Executive Summary
Business environment and the way business is carried out in the modern world are changing at faster rate. Globalization and other factors have been identified to be the key agents to these changes. These changes have not isolated the health care industry, where today, for efficiency and productive health care delivery, there is need of adopting the most efficient information systems.
Medical record processes in most health care organizations are still boggled by traditional manual systems, which remain inefficient and defective in many ways. Many medical errors have originated from old manual system, which has prevented appropriate health care administration procedure and process. As a result, it is established that adoption of electronic medical record (EMR) system is necessary in the modern world.
Organizations with ability to adopt the proposed collaborative EMR system possess the power to improve their overall health care delivery processes. Other related medical benefits are likely to be realized, and all these will improve the overall nature of health care in the country. However, for this to be achieved, there is need for top management to be involved, together with other key stakeholders.
In this manner, it is believed that collaborative effort and input of key stakeholders is necessary. Lastly, achieving objectives of collaborative EMR system requires a clear implementation plan, which gives overall strategies to be used to ensure goals and objectives of the new system are realized effectively.
Therefore, it is suggested that organizations, despite their size and nature, need to start thinking on the best way to initiate and develop appropriate EMR systems.
Health care Systems Analysis and Design
Information systems have become the artery in which modern organizations have the capability and power to navigate through dynamic business environments (Jeffrey and Lonnie, 2005).
In this sense, it has become clear that to be able to delivery appropriately to the designated clients and related stakeholders; many organizations are today involved in activities that aim to position the organization at a superior position using sophisticated information system tools.
This has seen the emergence and dominance of computers and related information system products in aiding an organization to improve and enhance its market performance and delivery strategies (Jeffrey and Lonnie, 2005). Health care sector constitutes one area where information systems have become an issue that can no longer be ignored or underrated.
The health care sector is regarded as one of the most information-intensive, and the need for technology in this sector has increased (Wager, Lee and Glaser, 2009). In carrying out an evaluation of health care providers in the country, one realizes that service delivered has been boggled by absence or inadequate information technology tools.
For instance, access and utilization of information in the hospital has been a big problem, whereby un-timely, incomplete, inaccurate, unreliable, and sometimes irrelevant information has been utilized to make health care decisions resulting into adverse effects for organization, client, society, and other stakeholders (Wager, Lee and Glaser, 2009).
It is with this understanding that modern-day health care providers are not leaving anything to chance; instead, they have become major and important participants in search for high quality and cost-effective service delivery systems in the form of appropriate, effective, and functional health care information systems.
Statement of Business Operation
The health care sector is perceived to be complex in many of its functions, a situation that has led to inappropriate adoption of health care information systems and related IT products and services. Smith (2007) observes that health care industry in the USA faces many challenges, and the situation affects the entire process of health care delivery.
At the same time, health care providers can no longer stick and depend on traditional methods and techniques of health care provision and delivery, but they need to embrace modern opportunities necessitated by growing urge for information technology and related processes. Information remains one of the fundamental tenets in proper health care delivery process, and there is need for various stakeholders to understand this.
The current situation in most hospitals is characterized by old approaches to information collection, integration, analysis, and then decision-making, which when evaluated and analyzed, has been overrun by modern-day events and more significant business environment dynamics. Therefore, what is needed is adoption of new approaches to health care system design, delivery, and operation in the new century (Smith, 2007).
At the same time, the new information system needs to be a product of numerous and multiple stakeholders’ effort, whose interest, concerns, and needs should be addressed through the process of designing, implementing, monitoring and evaluating the information system proposed.
In this way, the new information system approach should have ability to coordinate between and among different health care entities and those providing health care. Furthermore, the information system should be able to focus on delivery of care to the patient, while being efficient, cost-effective, and available to all that need care.
Analysis of the Organizations and Business Processes
Since the introduction of information technology some decades ago, profound changes have occurred that in one way or the other have transformed the way organizations conduct businesses, and deliver service to their clients. The health care industry, just like other organizations, has been a consumer of information technology products.
However, when comparison is made between information technology adoption and utilization in health care industry and other industries, it becomes clear that the rate and level of IT adoption in health care still lags behind other industries (Wager, Lee and Glaser, 2009). The health care industry is perceived to be complex, and numerous factors have been associated or linked to this nature of complexity.
The health care consumers are increasing, and this situation exerts pressure on the existing infrastructures, a situation that encourages inadequacy and inappropriateness. In addition, there are changes taking place in the health care industry contributed largely by forces of globalization affecting all types and forms of businesses.
