Introduction
Morale is a very important factor for good employees’ performance. It is well known that workforce that exhibit high morale is motivated to work hard and the verse versa is true. This research investigates the factors that affect the morale of employees in a workplace. In realizing the objective of the study, the researcher investigates the morale of the nurse who works in the Rural and Remote Communities of Canada. The researcher used his/her classmates as the participants.
Background Study
It is generally accepted that motivating the workforce makes employees to broaden their skills in order to address the rising organizations demands. Motivated employees are empowered to volunteer to accomplish more work than they have been assigned. The Two- Factor Theory of Fredrick Herzbur explains how motivation is important to enhance the morale of the employees and in particular the nurses working in harsh conditions like those found in the rural and remote areas of Canada (Jishi, 2009: Montour , Baumann , Blythe & Hunsberger , 2009).
Leadership, teamwork, autonomy, support, transparency and change management are considered as vital ingredients for healthy working conditions. Yet, what happens if one, some or all of these are missing? Who is affected and to what extent?
It is imperative for leaders to understand and address these concerns when there are signs and symptoms of a less than optimal morale among the practicing masses. Morale is often touted but seldom clearly defined as a necessary factor to workplace success. Understanding the perceptions, perspectives, definitions and opinions of morale and its implications will enable leaders to address the issues that in turn will potentially increase productivity and optimize patient care.
Problem Statement
The issue of low morale amongst nurses is prevalent worldwide and is no different in the remote and rural communities of Canada. Low morale results in dissatisfied employees and consequently, provision of poor healthcare. There is need therefore to identify the causes of low morale amongst nurses in remote and rural communities in Canada, so that remedial measures can be taken.
Purpose of the Study
The purpose of this study is to explore the opinions and experiences of the nursing staff about workplace morale.
Aims of the Study
The chief objective of this research is to identify the experiences and attitudes of group and class members toward morale and job satisfaction.
Research question
To realize the objective of this research, the researcher used the following question to guide him/her in the research process.
Overview
Durham (2010) argues that there are numerous ways in which organizations can adapt to motivate their employees so that to uplift their morale, but majority of these organizations do not use them. He posits that their failure to use them is the major cause that makes them incur a lot of expenses in terms of medical expenses and high absenteeism of employees.
Durham (2010) recommends employers to establish a working environment that rewards performance, promotes morale and an environment that the workers feel comfortable working in. some of the factors that Durham (2010) suggests that affect workforce morale include leadership, autonomy, Support, teamwork and change management.
Communication
The management should ensure that there is an effective communication across all levels. This is because if the workforce realizes that there are communication barriers between them and the management, they become resentful. The managements should organize regular meetings with their workforce to inform them about the organizations progress and alert them of any impending change so that they are psychologically prepared for it.
In addition, the management should encourage their employees to freely express their opinions. This greatly improves the morale of the workforce significantly and ensures an environment that is conducive for working for the employees and their leaders. Free communication enables the workforce feel more valued in their organization since their inputs are considered, unlike in situation where they are always commanded on what to do (Durham, 2010).
Support
Employees require to be supported adequately so that they are successful in executing their duty accordingly. To empower them appropriately, the management should provide training programs to supplement their skills. Offering training opportunities to the workforce ensures that the employees feel more valued and these training help them to progress in their carriers. The management should ensure that they consult the employees concerned adequately before commencing them so that to enhance the effectiveness of these trainings. Provision of training programs guarantees long-staff retentions.
Team Work
Team work is very important in every organization. The management should ensure that they are successful in establishing effective teams within their organizations so that to maximize their performance. Teams enhance performance since members who belong in one team are in a better position to understand their colleagues in their teams and thus assist them accordingly (Hayes, Bonner & Pryor, 2010).
Motivation
As noted earlier, motivation is considered as a vital factor in ensuring the morale of the workforce is high. To elucidate its importance, the researcher will use the Fredrick Herzburg Two-Factor Theory. The theory is split into two; the hygiene factors and motivators. The theory is based on explicating the factors that inspire people through identifying and satisfying their desires, needs and the objectives pursued to meet these needs (Hardy, 2009).
