Real-Life Case Study
In February 2003, at Duke University Medical Center, Jessica Santillan who was 17 died after undergoing heart-lung transplantation because of a simple mistake. The circumstances of this case were particularly poignant. Her family and the wider community had gone to extraordinary lengths to make her operation possible. Jessica had been brought to the United States by her father, a truck driver from Guadalajara, Mexico to seek treatment for her condition.
She suffered from a severe congenital heart problem and was disabled to the extent that she fainted on any exertion. The only treatment for her condition was a heart-lung transplant. Her family begged in the streets to raise funds for Jessica’s procedure until a North Carolina businessman adopted her cause. Money was then raised by a grass-roots foundation by building houses with donated materials and selling them.
On the evening preceding the operation, there were considerable logistical difficulties in obtaining the organs. They were eventually implanted, but, after a short time, it became apparent that they were not functioning well. The transplant coordinator then called to inform the team that the transplanted organs were incompatible: Jessica’s blood type was O and the donor was A. Jessica spent two weeks in intensive care, critically ill. She underwent a second heart-lung transplant, but to no avail. On February 22 she was pronounced brain dead, and life-support was withdrawn.
During this period there was full disclosure of the facts by Duke Medical Center. The chief executive officer admitted publicly that an error had been made. A chronology of the events was posted on a website. Public apologies were made. Subsequently, a root cause analysis was undertaken, and changes were instituted into transplant procedures at Duke, to reduce the likelihood of recurrence of this type of tragic event. (Excerpt taken from Safety and Ethics in Healthcare: A Guide to Getting It Right by Runciman, Merry, and Walton).
Introduction
Since Jessica’s death, the health sector has experienced a historic transformation in areas such as organ transplantation, diagnostic approaches, generation of new drugs, modern surgery, pain relief, effective anesthesia as well as immunization. Today, the core changes facing the health sector include an upsurge of patient acuity, intricate disease processes, cost entertainment constraints, aging population and reduced length of stay in the hospital, technological advancement, and call for quality care by clients. Some of these changes have been linked to moral dilemmas and incumbent ethical standards that are adduced from the day-to-day responsibilities of doctors and nurses. This paper will analyze the excerpt from a book entitled “Safety and Ethics in Healthcare: A Guide to Getting it Right” by Runciman, Merry, and Walton. In particular, the paper will conduct a root cause analysis and develop a cause-and effect-diagram as well as an action plan for this Jessica case.
Critical issues Surrounding the Case
Good use of Healthcare
In this case, the healthcare resources were not utilized effectively. Even though the hospital had all the necessary equipment required in the process of transplantation, they failed to effectively use these resources. For instance, equipment for carrying out the blood test was not employed to verify whether the blood group of the donor matched with that of the recipient. Besides, Jessica’s parents raised a lot of money that could have been used by the hospital to carry out a successful transplant.
How things went wrong: Things went wrong when the surgeon failed to verify whether the donor’s blood group matched with that of Jessica’s. It was later revealed that Jessica’s blood was group O while that of the donor was group A.
Overlooked check of blood compatibility and person to be blamed
The health professionals failed to carry out compatibility tests before implanting the organs. This, in my opinion, is the ignorance of the basic procedure and neglect of duty. It is indeed regrettable that such experienced doctors ignored to carry out the obvious-conducting blood group test, which is a procedural requirement before implanting any organ to a patient. The hospital also failed to recognize the mishap early enough to save the situation. To this effect, the blame falls squarely on the surgeon and the entire hospital. Besides, the national organ-transplant system is also partly to blame as well as the United Network for Organ Sharing (UNOS).
The UNOS’ policies did not allow its officers to verify the blood type of the individual receiving the organ and this paved way for the mishap that could have been prevented had the UNOS policies permitted its officials to confirm the blood type of the patient before being selected to the donate the organs. The hospital could not have performed the second transplant since there are few organs available for transplant. Instead, the second organs could have been preserved for another patient whose chances of survival might have been considerably high.
Avoiding future errors
This error can be avoided in the future by strictly following the procedures required in transplantation. EKG (electrocardiogram), blood tests (including blood group test) as well as x-ray must be carried out on the patient before implanting the organs to him/her. The assessment before transplanting the organ to the recipient should also encompass social work and dietary evaluation. Moreover, a comprehensive dental examination should be carried out to minimize the infection from bacteria in the mouth. Efficacious therapies ought to be carried out to the right recipients for the correct indications and at the right time.
The relationship between effectiveness and timing of an intervention is referred to as timeliness. Concerning this case, organ transplantation should be carried out at the right time if good results are to be expected. Safety issues should be taken into consideration. Risks may be minimized by the surgeon responsibly carrying out the transplant operation making the right plans and not adhering to the laid down plan as expected. Risks can be minimized by putting in place excellent systems, practices, and designs.
Hospital’s Response
The hospital response was not appropriate. It failed to recognize the mishap early enough to save the situation. However, after the death of Jessica, the hospital responded well by disclosing all the facts surrounding the case. It also carried out a root cause analysis in an attempt to find out where things went wrong as well as to develop appropriate procedures to be followed during organ transplantation. Nevertheless, some claim that the hospital officials tried to cover up the case by hiding some basic facts from the members of the public.
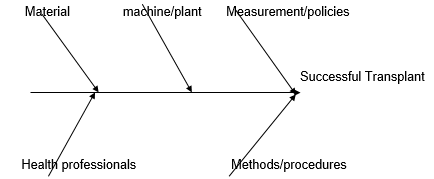
As the above diagrams demonstrate health professionals must be equipped with materials, machines/systems, measurement/policies as well as methods of procedures to carry out a successful transplant.
Action Plan
To avoid errors associated with organ transplants, initiating an action plan is critical. Action from this entails the following:
- Having in place appropriate systems/machine
- Scrutinizing health status and blood group of the Patient
- Scrutinizing the health status and blood group of the donor
- Following the right procedures during transplant
- Upholding ethical issues in the course of organ transplant
- Ensuring the safety of the patient
Conclusion
Conclusively, it is evident in the case that the surgeon, the hospital as well as system errors played an integral role in Jessica’s death. Her death raises serious ethical and safety issues associated with organ transplants. This paper recommends that efficacious therapies be carried out to the right individuals for the correct indications and at the right time. Organ transplantation should be carried out at the right time if good results are to be expected. Procedures involved in the transplantation of organs should be followed strictly. EKG (electrocardiogram), blood tests (including blood group test) as well as x-ray must be carried out on the patient before implanting the organs to him/her.
Many scholars agree that, with the increasing intricacy of modern healthcare, health professional desperately require advanced training. There is therefore the need to re-assess doctors’ curricula in light of its structure while at the same time emphasizing intellectual skills and mastery of facts versus basic principles. In other words, when appraising curriculum in terms of its structure, emphasis needs to be placed on the quality of the content, how the contents are organized and how students will be able to process and evaluate the information.