As a result, there is increasing interdependence among organizations, while information sharing and dissemination are rampant, organization restructuring is taking place at all levels, and there is emphasis on cost-reduction of services with maintenance of high quality.
All these, together with others, combine to exert forceful pressure on health care industry to remain abreast with new developments in form of IT that will see designing, implementation, and delivery of health care more appropriate.
Smith (2007) observes that use of computers and information systems in health care sector is inevitable, and health care organization have a responsibility to play. The need for information systems in health care is partly contributed by the increasing health care needs and clients demand for better health care services, at faster rate and at reduced cost.
As a result, the current information systems in the sector are overburdened, pressured, or just ineffective to match new developments in the sector. As a result, there is need for almost total overhaul of critical elements that constitute current information systems (Smith, 2007).
In this way, the system’s specialists and analysts in the health care industry will have to design and propose more efficient and effective, coordinated information systems that make use of more sophisticated tools in delivering appropriate health care.
When analyzed and evaluated, effective and more efficient information systems possess the capacity to store extensive data of information that can be used in the health care provision process. Furthermore, data stored is likely to move rapidly from where it is stored to where it is needed.
Coordination is likely to be achieved in provision of health care services, and health care information systems are likely to deliver health care services in the most appropriate way, at reduced cost, and to the satisfaction of the client/patient (Smith, 2007).
Niles (2010) notes that modern-day management teams find it almost impossible to manage without improved and sophisticated computer systems. According to the author, the process of integrating information systems in the organization activities is leading to realization of many goals.
For instance, it has been established that computerization of departments and integration of various activities across departments has led to increase in efficiency and information sharing. Decision making has become possible and faster, redundancy has been eliminated, operation costs reduced, and quality of service delivery improved (Niles, 2010).
Therefore, adopting the most sophisticated information systems in health care sector is seen to be essential and necessary, especially in defining how data is collected and disseminated, how diagnostic procedures are performed, how medicine is delivered, how patients are treated, and primarily, how the health care system operates efficiently and effectively (Niles, 2010).
Given the complex nature of health care sector, coupled with business and operation dynamics present in the world today, it is prudent to suggest that development and utilization of any information systems that possess ability to meet strategic goals and objectives of the organization should be the priority of management teams in health care organizations.
New strategies have to be formulated within the perspectives of information technology, and this requires critical stakeholders in the sector to recognize and comprehend the more significant role of improved, efficient, and sophisticated information systems.
This assumption tends to challenge the existing order where there is excellent deficiency of information systems that perform, which has translated to poor service management and delivery in health care.
As an essential sector in the society that touches people’s lives, the health care industry needs to take a leading role in initiating proper and appropriate information systems. In other words, the significant health care structure in any organization should reflect the input of multiple stakeholders, which subsequently should result in the development and adoption of efficient information systems.
Despite this excellent concern for improved and efficient health care information systems, it has been established through numerous studies that there are certain barriers that exist and limit the appropriateness of organizations’ ability and capacity to develop and adopt sophisticated information systems-IS (Niles, 2010).
For instance, majority of information systems users (physicians, managers, administrators’, and government) find the cost of acquiring IS to be way above affordability power (Niles, 2010).
The cost is further accelerated when the IS has to be developed, tested, implemented, managed, monitored and evaluated. Nevertheless, the problem may be even more discouraging to smaller health care organizations with inadequate capital to install sophisticated IS.
Another barrier originates specifically when the process of developing and implementing IS is not inclusive, does not operate with clear strategy, and the overall implementation plan lacks consensus, education, and training (Niles, 2010). Accordingly, the act of inclusion in developing IS becomes the major tenet upon which success of the process is anchored.
Multiple stakeholders need to be consulted, interviewed, involved, and also motivated to give their best in terms of input for the IS development process. When it reaches a point where the organization acts in isolation, disregard critical opinions, and does not carry out effective organization and market research, then it becomes difficult for such an organization to have a concrete base and foundation for its IS development.
The issue of stakeholder inclusion should be evident from the moment the project is initiated and developed, which again should be accompanied with more education and training, information sharing, and popularizing IS awareness.
The last contributing barrier to adoption of health care information systems has to do with reluctance culture, uncertainty and fear, and absence of strategic planning and organization. The process of developing and integrating IS in an organization is enormous, tedious, and sometimes full of uncertainty.
