Introduction
Healthcare Compliance Department is especially vital in building a reputable healthcare facility. Compliance with government and federal acts makes the facility enhance efficiency and therefore protect the privacy of patients. The healthcare sector is one of the highly regulated sectors, and it is highly expected to be very compliant with all the regulations put into controlling the services offered for the well-being of the patients. The compliance department is crucial in any health organization to help create and implement the laws that should be followed.
Policies and Procedures
The policies and procedures are the layout laws and regulations that the health community has to follow to ensure the security of the patients and the workers. The standards in the workplace are the code of conduct, recruitment policy, health safety, and anti-harassment policy. The compliance department should make its procedures that go in line with the department of justice, Department of Health and Human Services (DHHS); this department was created to protect people’s health and promote essential services and provide quality care (The Institute of Internal Auditors, 2021). There are also Federal and state programs that consist of health research, civil rights, healthcare security, disaster preparedness, and civil rights. The health rights are covered in the Health Insurance Portability and Accountancy Act (HIPAA), which protects patients’ privacy. Data protection under Health Resources and Service Administration ensures data is well stored at the warehouses and easily traceable. The department of Health and Human Services (HHS) offers guidance on public education about health policies and pertinent healthcare information.
Purpose of Compliance Department
There are many ways the compliance department can be effective for the healthcare organization. First of all, these program provides the facility with framework regulations and laws to help lower risks associated with this industry. The compliance department ensures the work ethics are upheld and all the staff work according to the code of conduct. Moreover, it commits to compliance with policies both by the government and those formulated internally to help set a compliance culture. Such department in the medical organization helps to comply even when hiring staff to get the right staff that is adherence to the regulations required. Additionally, it standardizes ethical policies by coordinating with other relevant departments to enhance patient security.
Besides encouraging accountability in the facility and encouraging employees to report any kind of violations, it identifies risks and advises the management on how-to on the proceedings. Designating a Chief complaint officer monitors operation and report to the executive and management on the situation of compliance. Moreover, it concerns such aspects as developing and ensuring maintenance of the flow of information communication chart for the effectiveness of communication and reporting of violations.
Health Compliance Board Responsibility
The responsibility of the health compliance department is to adhere to programs designed to govern the health sector. These are developed in conjunction with health measures from law-making bodies like the CDC, Federal and State regulations, and other government laws to ensure compliance. Acts like the Healthcare Compliance Association (HCCA) allow practitioners to be compliant with their obligation to the law. This includes creating mechanisms to report unethical issues within the organization, approaching and identifying risks, and providing correction methods. Moreover, it involves ensuring coordination and coherence in the departments relevant to compliance like the Human Resource, Legal, Audit, and compliance department.
Governance Framework
The Patient Protection and Affordable Care Act (PPACA) mandates enrolment in federal programs that address fraud and violations of the vulnerable. Mostly the risks associated with the health care section are billing information, privacy and security, data documentation, and quality care maintenance. The framework is put in place to ensure smooth compliance with federal guidelines for a compliant health organization. The compliance department makes rules and regulations compliant with the state authorities. The health care management is given the mandate to ensure that the organization is well compliant to avoid falling into trouble with the authorities. There must be compliance in the legal department, management, executive, and to all ethical programs.
Compliance Strategy
The compliance department policy should target potential high-risk occurrences and complement it with suitable laws and regulations. They get this kind of information from previous internal and external audits, previous years’ assessments, reports of non-compliance cases files, and also need to study current trends to develop a better strategy. When the compliance department conducts a good data analysis, the policies are likely to be more effective. For better results, the compliance team should ensure effective coordination of the internal auditing systems and ensure effective monitoring of programs. Health inspections from external agencies can help the compliance department in making an effective strategy by identification of the weakness in the facility and emphasizing them in their policymaking process.
Recommendations
The compliance department should pursue the following for the success of the compliance policies and programs they should create. Hence, Compliance Management System (CRM) is required to implement and manage compliance within the facility. Another recommendation is to create an enabling environment for health workers and other stakeholders to enjoy their work obligations without feeling too much pressure. Assessing the level of risks in the organizational setup to create effective policies under the facility’s current needs is of particular importance. In addition, the compliance department should create policies and programs that give importance to the elements of the federal and state acts to reduce risk management.
Compliance Analysis
The task force of the compliance team is supposed to carry out investigations and analyses of the current happening in the organization. The team looks for ways of remodeling the companies’ laid rules by evaluating the risks the company is exposed to and recreating the programs to ensure the organization justly follows the compliance concept. It must be noted that the compliance universe has some risks that the organization must be aware of (Tab. 1). The compliance concept helps the organization reduce violations and risks of lawsuits and legal if well analyzed and evaluated.
