Introduction
Diabetes is one of the commonest conditions affecting many people in different parts of the world. This medical illness interferes with the body’s capability to control and process the amount of glucose in the blood. Patients who do receive adequate support and management will record increased levels of blood sugar. Such individuals will be at risk of developing new complications, such as cardiovascular disease and stroke. This essay gives a detailed analysis of diabetes and how it impacts cardiovascular and nervous systems and oral health. The presented insights and concepts can guide many people to understand the nature of this complication and manage it effectively.
Diabetes: Background
The common hypothesis among many people is that being overweight or obese is the leading risk factor for diabetes. Such a condition can emerge or occur during childhood. A proper understanding of the nature of this illness can guide and empower many patients and guardians to manage it successfully. Three types of this condition are known to affect many people across the world. These include type 1 diabetes, gestational diabetes, and type 2 diabetes (see Figure 1). The first type is also called “juvenile diabetes” and it occurs when the body of an individual is incapable of producing insulin (Wang et al. 2501). Patients affected by this condition should get daily intakes of this substance to stay healthy and alive.
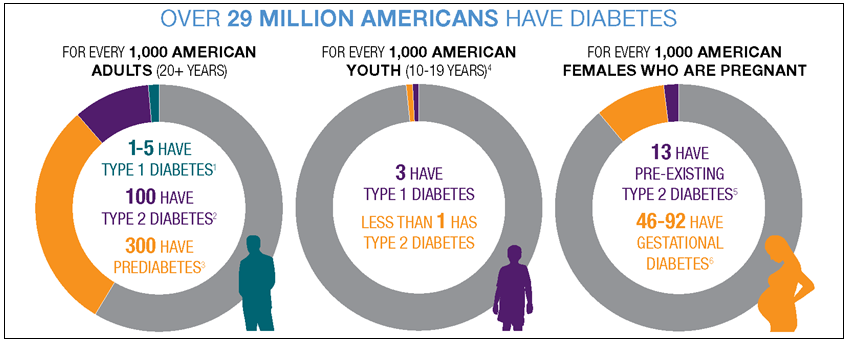
In type 2 diabetes, the body is not able to utilize the available insulin effectively. The relevant cells might be unable to respond perfectly or efficiently to the available or produced insulin. This type affects the greatest number of people across the world (Petrie et al. 581). Gestational diabetes is usually common in women during pregnancy (see Figure 2). Affected individuals will be insensitive to the produced insulin. Such kind of a condition will naturally resolve itself after birth.
Prediabetes is a common condition that is currently affecting many people in the United States. According to Messerli and Grossman, it will trigger the development of type 2 diabetes if the affected individual fails to receive adequate or timely support within 4-5 years (e11). The latest statistics by the Centers for Disease Control and Prevention (CDC) reveal that over 100 million American adults are either living with diabetes or prediabetes (Malone 356). Currently, studies have revealed that 30.8 million citizens in the United States have diabetes while around 84 million are affected by prediabetes. Within the past two decades, the diagnosis for different diabetes types has remained steady in this country (Moningi et al. 581). New research by Malone revealed that citizens living in urban areas were affected the most by this condition (355). Native Americans, African Americans, Asian Americans, and Latinos tend to have increased chances of developing this condition.
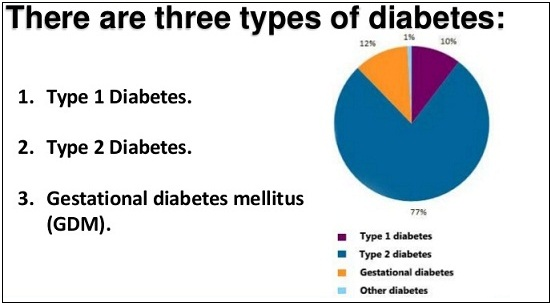
Some statistics have indicated that obesity is a major illness that requires evidence-based intervention measures. From the year 1990 to 2010, the number of people affected by diabetes has tripled (Moningi et al. 579). Age has emerged as a major factor associated with the development of type 2 diabetes which affects around 95 percent of all patients (Moningi et al. 581). The first type affects less than 5 percent of the affected population (Petrie et al. 582). Some of the potential causes of this condition include high blood pressure, excessive body fat, age, and the presence of gestational diabetes.
