A mixed methods systematic literature review.Behavioral Sciences, 9(6), 1-16. Web.