The hygiene factors comprise of the organizations policies, working conditions, supervisions, salary, safety and job security. The employees are highly productive and their morale is high when the hygiene factors are addressed by the management. When the management fails to honor them, for example when the employees are not well paid, the working conditions are not conducive or are not happy with their supervisor, their morale is low and their performance is affected negatively.
The motivators are considered as those factors that are intrinsic to the work. They include achievement, promotions, growth and participation. Motivators are regarded as the factors that encourage the employee to put extra effort. Concentrating on the hygiene factors is not enough to ensure more job satisfaction. The management should enrich jobs by assigning the workers challenging opportunities and responsibilities.
Methodology
The research will use both primary research and secondary research. The secondary research will include review of literature on the factors that affect employees’ morale. The review will be conducted from relevant books, journals and articles. The researcher will in addition conduct a primary research to complement the findings of the secondary research. The primary research entails two sections.
The section referred as Lab1 which is qualitative in nature and follows a phenomenological method of inquiry with the lab group as the focus group participants. Discussions were aimed at attempting to comprehend the participant’s definition, experiences and contributing factors to workplace morale. At this stage, the research morale was defined as a personal state of emotional phenomena that is closely linked and influenced by group activity (Leedy & Ormrod, 2010).
Sample
The sample used for this study was the lab group participants. Due to complications, there were only two participants in the focus group study. In a focus group phenomenological study, there is customarily a limited number of participants, 5-25 in order to deeply explore the thoughts and opinions of the participants (Cresswell, 2003).
Assessment instruments
The Primary Investigator (PI) could be viewed as the main instrument in this study with the survey questions as the main tool. The responsibility of the PI is to maintain the integrity of the data, conduct the research and basically assume full responsibility for the research project (Purdue University, 2008). The tool developed for this study was a selection of 4 open ended questions. Due to the limited number of participants there is some question as to whether sufficient depth or saturation of the data was met.
Procedure
Prior to initiating the study it was decided that the participants would contribute their discussions in an email format to facilitate data coding and development of data essence descriptions (Cresswell, 2003). Informed consent was obtained verbally from each participant. A semi-structured interview technique was employed by the PI to elicit responses using initial opening remarks to explain the study.
The principal investigator was also a participant in the interview process and was the first to answer questions so as not to be influenced by other participant responses. Once all questions were answered the participants were asked to expand and/or clarify responses that were vague or unclear. Responses were coded and similar themes were identified.
Ethical Considerations
Before commencing the interview, the participants were assured that the data collected will only be used purposely for this research study. They were also assured of confidentiality of the information they will give.
Analysis
For the qualitative data, the data collected from the respondents was recorded in tables and relevant inference realized by the use of thematic. The quantitative data collected was first coded and then analyzed using the SPSS and Excel applications.
Results
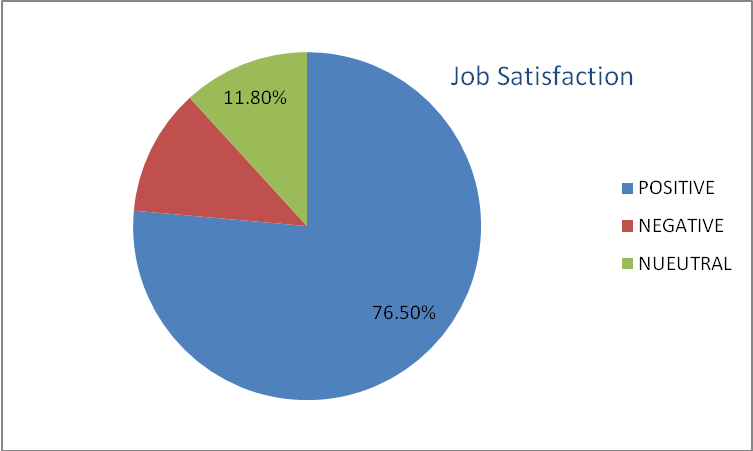
The thematic cited that the major source of employees satisfactions were; lack of team work, dissatisfaction, poor management, lack of support and poor communication. Lab 2 that comprised of a quantitative analysis of the survey response indicated that 5.9% and 76.5% strongly agreed and agreed respectively that they were satisfied with their job.