Patients can manage this condition through the use of a proper diet, physical activity, and getting adequate insulin to control the level of blood sugar in the body. Individuals suffering from this medical condition are usually at risk of developing various diseases and health complications, including heart disease, kidney failure, amputation of feet and legs, premature death, and vision loss (Matheus et al. ID 653789). These issues explain why a multifaceted approach is needed to manage this illness and make it possible for more people to achieve their potential.
How Diabetes Impacts Cardiovascular and Nervous Systems
Cardiovascular System
Researchers have observed that there is a correlation between diabetes and cardiovascular disease. For instance, Wang et al. indicate that around 68 percent of all patients with diabetes and aged 65 years of age or more die from some kind of heart disease (2501). Petrie et al. go further to argue that 16 percent of such individuals will be affected by stroke (581). Adults who have this condition have increased chances of suffering from heart disease. Although diabetes is manageable and treatable, elevated levels of glucose in the body increase the chances of developing stroke and different types of cardiovascular diseases. Type 2 diabetes is a serious health condition that triggers various events. Such occurrences eventually result in the development of cardiovascular disease.
The first one is the increased levels of blood pressure or hypertension. Messerli and Grossman indicate that this condition is a leading risk factor for heart disease (e11). When the body experiences insulin resistance, the problem of hypertension worsens and eventually increases the risk of cardiovascular disease. This issue explains why proper management of type 2 diabetes can reduce this challenge and improve the health outcomes of more people. The second consideration when examining the correlation between cardiovascular disease and diabetes is that of abnormal levels of triglycerides and cholesterol (Moningi et al. 581). Unhealthy quantities of these compounds result in poor lipid count (Petrie et al. 581). Affected persons will have higher chances of developing coronary challenges or diseases. Lipid disorder can occur and affect the body’s ability to pump blood successfully to different parts.
Obesity and diabetes are conditions that can be found simultaneously in a given patient. These illnesses are known to increase the risk of the development of cardiovascular disease. The high level of insulin resistance affects the flow of blood in the body. This health problem can trigger increased blood pressure and creating a new opportunity for the development of cardiovascular disease (Messerli and Grossman e11). The introduction of weight loss programs can reduce the risk for the condition and increase the body’s ability to use insulin. Such measures will ensure that the targeted patient does not develop hypertension and cardiovascular disease.
Some specific aspects or factors increase the chances of heart illnesses in individuals affected by diabetes. For instance, those who smoke will affect the flow of oxygen in the blood and trigger hypertension. Such individuals will complicate the common conditions associated with diabetes and eventually trigger the development of cardiovascular disease (Messerli and Grossman e11). Those who fail to control their blood sugar levels will also be exposing themselves to this kind of complication. The impaired cardiovascular system will affect the overall health of the patient and eventually result in premature death. These aspects or arguments explain why there is a need for all stakeholders to consider evidence-based strategies for addressing the challenges associated with diabetes and managing it successfully.
Nervous System
The human nervous system plays a critical role in delivering and coordinating electrical impulses, thereby making it possible for organs to communicate effectively with each other. The brain is what offers the processing ability to ensure that the acquired or relayed information is understandable. This system guides physical and emotional responses throughout the body (Malone 356). Through it, people can monitor and deduce useful data from what is happening around them and act appropriately. Such responses might be automatic or deliberate depending on the acquired or recorded impulses.
