Description of the Community
The HIV/AIDS epidemic was first identified in Kenya in the early 1980s among commercial social worker population (US Census Bureau 2). Since then, the epidemic has spread to other parts of Kenya, including remote, marginalized areas. The Kenyan government had declared AIDS a national disaster in the year 1999. It is noteworthy that HIV/AIDS control and campaign programs have been relatively successful because of declines in prevalence rates have been noted across the country in both low and high-risk individuals, as well as in urban and remote parts of the country. In addition, population-targeted HIV testing has also shown the decline in the rates of new infections among the public (US Census Bureau 2).
Latest data provided by the Population Reference Bureau & UNAIDS (United Nations Program on HIV/AIDS) in 2012 have noted that 1.6 million Kenyans are living with HIV/AIDS. Kenya currently has 44 million people in which 820,000 women aged 15 years old and over have tested HIV/AIDS positive while nearly 200,000 children live with HIV/AIDS based on figures obtained in the year 2012. The HIV/AIDS prevalence rate in “the country is 6.1 percent while deaths related to HIV/AIDS were 57,000 in the year 2012” (Regents of the University of California 1).
Although marginal declines in the prevalence rate have been noted over the years, further studies have revealed that new, increased cases of infections have been identified among married couples who were initially not targeted in the health promotion campaigns. This, in turn, affects progresses made and could explain why the prevalence rate has remained the same (6%) since the year 2008 to 2012.
A summary of the mini-needs assessment conducted to determine a priority HIV/AIDS in Kenya
Studies have established that married couples and other people in more stable relationships have contributed to the highest number (more than 44%) of new HIV/AIDS infection in Kenya (Omanje, Bosire and Mwenda 73). Nevertheless, the UNAIDS report of 2010 had demonstrated that a decline in the rate of new HIV infections in the last decade was generally attributed to behavior changes, changes in social norms and enhanced knowledge on HIV/AIDS.
It is estimated that for every ten couple, a partner is most likely to be living with HIV/AIDS. In these marriages and relationships, some couples are not infected. Nevertheless, knowledge of HIV/AIDS among couples in relationships has been a significant source of concern. In addition, most of these couples have multiple sexual partners in marriage. While some couples are aware of their partners HIV status, “not all couples have this knowledge” (Omanje et al. 73). Moreover, a consistent use of condom is not common among married couples whose status remain unknown to their partners. Thus, most HIV transmission cases among married couples and those in stable, long-term relationships have resulted from ignorance of partner’s or self HIV/AIDS status (Omanje et al. 73).
Discordant, married or cohabitating couples remain at significantly higher risk for new HIV infections in the country. Moreover, couples who are in “acute phase of new infection are also critical source of risk for subsequent spread of the virus to their partners within or outside marriage” (Omanje et al. 73).
Therefore, without appropriate interventions, a large percentage of HIV infected individuals will infect their partners with HIV.
Until recently, the current prevention efforts have largely failed to account for couples (married, discordant or coexisting). Rather, most prevention strategies and campaigns have focused on casual relationships and youth. Thus, lack of knowledge has been a factor contributing to new HIV infections among couples in stable, long-term relationships. In this case, one can observe that lack of knowledge also implies a lack of awareness about risks of contracting the virus in such relationships. In addition, failure to use condom or low usages could be responsible for the widespread HIV/AIDS and other sexually transmitted diseases among population at risk.
A description of the primary socio-ecological factors related to HIV/AIDs in Kenya
Several major socio-ecological factors have been attributed to HIV/AIDS in Kenya. First, individual factors such as multiple sexual partners are responsible for several cases of new infections. These factors are influenced by community practices, beliefs and policies among others (University of Ottawa and Ontario Ministry of Health 1). Second, societal factors, including systemic discrimination and stigma affect the spread of the disease. People living with HIV/AIDS may fail to pursue interventions because of stigma. Third, socioeconomic and political factors show that HIV/AIDS is now common among marginalized, poor sections of Kenya.
Inequalities and gender influence risks of contracting HIV/AIDS. Fourth, cultural practices in Kenya could also be responsible for the spread of HIV. Practices such as wife inheritance and attributing HIV/AIDS to curse or witchcraft have affected any intervention efforts in such communities. Fifth, gender factors also influence the spread of HIV. In Kenya, for instance, it has been noted that women are more vulnerable to infections relative to men. In addition, coercive sexual practices and violence against women have exposed many women to HIV/AIDS. Sixth, generally, Kenya lacks robust healthcare infrastructures to cater for many people living with HIV/AIDS or implementing any effective health promotion programs. HIV/AIDS can only be controlled when healthcare infrastructures are working effectively.
Finally, government policies also influence HIV/AIDS outcomes. For instance, countries that have recorded success in fighting HIV/AIDS have favorable political environments and well-formulated policies. Policies should ensure that all stakeholders, including patients, political leaders, religious leaders, not-for-profit organizations and civil societies take active role in the fight against HIV/AIDS.