For instance, Niles (2010) observes that moving from a hard copy system to an electronic system requires several components that may include physician order communication results retrieval, electronic control management, electronic physical order entry and prescribing, and clinical decision support system.
Also, related activities may include providing patients’ portals and automating personal health records and population health (Niles, 2010). All these aspects are likely to bring about changes in workforce and workflow, an aspect that is likely to lead to uncertainty, fear, and stress.
Therefore, organizations need to have pre-and post-training sessions for workforce to reduce the likelihood of resistance and reluctance instances.
Analysis of the Requirements for a Solution to the Business Operation
Health care provision today relies on accurate and effective data and information, which can only be generated through effective medical records procedures and processes. As a result, the quality of health care in modern world relies a lot on the type, nature, reliability, and accuracy of data and information collected by nurses and other medical professionals concerning the patient and related care management (Green and Bowie, 2010).
But even with this in mind, many health care provision processes have continuously relied and utilized traditional medical record data processes, which are inherently ingrained in paper record systems (Lighter, 2011). This conventional method has been found to be tiresome, long, and sometimes complicated, without forgetting that numerous errors have been identified on this traditional system (Lighter, 2011).
Therefore, as the modern-day business and health care environment continues to experience many changes in terms of operations, there is great need to develop new information and data collection systems. This process will enable accurate, faster, and reliable collection, dissemination, and utilization of health information and data more appropriately.
To this end, it has been observed that the best way to achieve or approach this issue is to develop information and data collection systems that possess capability to automatically record patients’ information from the time they enter a health care unit to the moment they leave.
Despite the great need for effective medical record systems in majority of USA health care centers, it has been established that the rate of developing and utilizing EMR still rated low in most of these health units (Lighter, 2011). In a survey carried out in 2008 involving 2,758 physicians, it was established that only 4% of health care hospitals and centers have integrated use of effective EMR in their operation (Lighter, 2011).
Moreover, it was found out that only 13% possess the basic EMR system, while 16% were found to have acquired EMR but due to various boggling factors, such systems were still inactive (Lighter, 2011).
On a lighter note, 26% of respondents expressed optimism that in the near future, the issue of EMR would be part of their organizational strategic planning and acquiring an effective EMR would be key priority in their organizations (Lighter, 2011).
Therefore, on overall, the EMR adoption in the health care industry in the country still faces challenges that need re-dress and practical actions. This is so, given the inevitability of operating in new world in absence of effective information systems such as EMR.
Decision-making process in the field of medicine, especially with regard to patient diagnosis, treatment, and recommendation, has been boggled with errors in the past. In attempt to minimize these errors, there have been growth of health care decision support systems in form of electronic medical record (EMR) information systems (Wager, Lee and Glaser, 2009).
EMR generally constitutes computer systems developed with the aim of improving health care decision-making about individual patients at the point in time that these decisions are generated (Berner, 2007).
When EMR functions together with computer-based physician order entry (CPOE), it has been evaluated and found to possess the ability of improving patient safety, reduce overall operating cost and at the same time, impact positively on the medical care process (Berner, 2007). EMR has become useful in the provision of recommendations for managing health care needs, specifically patients’ health needs.
In most cases, EMR is described as the computer system that enables clinical decision process by delivering guideline-based patient-specific recommendations about health status of individual patients (Wager, Lee and Glaser, 2009).
In order to operate or function to the desirability of the needs of critical stakeholders, EMR should possess essential characteristics that make it suitable. As a result, the symptoms manifested by EMR should be reflected in the overall functioning of the system.
Some notable critical functions of EMR that an effective EMR should have include ability to integrate health information and data into a sophisticated but productive system (Green and Bowie, 2010). Some of the data and health information to be integrated include medical and nursing diagnoses, medication list, allergies, demographics, clinical narratives, and laboratory test results (Wager, Lee and Glaser, 2009).
At the same time, EMR should reflect ability to support and function based on electronic communication and connectivity. In this way, the appropriate EMR should enable those directly and indirectly involved in patient care to communicate effectively with each other and the patient. This should also involve communication connectivity among key stakeholders via means such as e-mail, Web messaging, and more so, the telemedicine.
It is further observed that effective EMR should support results management process and this should involve all the health care results. Such results may include laboratory test results, radiology procedure results, pharmacological results and requirements, clinical documentation, and administrative modules, and all these should be integrated and made to function efficiently electronically.
The desire for effective EMR should further involve developing and enhancing order entry and support, which should incorporate use of computerized provider order entry, specifically in ordering medications.