Table 1. Compliance Universe and Its Risks
Functions of a Compliance Officer
The compliance officer is responsible for establishing a compliance program, monitoring, and ensuring total adherence to the program. Moreover, this specialist gives reports to the relevant management authorities on the compliance state of the organization and gives measures for betterment. Another task of compliance officers is to ensure coordination and training of staff on the importance of compliance and the actual laws. In addition, they coordinate with HR to ensure all contracted employees are adhering to the laws of compliance and strictly investigate violations and ensure effective discipline. The last function is to periodically review the compliance laws and revise the law to ensure they match the organization’s needs.
Skills and Qualifications
To become compliance officers, people must obtain a bachelor’s degree in law. In addition, compliance certificates like the Certified in Healthcare Compliance (CHC) and Certified in Healthcare Privacy Compliance (CHPC) are required, and candidates have to have a good compliance background. Moreover, they must have strong decision-making and coordination skills, be good strategic planners, and have a deep understanding of the organization’s culture (The Institute of Internal Auditors, 2021). Another requirement is that people must be well conversant with technology and the advancements for effective detection of any violations.
Internal Teams
The internal auditing department deals with the evaluation of internal activities to see the effectiveness of processes. Compliance and auditing have some similarities that make them coordinate, such as they both must investigate cases of violations of the compliance policies. Additionally, they access the database of the whole organization, and both advise the management on the implementation of policies and laws to achieve the organization’s strategy. Henceforth, they both report to the board of managers about the compliance situation in the organization.
Compliance and auditing have a role in ensuring discipline and adherence to the code of conduct. They investigate violations of the code of conduct, ensure related discipline is administered, and ensure recruitment is compliant with the regulations of the federal and state action. They all have the mandate to check the legal stability of the organization. These departments have to coordinate for better results and resolve issues related to legal. They also equally make recommendations to the management about the legal situation of the organization. It must be noted that technology is very vital in the security of data in the healthcare sector, but also it is highly targeted by fraudsters and cyber attackers, and this is why it has to work closely with the compliance department to ensure the information is stored securely under the set rules of HIPAA for the confidentiality of patient’s information.
Function of Compliance Department
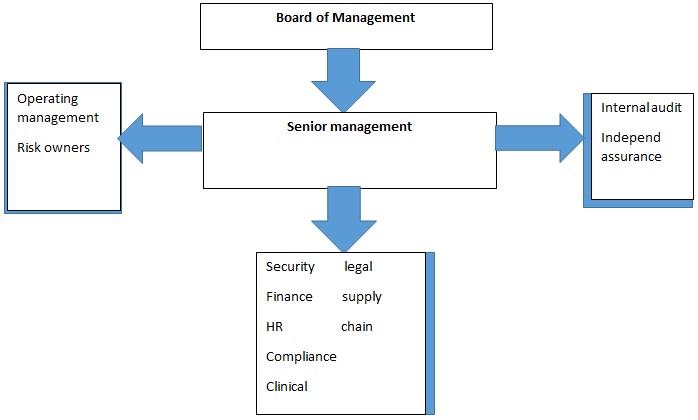
The compliance department constitutes an essential part of the healthcare establishment and has a complex structure (Fig. 1). The function of the compliance department is to ensure patient privacy and security acts are well adhered to. Therefore, it follows compliance with the government rules so that the facility does not fall into trouble with the government. The studied department helps the facility reduce the risks such as malpractice and violations of the code of conduct and makes sure health information is stored securely and complies with the set health standards. In addition, it enhances transparency in the organization by investigating any kind of violations and creating a platform that helps whistleblowers raise their concerns.
Another vital function of the compliance department is assisting the organization to enhance its reputation and reduction of lawsuits and legal problems. It is responsible for creating well-defined programs that can easily be understood for increased efficiency. Ensuring CMS is implemented in the facility and regularly reporting on the situation of the compliance to the management is also of particular importance. The compliance department is responsible for monitoring changes made to the legislation, adapting them, and ensuring quality control throughout the organization. Lastly, this organization segment is in charge of training on the code of conduct and the importance of transparency.
Coordination with Remote Locations
The compliance department should always try to get along with the board of managers as mutual relations will ensure a smooth flow of work. The compliance department requires the BOM to support its ideas and ensure communication across the organization. And also should have cohesion for the success of the implementation of compliance. Moreover, the department and HR managers should coordinate to ensure the effective implementation of the code of conduct and ethics. When speaking about information technology, the two departments make internal coordination to ensure adherence to the security and confidentiality policy of the patient’s information. Legal representatives of the company and the compliance department have to work together to prevent the organization from suffering third-party violations and enhancing privacy and compliance.
