Introduction
Congestive heart failure (CHF) is a “progressive and debilitating disease” that is characterized by the congestion of body tissues (Nair & Peate, 2013, p. 237). Five percent of all medical admissions in hospitals are due to CHF. When an individual has this disease, his or her heart is not able to pump adequate blood for circulation throughout the body; hence, the heart is not able to meet the body’s needs. Congestive heart failure can either affect the right or the left part of the heart.
Pathophysiology
Various precedent factors lead to congestive heart failure. The factors include:
Hypertension, acute myocardial infarction due to loss of myocardial muscle, leading to poor contraction, anemia, incomplete emptying from the left ventricle due to poor contraction of the myocardium, and valvular heart disease (Medifocus, 2011, p. 21).
Precedent heart problems such as heart attack/myocardial infarction, infection, arrhythmias, and congenital heart disease cause heart failure (2014). Diseases such as iron toxicity, diabetes, hypertension, amyloidosis, sarcoidosis, hypothyroidism, iron deficiency, and emphysema predispose an individual to CHF, as well.
There are two classes of congestive heart failure that are differentiated by the causative factor. CHF can either be attributed to the weak heart muscle (systolic dysfunction) or increased stiffness of the heart muscle (diastolic dysfunction). As earlier mentioned, CHF can either affect the left or right side of the heart. The left side of the heart is the most common. The characteristic of left-sided failure is high-pressure levels that affect the pulmonary veins in the lungs, leading to the accumulation of fluid in the surrounding alveoli (Rubin & Reisner, 2014). The aftermath is dysfunction of the alveoli; thereby, limiting oxygen availability in the body.
In right-sided failure, the combined effect of increased pressure in the veins that pump blood from all the other parts of the body to the heart and the compensatory retention of water and sodium results in edema of the abdomen, liver, and legs (Acton, 2013). Nonetheless, both sides are affected because when one fails, it places a strain on the other one. Even though the heart heals after myocardial infarction/heart attack, the resulting scar does not contract as a normal heart tissue would. Thereby, the heart becomes progressively weaker, and there could be the formation of an aneurysm.
Epidemiology
CHF is most prevalent among individuals over the age of 60. According to Rubin and Reisner (2014), 15% of the 2 to 3 million diagnosed with CHF die every year. Diastolic heart failure accounts for 30% to 70% of patients who get heart failure. Men have a higher prevalence of CHF in comparison to women, but according to Medifocus (2011), this gap narrows with age. The disease has a maximum survival rate of five years. The estimated cost of the disease is $ 32.9 billion in the U.S., and this figure will increase over the years due to projections of elevated prevalence of CHF.
Symptoms
There are several symptoms of this disease. Individuals complain of shortness of breath (dyspnea), which is due to the accumulation of fluid in the heart. This fluid accumulation is known as pulmonary edema. There is another kind of accumulation of fluid in the peripheral tissues, abdomen, and liver. CHF results in reduced glomerular infiltration and high renin secretion. Increased renin secretion stimulates angiotensin that subsequently triggers the release of aldosterone.
The result of these combined events is sodium reabsorption and fluid retention (Rubin & Reisner, 2014). There is also a reduction in hepatic flow that impairs aldosterone catabolism causing more elevated aldosterone levels in the blood. In a bid to correct the situation (a compensatory mechanism), the distended atria attributed to increased blood volume stimulates the release of atrial natriuretic peptide that enables sodium excretion (Rubin & Reisner, 2014). It is after this compensatory mechanism fails that edema results. Initially, dyspnea will be noticed when a person has engaged in physical activity or is undergoing emotional stress.
However, as the disease progresses, dyspnea is recognizable even as a person rests. Dyspnea is worse when people lie down, and in such a situation, it is called orthopnea. The disease may cause paroxysmal nocturnal dyspnea (PND), where an individual is not able to sleep at night. However, it is important to note that there are different symptoms for the different classes of cardiac heart failure as indicated on the mind map in this paper.
Diagnosis
The first step in diagnosis is to evaluate the signs and symptoms an individual presents. Various examination procedures are useful as Daniels and Nicoll (2012) comprehensively explain. There are stress tests that determine the function of the heart when subjected to stress/exercise. There are also laboratory tests, for example, complete blood count. Imaging tests such as nuclear scan, an echocardiogram, an angiogram, or cardiac magnetic resonance imaging (MRI) determine ejection fraction. Ejection fraction is the “fraction of blood in the heart during diastole that gets ejected during systole” and should be at least 55% (Acton, 2013, p. 26).
Treatment
Other than pharmacological treatment, there are some behavioral therapy procedures that individuals could use. A person with orthopnea manages the symptom by sleeping propped up on a stack of pillows, or in a recliner. Diet therapy is effective in cases of mild CHF. In pharmacological treatment, diuretics are used to in reducing the volume of blood and preload to the heart; hence, reducing the heart’s workload. Pharmacological treatment is used to improve the quality of life, but it does not affect survival. The current pharmacological regimen entails diuretics, beta-blockers, angiotensin-converting enzyme inhibitors, inotropes, and vasodilators (Acton, 2013, 27).