Other critical notable features of EMR should include enhanced decision support system, whereby, the whole process is computerized in terms of clinical decision-support capabilities, which may consist of having reminders, alerts, and computer-assisted diagnosing (Wager, Lee and Glaser, 2009).
Related to this aspect should be an attempt to develop an EMR that supports holistic patient care and management in terms of everything from patient education materials to home monitoring to telehealth. Another key feature to put into consideration is the development of EMR, which supports administrative processes.
In this manner, an effective EMR should facilitate and simplify key health care processes such as scheduling, prior authorizations, and insurance verification. Also included in the sub-system of administrative EMR system are the decision-support tools that identify eligible patients for clinical trials or chronic disease management programs (Wager, Lee and Glaser, 2009).
More importantly, EMR system should have and effective clinical vocabularies system, interoperability capacity, and capability, EMR ontologies about the structure of the system, and EMR should be conducive to fitting with varying aspects of the system (Lighter, 2011).
Lastly, an effective EMR should possess the ability and capacity to enhance reporting and health management process. This should be so specifically in establishing standardized terminology and data formats for public and private sector reporting requirements (Wager, Lee and Glaser, 2009).
Discussion of Health Care Application Systems Solutions
In order to solve the issue of manual medical record process in health care institutions, there has been suggestion and recommendations to adopt different types of EMR. What needs to be known is that an EMR to be adopted by any organization depends on various factors and issues ranging from cost, sustainability, time, knowledge, and capacity of the organization.
Therefore, the process of developing and implementing an EMR should be holistic, inclusive, and strategic, incorporating organization’s goals, objectives, and financial power. In most cases, it has been noted that smaller organizations have mostly expressed reservations and rarely adopt sophisticated information systems.
The barriers associated with finances, expertise, capacity, and overall perception of EMR are outlined as some reasons that act to discourage organizations from adopting effective and efficient EMR (Murray and American Society of Critical Care Anesthesiologists, 2002).
On the other hand, large organizations adopt EMR in varying capacity, but research shows that even in large organizations, presence of sophisticated and effective EMR is still a problem and ineffectively carried out. Therefore, what is needed is that, despite their size and nature, organizations have to conduct an effective needs assessment study that identifies the most appropriate way to adopt or initiate an EMR system.
Two prominent EMR systems have been proposed in the past that some organizations have taken forward steps of implementing. The Clinicomp International Clinical Information System (CIS) constitutes one of the critical EMR systems that majority of health care organizations have adopted (Murray and American Society of Critical Care Anesthesiologists, 2002).
The EMR information system is designed ambulatory, outpatient, and inpatient use. The system has been designed and possesses capability to integrate current patient information and subsequently displays it at the point-of-care, at central stations, and from remote locations (Murray and American Society of Critical Care Anesthesiologists, 2002).
The system further supports patient care functions that include charting, managing order entry, and analyzing data as part of improved clinical decision support system. CIS exchanges information through the HL-7 language hence, it can effectively be integrated into an existing hospital information system.
The second information system is the Picis CareSuite, which has become prevalent in health care as an EMR system (Murray and American Society of Critical Care Anesthesiologists, 2002). Some key features of this EMR system are that it has an order entry system, decision support tool, and a reporting system.
Picis CareSuite is further enhanced by Chart+ program, which enables the system to collect automatically, manage, integrate, and store critical and essential patient information. The information integrated becomes necessary in evaluating patient’s condition, providing care, and further generating the medical-legal record of the patient.
In addition, the system has the capability to connect to a variety of medical devices, laboratory systems, and hospital information systems. The two systems have been unified by advantages of being faster, effective, time managing, and cost-effective.
Moreover, the systems have revolutionalized the way health care is administered and executed and the overall medical record management in hospitals has improved. On the negative side, most of these systems are expensive, sophisticated, and when not well managed, can destabilize patient’s medical administration process.
Recommended Solution and Implementation Issues
Designing an effective IS should follow particular steps and in each case, there should be successful integration of sub-system to the larger system.
As the health care continues to change as more dynamism take place in the industry, there is need to design and develop an effective EMR that addresses multiple health care needs in harmony with other systems of the organization. In other words, the proposed EMR system should be collaborative. Therefore, collaborative EMR system is what this study proposes.