Types of resources and community stakeholders
Resources required for the target population, specifically married and cohabitating couples. They should aim to provide information on risks associated with HIV/AIDS in marriage or long-term relationships. Mass and local media should be used to offer consistent messages about HIV/AIDS and are the best channels for most Kenyans in rural areas.
Posters, leaflets, public announcements, printed articles and messages on radio and televisions have proved to be effective in Kenya. In addition, interpersonal communication conducted by leaders, physicians and other individuals of authority should reinforce the message.
All messages must be accurate, fact based, easy to comprehend and consistent among the target population.
HIV/AIDS programs in Kenya involve a wide range of diverse stakeholders, including people living with HIV/AIDS, policymakers, cultural leaders, religious leaders, civil societies, funders, regulatory agencies, care providers and international partners. In Kenya, only prominent stakeholders such as Ministry of Health, Kenya; National AIDS Control Council, Kenya; National AIDS/STD Control Program, Kenya; not-for-profit making organizations; and international organizations are recognized as useful. Thus, other stakeholders largely remain unaccounted for during stakeholder identification.
These stakeholders should participate in all processes involving HIV/AIDS intervention programs, including program implementation and outcomes. This approach normally enhances the relationship among stakeholders, evaluates their levels of engagement and focuses on HIV/AIDS concerns in a community.
A description of the stakeholder collaboration strategy and its appropriateness
A stakeholder collaboration strategy for the health promotion should be shared ownership for community health. Generally, as identified above, there are diverse stakeholders with different expectations from health promotion campaigns. It should be asserted that public health should be a priority for every member of the community, and not just healthcare providers or governments. A consultation process would bring together all representatives of all stakeholders in HIV/AIDS issues. It is expected that stakeholders would have divergent views but would share common concerns about HIV/AIDS infection in Kenya (Desclaux, Kouanda and Obermeyer S79).
Through consultation processes rooted in shared ownership for community health, all stakeholders would ensure that they create population health capacity over time. For instance, experts would provide knowledge for best practices on HIV/AIDS control and management. The process will ensure that stakeholders with diverse views develop a shared agenda, evaluation metrics, structured procedures and jointly funded health promotional campaigns to achieve one goal of reducing rates of new infections (Barnett 1).
Stakeholders must be represented across all phases of the HIV/AIDS programs. However, it is observed that not all stakeholders can play similar roles in the process. Therefore, experts in various fields may take multiple roles based on their professional skills in HIV/AIDS management in Kenya and other parts of the world. All members involved in the implementation of the campaign must address any issues that may hinder progress through effective consultation and collaboration processes.
Program goal and objective
Health promotion goal is to use comprehensive strategies to create awareness about new increasing rates of HIV infections among married, cohabitating couples and other people in long-term sexual relationships in Kenya. Thus, the promotion will engage married, cohabitating and discordant couples and the public across various continua of stages to ensure acquisition of knowledge and behavior change about HIV/AIDS spread among identified population at risk. This would strive at reducing the rates of new infections among sexual partners. It would also be imperative to collaborate with various stakeholders, including local, national and international agencies to identify and obtain external resources that could assist in HIV/AIDS health promotion campaigns.
The objective of the promotion on HIV/AIDS is to inform, educate and empower married, cohabitating and discordant couples and the public about new cases of infection among the target population. Thus, it is expected that by the end of the health promotion, at least 80 percent of the couples will have acquired knowledge on HIV/AIDS transmission among couples and demonstrate behavior change through changes in sexual behavior practices, use of condom and knowing partners’ HIV status among others. The target population may be contacted within three months to determine outcomes of the health promotion.
The theory used to guide development of the intervention
The Theory of Planned Behavior (TPB) has been effective for interventions (Foy et al. 207) because of the following reasons. TPB predicts behaviors with regard to factors considered for change such as belief systems, sexual behavior practices and potential external difficulties. TPB has been evaluated and found to be effective in various settings, and it recognizes that violations may occur because people to do not have absolute control over their actions (Foy et al. 207).Based on TPB, attitudes toward behavior is imperative, and a person’s view could be a subjective norm while perceived social pressure or views of others and alleged behavioral factors that include belief systems and self-efficacy (confidence in performing and achieving a given goal) and a wide range of environmental factors have profound effects on promoting or inhibiting performance. The theory also focuses on attitudes that show perceived outcomes and emotional attitudes. That is, TPB considers whether couples will benefit, be harmed after disclosing their status or healthcare professionals would feel discomfort while evaluating the disclosed behaviors. Thus, the theory will make it possible to predict changes related to sexual practices and acquisition of knowledge about HIV infections in marriage and long-term sexual relationships.