The occurrence of diabetes can affect the nervous system and make it impossible for the patient to achieve his or her goals. Due to the presence of this condition, the blood vessels in the body that usually support the nerves will become incapacitated or damaged. This kind of destruction will affect or distort the rate at which electrical impulses from one organ are relayed to another. When this problem occurs, chances are high that the individual’s feeling ability will be distorted. Sustained or prolonged damage will affect most of the organs that communicate with the brain and make it impossible for every patient to achieve his or her aims in life.
The obliteration of various nerves in the body can trigger a condition called diabetic neuropathy. This occurs when different parts of this system are incapable of relaying the right information and in a systematic manner (Sowers et al., 1056). Some of the organs that will be affected by this illness include those responsible for respiratory and digestive activities. Some of the common types of the identified condition include sensory neuropathy, autonomic neuropathy, and motor neuropathy (Moningi et al. 580). A study by Malone showed that around 50 percent of all patients with type 2 diabetes had a specific kind of neuropathy (356). This is a clear indication that health professionals and community members should consider and propose superior measures or strategies for overcoming the possible challenges associated with diabetes and ensuring that more patients record positive results.
Due to nerve damage, the feet become more sensitive in persons with diabetes. The loss of sensitivity triggered or caused by this condition explains why amputation is common among patients with diabetes. Those who suffer from this disease should also be keen to check their feet regularly to overcome such a problem. Peripheral neuropathy is quite common and affects the legs and the feet. It can later occur in the arms and hands. The major signs include cramps and sharp pains, numbness, increased sensitivity, foot problems, loss of coordination and balance, and muscle weakness (Malone 356). Autonomic neuropathy will affect the patient’s eyes, sex organs, bladder, heart, and stomach. The common symptoms associated with it include constipation, sweating problems, vaginal dryness, body temperature changes, bloating, loss of appetite, and bladder issues.
The nature of this complication associated with diabetes explains why people should monitor their blood sugar levels and pressure regularly. This is the case since nerve damage can distress different organs and body parts, thereby disorienting the patient’s quality of life (Wang et al. 2500). Those who have neuropathy will experience numbness and pain in their legs and have problems with their blood vessels, urinary tract, heart, and digestive system.
How Diabetes Impacts Oral Health
Diabetic patients tend to have increased chances of developed various oral health problems. Those who fail to control this condition effectively will be at a higher risk of recording numerous challenges that can affect the overall quality of their lives. People who are above the age of 50 should take this issue seriously since they have increased chances of experiences additional dental health problems (Kaur et al. 74). This means that people who are older but do not have this medical condition should monitor their oral hygiene properly and promptly.
Uncontrolled diabetes is a leading contributor to increased sugar and glucose levels in the body systems and fluids. This means that the patient’s saliva will be capable of attracting different types of bacteria. Wang et al. reveal that such organisms thrive on sugar (2500). They digest or break it down, thereby producing a strong acidic compound that is capable of damaging the teeth (Mauri-Obradors et al. e588). Such bacteria will multiply very fast and feast on different food materials in the mouth to form a dangerous compound called “plaque” (Wang et al. 2500). This subsequent composite will eventually result in gum disease and tooth decay. This health challenge explains why these conditions continue to affect the oral health of many patients with diabetes.
The first condition of the mouth is called periodontitis that is common in many patients with diabetes. This dental disease usually results from poorly managed gingivitis. Periodontitis is identified as a common but complicated disease of the gums that result in the loss of the tissue and bone known to support a person’s teeth (Wang et al. 2501). If poorly managed or treated, the affected individual might eventually become toothless, thereby being unable to eat different food types.
The problem of saliva production has continued to be experienced or recorded in many people with diabetes. For instance, Petrie et al. argue that older patients with this disease tend to have slowed production of saliva (580). This challenge results in a dry mouth and triggers a condition called xerostomia (Petrie et al. 580). With low quantities of saliva, bacteria multiply in the mouth rapidly and eventually result in various complications. For instance, mouth ulcers and sores will occur if xerostomia is left untreated. When the condition worsens, the affected individual might suffer from gum disease and tooth decay.