Training and Awareness
The compliance department must be able to train the employees in a health care facility about its policies and regulation for them to understand and be able to work complying with the laws. The complaint department takes a lot of emphasis on technology by training workers on the effective ways of ensuring data is stored securely. Employees are trained not to leave their work gadgets unlogged out to prevent information theft. They are also trained to avoid connecting their devices to the internet online to avoid cyber-attacks. They are also advised not to share their login details with anyone else to prevent breaches. According to HIPAA, every employee in the health sector has the right to refresher training at least annually. This is helpful to both protect the entity and the patients from unauthorized disclosure of health information. This training will help keep the facilitator fresh and highly compliant with the regulations required.
Importance of Training
Training is a part of the law, and The Health and Safety at Work Act requires all employees and employers to have practicing steps through training. It is needed to minimize risk management. Improving employees can increase efficiency in productivity and helps reduce the cost of fines and other sanctions that are caused by non-compliance. Moreover, it helps create a safe space at workplace hence increasing efficiency and making workers adapt to the culture of compliance.
Compliance Channels
The establishment of the compliance department enables the organization to adapt to new emerging ways in the technology sector. The departments need to have very comprehensive assessments of the technology used to evaluate the system’s compliance with the regulation put, such as data encryption to protect the channel of communication. These innovations, if well adopted can lead to enhanced services at the facility with all the risks like data protection and billing being up to the required standard.
Compliance Reporting
The compliance department is bound legally to ensure that the people who report non-compliance issues should be protected so that they are not subject to retribution. If the compliance or head of department breaches, the whistleblower can decide to report directly to the Office of Inspector General (OIG). Confidentiality is highly required for cases of fraud, abuse, or wasteful management. The reporter also has a right to report anonymously without revealing their identity; in this kind of reporting, the user does not enjoy the protection under the act of federal and state whistleblower laws. The compliance department requires all workers to have an obligation to report cases of non-compliance to enhance security. When the issue is about a system in the department, a person can report directly to the immediate superior. Employees are encouraged to report issues of non-compliance, like a violation of code of conduct, violation of health care standards, violation of pertinent policies and procedures put to regulate the practice.
Steps of Reporting
Firstly, the organization should stop engagements with people or activities they think violate compliance. Therefore, they must use the right channel to report and also keep in mind only the compliance officer has the mandate for your protection. Managers can report an issue using a hotline or go directly to the compliance officer and the office of OIG as a person responsible for the detection of fraud and abuse. The vital aspect of this process is the anonymity of the reports, and the compliance officer should offer warranty protection against retaliation. The reporter can use the hotline to speak directly to the compliance officer. This method allows questions and can help get more information regarding a case. Moreover, beneficial can be text messages or recorded messages. Email reporting also can be used even though it is discouraged as it might breach the sender’s privacy.
Monitoring and Evaluation
Annually the compliance team has to make a report of evaluation on the organization’s activities, mention the risk areas they observed, and give their reviews on the evaluation. The report is then approved by a committee appointed by the board. Monitoring involves activities like work inspection, assessments, incident tracking, and suggestions from employees.
Assessments
This measures the frequency of an issue or the proximity of the hazard. Assessments may include biological monitoring, reviewing health records, and medical examinations. This enables the compliance department to be aware of the compliance loopholes and advise promptly on the measures to be taken. It also helps the compliance department find aspects that need to be included in the compliance program for the betterment of the organization.
Incident Tracking
This is where the compliance team has to follow up on incidences of non-compliance to find out the frequency and severity of the situation. This helps to find proper measures to deal with the situation. The compliance team has to choose who is going to take part and if they are willing to give out information without pressure so that to come up with effective recommendations.
Suggestions
Employees can give their suggestions on issues and tell what they think is best suited for the organization. They can give suggestions through questionnaires, interviews, meetings, and so on. This helps the compliance department to come up with the best-suited policies that are acceptable to the employees too.
Independence of the Compliance Department
Under the policy of the three-line model, it states the first business line owns the risks of an organization that being the board and the owners, the obligation of ensuring compliance lies in their power and required to initiate rules and regulations for internal compliance. The second line includes the provision of oversight and compliance in the organization. The independence of compliance is essential even though the two lines of command oversight. The guidance act from the Foreign Corrupt Practices Act (FCPA) resource guide updates to “Evaluation of Cooperate Compliance Programs” that the function of compliance should be made independent and should not be influenced by any organ internally. This will allow the compliance department to be able to give advice to the first line and also be able to deal with their line of compliance and support each other.