An appropriate intervention strategy that targets one of the socio-ecological factors associated with HIV/AIDS condition and target population
Behavioral intervention would be adopted in health promotion campaigns to change behaviors and sexual practices of married and cohabitating couples. It is imperative to recognize that most of these couples are now more informed about HIV/AIDS with the exception of few couples in marginalized, remote areas of the country. Education and behavioral skills to reduce exposure risk for infection and a focus on individual factors that hinder change would be appropriate intervention for Kenyan married couples.
Behavioral interventions accompanied by counseling and testing would be effective for many married couples who are at high risks of contracting HIV.
Specific Program Activity
Behavioral change will focus on couples HIV counseling and testing so that couples can know HIV status of their partners and change their sexual practices. Couples HIV counseling and testing would be effective because studies have shown that knowledge of HIV/AIDS alone does not necessarily lead to behavior change (Kanekar 10).
Couples HIV counseling and testing activity in this population at risk will aim at enhancing benefits of engaging in safe sex among couples. They must however undergo counseling and testing to change poor behaviors and reinforce their knowledge. Health promotion must ensure that counselors understand the relevance of interpersonal skills when engaging participants. In addition, they must demonstrate other practices such as constant use of male condoms during sexual intercourse. Counselors should also stress the risk of pleasure seeking by engaging in sexual intercourse with multiple partners outside marriage or stable relationships.
Counseling and testing for couples should also address individual factors related to unsafe sex such as low knowledge or poor perception of risks, abuse and inequalities in marriages and relationships.
It is believed that couple counseling will enhance risk perception through social interactions in which couples are encouraged to engage in meaningful conversation related to HIV/AIDS risks. This is most likely to lead to behavior change by ensuring regular and correct use of condoms and remaining faithful to only one partner.
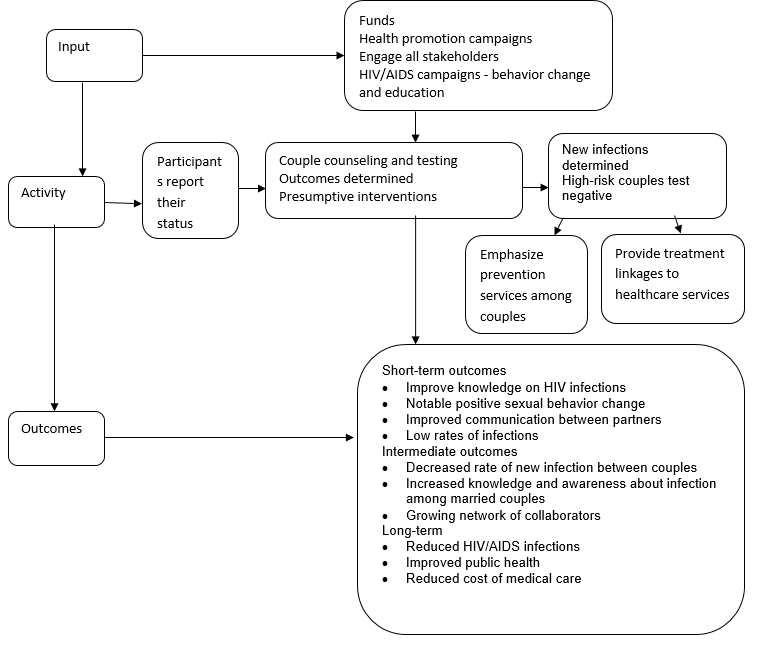
A Logic Model for the Health Promotion Program for Couples
Works Cited
Barnett, Kevin. Best Practices for Community Health Needs Assessment and Implementation Strategy Development: A Review of Scientific Methods, Current Practices, and Future Potential. 2012. Web.
Desclaux, Alice, Seni Kouanda and Carla Makhlouf Obermeyer. “Stakeholders’ participation in operational research on HIV care: insights from Burkina Faso.” AIDS 24 (2010): S79–S85. Print.
Foy, Robbie, Jillian Francis J, Marie Johnston, Martin Eccles, Jan Lecouturier, Claire Bamford and Jeremy Grimshaw. “The development of a theory-based intervention to promote appropriate disclosure of a diagnosis of dementia.” BMC Health Services Research 7 (2007): 207. Print.
Kanekar, Amar Shireesh. “HIV/AIDS Counseling Skills and Strategies: Can Testing and Counseling Curb the Epidemic?” International Journal of Preventive Medicine 2.1 (2011): 10–14. Print.
Omanje, Thadeus S, Sheillah Bosire and Samwel Mwenda. “Knowledge and Perceptions of HIV/AIDS among Married Couples in Kenya.” Public Health Research 5.3 (2015): 73-78. Print.
Regents of the University of California. HIV/AIDS in Kenya. 2014. Web.
University of Ottawa and Ontario Ministry of Health. Socio-ecological assessment: HIV/AIDS in Kenya project. 2009. Web.
US Census Bureau. HIV/AIDS Profile: Kenya. 2008. Web.