On top of bacterial infections, fungi and other organisms are recorded in patients with diabetes. This is the reason why additional oral diseases will affect most of these individuals. For instance, a thrush is a common form of oral yeast infection common in many diabetic patients. This disease is characterized by red or white patches on the tongue (Petrie et al. 581). It can also be observed in the cheeks and might eventually become open sores. These cause discomfort and affect the experiences of the affected individual.
Thrush is common in diabetic patients who wear dentures, take antibiotics, or smoke. The presence of sugary saliva and food materials in the mouth will worsen the situation and trigger numerous complications. This is a clear indication that diabetes is a common risk factor for different oral diseases or infections (Wang et al. 2500). Fungal infections of the mouth will occur in many patients who have this condition.
Burning mouth syndrome can occur in individuals who have high blood pressure and diabetes. This disease is usually related to the presence of a dry mouth and thrush (Mauri-Obradors et al. e590). Some patients experience tingling pain or numbness in their mouths. When left untreated, the affected individuals will be unable to taste different foods properly. Some patients might decide to add sugar into their drinks to overcome this problem. Unfortunately, such kind of behavior will increase the chances of developing additional complications, such as gum disease and cavities.
Finally, those who have this condition will observe their oral wounds take longer to heal. The situation will worsen in individuals who are above the age of 65 (Kaur et al. 75). Different experts and dentists encourage people to take good care of their mouths and seek the right support or care whenever necessary. They should also check the level of blood sugar, brush regularly, and rinse the mouth with antiseptic. They ought to manage all aspects of diabetes effectively to record positive oral health outcomes.
Conclusion
The above discussion has identified diabetes as a major condition that affects millions of people in the United States and across the world. Type 2 diabetes is the commonest and remains a major risk factor for other illnesses, including cardiovascular disease, stroke, hypertension, nerve neuropathy, and poor oral health outcomes. The analysis has linked this condition to a wide range of dental and gum diseases that diabetic patients should address using evidence-based measures. The government should be ready to offer adequate guidelines and resources to manage this illness and ensure that more people record positive health outcomes.
Works Cited
Kaur, Sandeep, et al. “Oral Health Management Considerations in Patients with Diabetes Mellitus.” Archives of Medicine and Health Sciences, vol. 3, no. 1, 2015, pp. 72-79.
Malone, John I. “Diabetic Central Neuropathy: CNS Damage Related to Hyperglycemia.” Diabetes, vol. 65, no. 1, 2016, pp. 355-357.
Matheus, Alessandra S., et al. “Impact of Diabetes on Cardiovascular Disease: An Update.” International Journal of Hypertension, vol. 2013, Article ID 653789.
Mauri-Obradors, Elisabet, et al. “Oral Manifestations of Diabetes Melittus: A Systematic Review.” Medicina Oral Patologia Oral y Cirugia Bucal, vol. 22, no. 5, 2017, pp. e586-e594.
Messerli, Franz H., and Ehud Grossman. “Diabetes, Hypertension, and Cardiovascular Disease: An Update.” Hypertension, vol. 38, vol. 3, 2001, p. e11.
Moningi, Srilata, et al. “Autonomic Disturbances in Diabetes: Assessment and Anaesthetic Implications.” Indian Journal of Anaesthesia, vol. 62, no. 8, 2018, pp. 575-583.
Petrie, John R., et al. “Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms.” The Canadian Journal of Cardiology, vol. 34, no. 5, 2018, pp. 575-584.
Sowers, James R., Murray Epstein, and Edward D. Frohlich. “Diabetes, Hypertension, and Cardiovascular Disease: An Update.” Hypertension, vol. 37, no. 4, 2001, pp. 1053-1059.
Wang, Cecilia C., et al. “Clinical Update: Cardiovascular Disease in Diabetes Mellitus.” Circulation, vol. 133, no. 1, 2016, pp. 2459-2502.