Elements of Independence
Written framework for the compliance department that is approved by the board to give it power over its mandate independently. Appointment of Chief Compliance Officer (CCO), with the responsibility to report to the committee appointed by the board of the hospital for the department to achieve anonymity. Additionally, the compliance team should not mix work by doing other employees’ tasks for them to maintain their function. The board gives the compliance department authority to access all data from the organization to be able to carry out its mandate successfully.
Principles of Compliance
Compliance should be a formal function documented in the law to give it its independence and authority to take its mandate. The management should appoint an overseer on the duties of the compliance department that does not partake in any internal line of work. Therefore, the staff should be compliant with the policies framed by the compliance department to avoid contradiction and avoid taking activities that contradict the interest of compliance. The compliance department should have direct access to the highest rank, like the executive, for information or other materials. Moreover, it must ensure that liability checks should be taken when dealing with the third parties and patient privacy protection as provided in (HIPAA) implementation to keep their records secure. Principles of Compliance include the affordable insurance implementation and False Claims Act, making it illegal to fill in false information regarding funds from institutions like Medicaid or insurance companies. Furthermore, one of the principles is to regulate drug creation and supply by the Drug Enforcement Administration.
Responding to Audit Reports
The compliance department audits report is directly responding to the recommendations made by the audit team. It also identifies specific information that is not pertinent to its work frame and imposes corrective action. The organization should recommend the findings of the audit and advise the management on the practical measures they need to put in place. Therefore, it is responsible for forming the timeline for the creation and implementation of the recommendation.
Compliance Self-Assessment
There is a need to exercise the attribute of self-control and oversighting the departments’ elements to ensure that its performance is verifiable and that the members are also complying with the set rules of the code of conduct of the facility. The process of following audit verification and self-compliance duties can be expensive, and this might lead to a tussle between the compliance department and the financing bodies. Moreover, an excessive amount of pressure and expectations can make the department be negatively impacted. Gaps in the audits can lead to loopholes in the organization’s compliance, which would affect the reputation of the compliance department. Furthermore, the governing laws are ever-changing and are an added responsibility as many different responsibilities are to be carried on by them. Unreliable data got from the audits can be non-standard recommendations and inconsistency.
The emergence of many laws, especially in technology, makes it difficult for an organization to comply with them. This is because they stretch them to a limit they cannot, as it is costly to implement some of the trends emerging in the technology sector. Duplication of the compliance policies can lead to very diverse effects as it may cause the compliance department to have a hard time in management, which is a breach of compliance interests.
Best Practice Compliance Verification Steps
The compliance department should form solutions to self-assessment and the usual audits made in the department for use. These solutions are supposed to be made clear and well mentioned in languages understood by the team for learning and adoption of the system. The workers under the wing of compliance are to take compliance applicability assessments to see the effectiveness of adherence (Eastern Health Cluster, n.d.). The team could use questionnaires to speed up the tests. The assessment program should be done at the launching of the program for effectiveness and efficiencies as they start work.
Change of regulations can be used to manage risks when incidences happen or violations. If there is change at the workplace, reviewing programs to ensure applicability to the regulations is required. In case of high risks experienced at the facility and continued failure of mechanisms put for compliance, then the facility can decide to use second and third lines of command for monitoring. This is an example of self-assessment questions the department should use:
Table 2. Medicare Advantage and Drug Prescription Compliance Program Effectiveness Self-Assessment Questions.
Conclusion
The healthcare sector has very complex laws regarding the safety and privacy of patients. Therefore, the health facilities need to have information about compliance and regulations set by the relevant authorities. The compliance officers, together with other health care workers, are supposed to be aware and have an understanding of the compliance regulations for the maintenance of an effective compliance program. The operations put in place by the Federal and State should be sufficiently addressed.
The organizations should stop negligence towards compliance because the budget-related issues as it brings very satisfying solutions that help the organization to adhere to the compliance requirements hence avoiding falling into trouble with the relevant authorities. Avoidance of these non-compliances will lead to more efficiency, and this brings more investors to the health sector because they need the safety of their investments. The executive should ensure effective budget plans for the compliance department for effective coordination and auditing of the organization’s compliance status.
References
Eastern Health Cluster. (n.d.). Long-term strategic plan 2021-2025. Eastern Health Cluster.
The Institute of Internal Auditors. (2021). Internal audit and compliance: Clarity and collaboration for stronger governance. Global Perspectives and Insights.