Assist systems used are things like mechanical pumps, which take up some or all of the pumping function of the heart; thereby, reducing the load on the heart. Patients use mechanical pumps, meanwhile, as they wait for a heart from a suitable donor. Defibrillators are ideal in situations where there is a need to regulate heart rhythms, while a pacemaker is appropriate in situations when the heart rate is too slow (U. S. National Library of Medicine, 2014). Surgical heart procedures entail dynamic cardiomyoplasty, heart transplant, and Batista partial left ventriculectomy (Acton, 2013).
Heart transplant takes place alongside therapies, which, according to Acton (2013), suppress the immune system. Cardiomyoplasty is a procedure that involves wrapping the heart with skeletal muscle to aid in the synchronous contraction of both muscle and heart upon electrical stimulation. Ventriculectomy involves remodeling the left ventricle by the removal of a part of the muscular wall. The result is a reduced diameter of the dilated heart, subsequently reducing the heat load.
Factors
Poor lifestyle marked by high caloric and salt consumption predisposes an individual to diseases like diabetes and hypertension, both of which result in congestive heart failure. When congestive heart failure occurs, there is an accumulation of salt in the blood; hence, therapy entails a restriction on an individual’s salt intake. Control of blood volume is imperative in the treatment of CHF. Therefore, individuals are asked to restrict both their salt and fluid intake. Intake of western diets that are high in calories and salt is a major reason for the occurrence of cardiovascular diseases and metabolic diseases that subsequently lead to CHF. Therefore, other than fluid and salt intake, an individual is asked to restrict his or her caloric intake to avoid elevating the blood pressure attributed to excess weight.
In addition, there is a strong association between genetics, ethnicity, and the occurrence of CHF. In such a case, where an individual is at risk by default of birth, intervention for CHF begins right from infancy to prolong the onset of the disease. According to Medifocus (2011), African Americans are more likely to get heart failure in comparison to Caucasians. A healthy lifestyle is imperative in such a case to slow down the occurrence of this disease. Health workers initiate patient education in the form of health promotion and health campaigns as a way of advocating healthy lifestyle choices.
Conclusion
Congestive heart failure is a chronic disease that affects the quality of life. It exerts a huge economic burden on one’s family and the country at large. Knowing one’s health status is the ideal thing to do, as well as understanding the disease. This knowledge enables one to develop strategies of controlling the disease; thereby, improving quality of life.
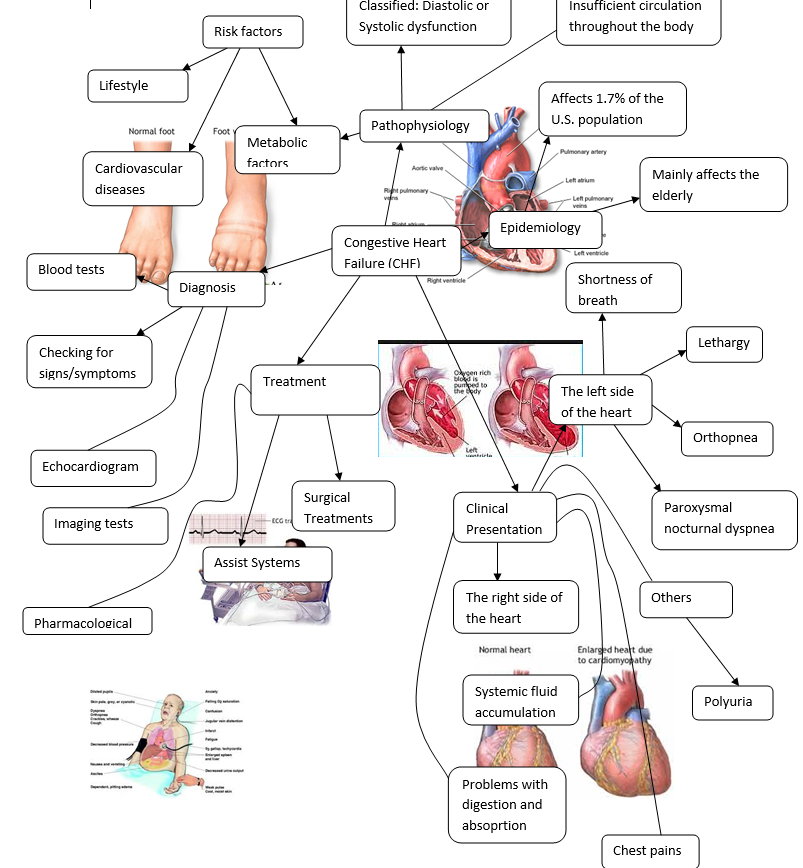
Mind Map-Congestive Heart failure
References
Acton, A. (2013). Congestive heart failure: New insights for the healthcare professional. Atlanta: Scholarly Editions.
Daniels, R., & Nicoll, L. (2012). Contemporary Medical-Surgical Nursing (2nd ed.). New York: Cengage Learning.
Medifocus. (2011). Medifocus Guidebook on Congestive Heart Failure. New York: Medifocus.
Nair, M., & Peate, I. (2013). Fundamentals of Applied Pathophysiology: An essential guide for nursing and healthcare students (2nd ed.). Iowa: John Wiley & Sons.
Rubin, E., & Reisner, H. (2014). Essentials of Rubin’s Pathology (6th ed.). Baltimore: Lippincott Williams & Wilkins.
U. S. National Library of Medicine. (2014). Heart Failure Overview. Web.