Process map
The paper will attempt to explain the issues that are faced by Health Management Organization (HMO) pharmacy and come up with possible solutions to the problems. In order to identify the problems at a pharmacy, it is important to first come up with the process map of the prescription filing process (Snee & Hoerl, 2005). The process map is presented below.
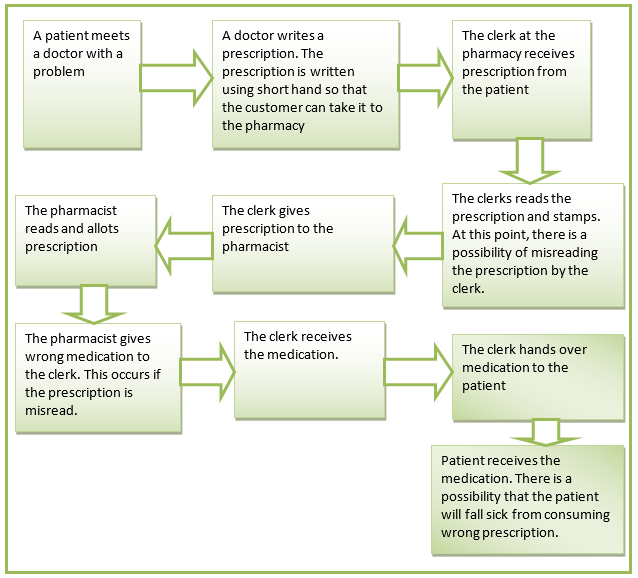
The map above is categorized into four parts, that is, ordering, transliterating, allotting and administering. In each of the four stages, there are potential areas for errors to occur. A closer review of the entire process shows that the most profound errors are incorrect drug, dose, patient, time, route, labelling, and drug interaction (Snee & Hoerl, 2005). In summary, it can be noted that the entire process lacks quality control checks that ensures that patients receive the correct medication.
SIPOC Model
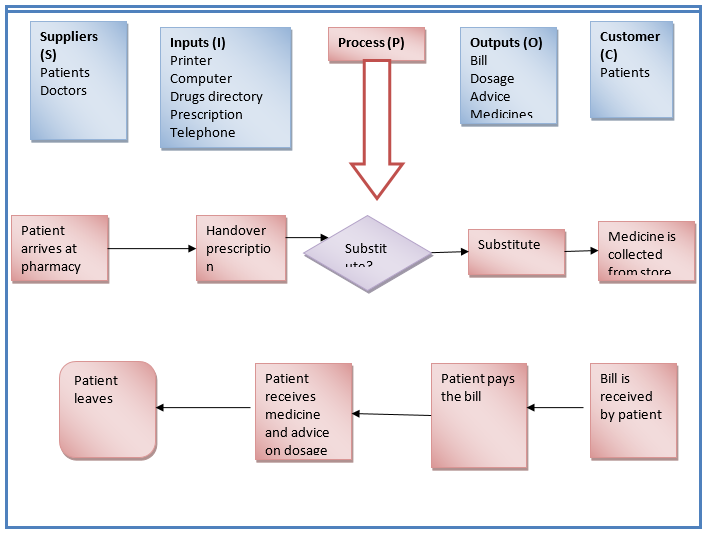
At this point, the SIPOC model will be used to analyze the HMO’s pharmacy business process. This model will assist in finding all important elements of the prescription filling process. SIPOC is an abbreviation for suppliers, input, process, output, and customer (Britz et al., 2000). The SIPOC model is presented below.
Root causes of problems
The first main cause is unreadable handwriting. This arises when the handwriting of the doctor cannot be understood clearly by the pharmacy clerk. The second cause is the lack of efficient and effective quality control checks. It can be observed that the process lacks a third party who reviews the prescriptions against the medication before being issued to the patients (James et al., 2009). Therefore, errors committed by one person cannot be noticed on time. The third root cause is interruptions.
This can be attributed to the fact that the clerk handles many patients and can make mistakes. Interruptions are also caused by few clerks handling numerous patients. This is likely to cause fatigue at work and increase chances of errors. Another cause is customer related problems. This arises from customers with numerous prescriptions, noisy customers, and customers in a rush. The final cause that can be identified in the process are traps. These are medications that sound or look like the prescribed medicines (Snee & Hoerl, 2005).
Special or common causes
A review of the root causes shows that they are common causes. They are not specific to the HMO’s pharmacy. They are common across various hospitals. For instance, a study conducted in the UK in 2007 showed that most hospitals experienced these problems (Anecleto, Perini, Rosa & Cesar, 2007).
Tools
The first tool that can be used to evaluate the cause of errors is carrying out root cause analysis. The analysis is important because it gives information on the reality of the causes of the errors. It also suggests possible ways of improving the process. The second tool is carrying out a survey. A survey is aimed at measuring the opinions and perceptions of the pharmacists. This tool is effective in establishing self-reported errors. Therefore, a combination of these two tools can be help in establishing errors in the HMO’s pharmacy business process (Snee & Hoerl, 2005).
Solution
The HMO’s pharmacy should introduce an automated pharmacy carousel system. Other items that can work together with the carousel system are printers, bar-code scanners, and a bar-coded medication bins. Also, it should have software that allows the carousel system to interact with the HMO’s system. Studies have shown that this system has significantly reduced errors in the business process of a process (Peck et al., 2006).
Strategy to measure the aforementioned solution
The solution above can be measured by calculating the rate of incorrectly filled prescriptions (error rate). This should be calculated before the system is implemented. After implementation of the system, the error rate should be calculated at an interval of one week. This rate should be monitored to ascertain whether there is a reduction in error rate or not. If there is a significant reduction of the error rate, then it implies that the system is effective (Cheung, Bouvy & Smet, 2009).
References
Anecleto, T. A., Perini, E., Rosa, M. B., & Cesar, C. C. (2007). Drug-dispensing errors in the hospital pharmacy. Clinics (Sao Paulo), 62(3), 243 – 250.
Britz, G.C., Emerling, D.W., Hare, L.B., Hoerl, R.W., Janis, S. J., & Shade, J.E. (2000). Improving performance through statistical thinking, Milwaukee, WI. Quality Press.
Cheung, K., Bouvy, M., & Smet, P. (2009). Medication errors: the importance of safe dispensing. British Journal of Clinical Pharmacology, 67(6), 676-680.
James, K. L., Barlow, D., McArtney, R., Hiom, S., Roberts, D., & Whittlesea, C. (2009). Incidence, type, and causes of dispensing errors: a review of the literature. International Journal of Pharmacy Practice, 17(1), 9-30.
Peck, R., Casella, G., Cobb, G., Hoerl, R., Nolan, D, Starbuck, R., & Stern, H. (2006). Statistics: A Guide to the unknown, Pacific Grove, CA: Duxbury Press.
Snee, R.D., & Hoerl, R.W. (2005). Six sigma beyond the factory floor; deployment strategies for financial services, health care, and the rest of the real economy, Upper Saddle River, NJ: Financial Times/Prentice Hall.