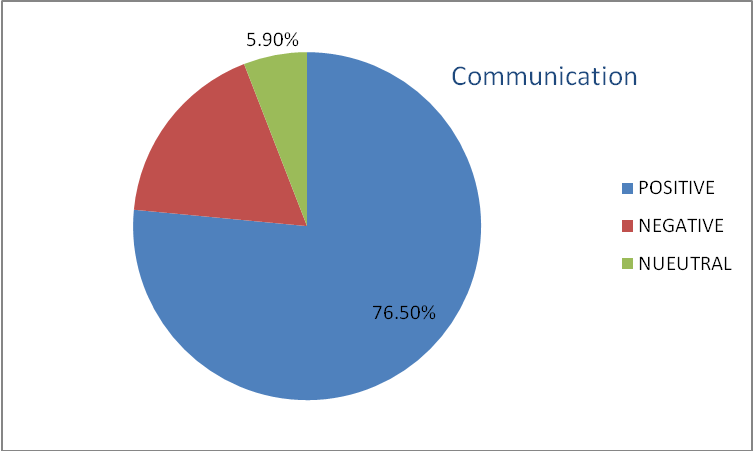
The total of those that were satisfied with their job represented 76.5% of the respondent of those interviewed. 41.1% and 35.3% strongly agreed and agreed respectively that there was effective communications and they were free to contribute their ideas in their work place.
Leadership also features as one aspect that greatly affects employees’ morale. 52.9% recorded that their leadership plans motivates them, while 29.4% were that the management plans were tailed to motivate the management.
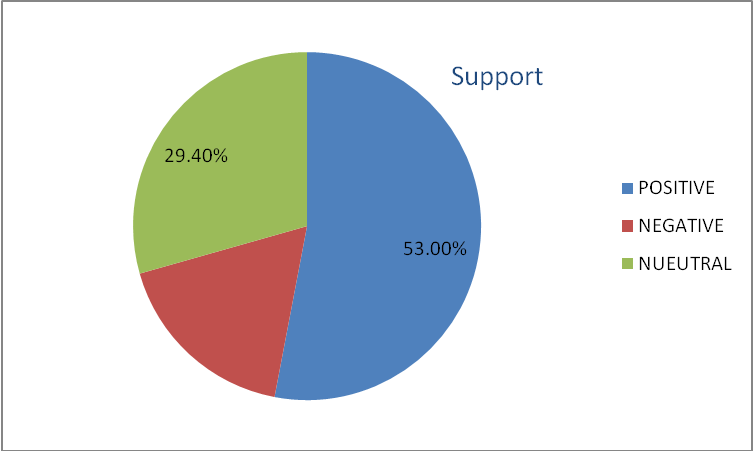
17.6% and 41.2% of the respondent strongly agreed that they receive adequate support from the management. 23.5% of the total respondent complained that their unit did not offer sufficient educational support and in services that are enjoyable and engaging.
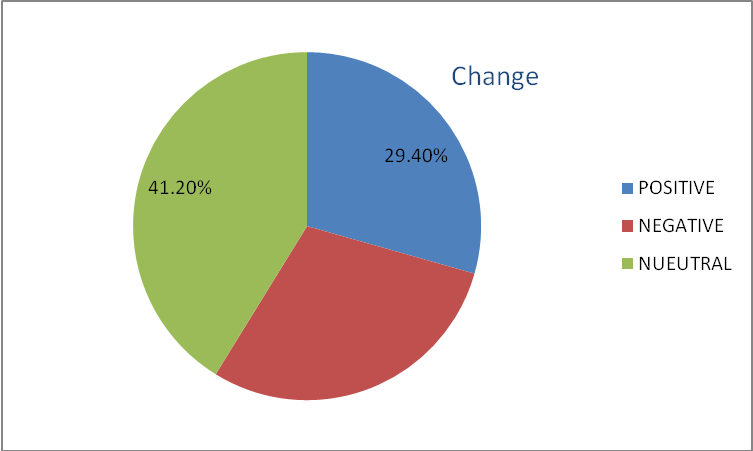
Safety of the workers also featured as an important factor that affect employees’ morale. 41.2% strongly agreed and 35.3% agreed about its importance in ensuring high employees morale. 17.6% and 41.2 agreed that autonomy was encouraged in their work. This represented 58.8% of the total respondent, with 23.5% disagreeing about the support of autonomy in their organization. 29.4% of the total respondent are the one who were ready to welcome change in their organizations since it meant improvement to them, but 35.3% were not happy with change in their organization.
Discussion
According to Fredrick Herzburg, Job dissatisfaction results when the hygiene factors are not addressed by the management. This occurs when the employees are not well paid; the working conditions are not conducive. Similarly, job dissatisfaction also results when the motivators are not met in a workplace.
In this research, though the issue about job dissatisfaction featured as one of the reason of low morale of the nurses who work in the remote and rural area of Canada, it only represented the minority of the group since 76.5% reported that they were satisfied with their job. The high job satisfaction of the nurses can be as a result of the good communication that exists among them and the management since from the study 75.4% of the respondents were happy with the communication at their workplace. Good communication motivates the workers to work hard when they realize that the management considers their opinions as important. This realization raises their morale greatly which makes them being satisfied with their job.
Appropriate support from the management is also considered to affect the employees’ morale greatly. The research showed that 53.00% of the responded reported receiving appropriate education program in their work. Though, the response is above the average it means that the managements need to improve on their training programs so that to reflect the needs and interests of their workforce so that the employees can feel adequate supported and thus increase their morale at work. Thus the nurses working in the remote and rural areas of Canade lack sufficient support from the management. This is one of the reasons why they reflect low morale in their work.
Autonomy also recorded 58.8% of the responded. This also calls for action from the management that is responsible for the nurses who work in the remote areas of Canada. The management should encourage autonomy in their work place to uplift of those nurses who morale is down in their workplace.
Change is always a very controversial issue to many people. The problem that makes employees have a negative perception on change in many organizations is because of how changes are implemented. Most leaders in management are not knowledgeable on strategic change implementation. They do not communicate about the impending change process to their workforce early enough so that the employees can be psychologically prepared for it. This is the reason why only 29.4% of the respondents were comfortable with a change in their place of work, while 35.3% did not entertain the idea.
The nurses who work in the remote and rural areas of Canada due to their nature of work are likely to experience a lot of changes in their workplace now and then. Thus, the management should ensure that they implement these changes strategically so that not to affect the morale of the nurses negatively.
Further research
The researcher advocates for further research to explain why the job satisfaction of the workers interviewed featured very high, despite many observations of the factors that affect employees’ morale being recorded as average and others much below the average.
Conclusion
Good leadership, autonomy, teamwork, support and strategic change management are factors that make the working environment healthy to work in. Thus, it is important for the leaders to ensure that they provide their employees with such an environment so that to boost their morale and ensure high performances.
Reference List
Cresswell, J. W., (2003). Research design: Qualitative, quantitative and mixed methods approaches. Thousand Oaks, CA: Sage Publications.
Durham, J. (2010) Improving Staff Morale in the Workplace. Web.
Hardy, B. (2009). Morale: definitions, dimensions and measurement. (Unpublished Doctoral dissertation). University of Cambridge, Trinity Hall. Web.
Hayes, B., Bonner, A. & Pryor, J. (2010). Factors contributing to nurse job satisfaction in the acute hospital setting: a review of recent literature. Journal of Nursing Management, 18, 804–814.
Jishi, H. (2009) Motivation and its Effect on Performance on Nurse in Aramco Health Centre. Open University, Malaysia. Web.
Leedy, P.D., & Ormrod, J.E. (2010). Practical research: Planning and design. Upper Saddle River, NJ: Pearson.
Montour, A., Baumann, A., Blythe, J., & Hunsberger, M. (2009).The changing nature of nursing work in rural and small community hospitals. Web.
Purdue University (2008). Committee on the use of human research subjects: The role of the principal investigator in human research. Web.