Proposed Collaborative EMR System
The proposed collaborative EMR system can be seen to integrate different departments of the organization. Key departments include Finance, Engineering, administration, IT, Human resource, and many more. Designing the IS requires collaborative efforts of human resource in these departments. Cost, time, applicability, organization capacity, and clients’ needs should inform the development of the new EMR system.
The clinician puts the relevant data in the system, which, through the execution engine, is able to process, integrate, and disseminate information and data according to communication pattern installed in the system. Input information that the system absorbs includes radiology information, laboratory information, picture archiving information, pharmacology documentation, and clinical documentation.
Computerized system after that is able to carry out order entry that is built on system reminders, alerts, and computer-assisted technologies. The output data reflects products of enhanced EMR system in form of medical and nursing diagnosis, medical listing, allergies, demographics, clinical narratives, and laboratory test results.
Adoption and implementation of this collaborative EMR system are likely to results in some benefits, and health care, specifically patient care is going to improve.
These improvements will be evident in easy access to relevant patient data, shifting and stimulation of management change, and improvement in patient screening and diagnosis process. When well managed, collaborative EMR is likely to be cost-effective and at the same time, enhance efficiency in health care delivery process.
Collaborative EMR system
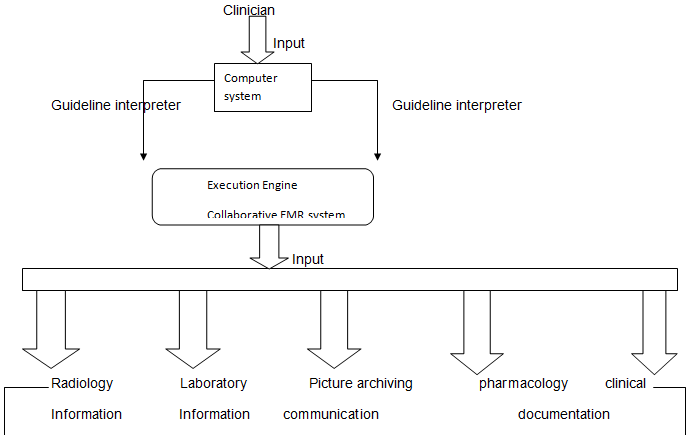
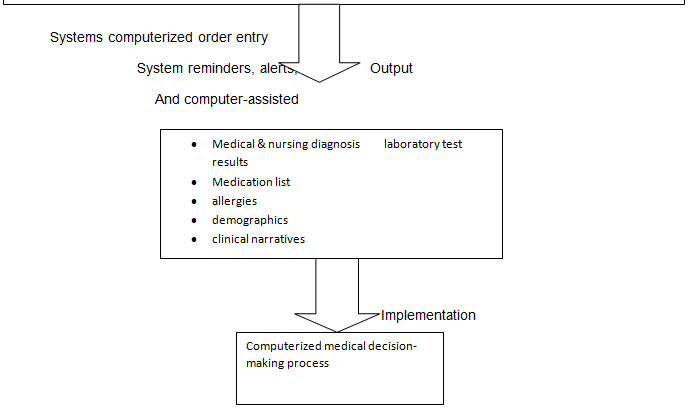
Source: Sources: Shankar, et al., n.d; Goldstein, 2008; Varshney, 2009; Jeffrey and Lonnie, 2005.
Implementation, Support and Maintenance
Successful establishment of an EMR requires a clear plan of the purposes of the EMR before it is developed and implemented. The plan should address and outline strategies to overcome issues such as education and training, engineering, installation, culture change, support, and maintenance.
The entire process of EMR should start with a vision, whereby, an outline that is clear and succinct on why the EMR is necessary is developed. After that, the vision is translated into concrete plan addressing the identified and specified needs and goals. Therefore, the organization management team should embark on process of identifying and forming the right project team to oversee the development of the new collaborative EMR.
The project team should have the right leadership structure, roles, and responsibilities of members identified. The project team should be at the center stage to carry out research assessment, and evaluation of the existing EMR systems, and subsequently, create recommendations and procedure for adopting the new system.
After all processes of identifying their various roles, the project team should now embark on process of gathering necessary and relevant information about the organization staff, patients, and practice habits which will be necessary and important in informing the type of EMR system to develop and implement (Scott, Rundall, Vogt and Hsu, 2007).
Cost-benefit analysis should be the core business of the team at this stage on various EMR systems and their suitability and applicability to the organization.
Therefore, the design process should start that puts into consideration multiple aspects of organization’s coding uncertainties, defensive down-coding, inefficiencies of manual processes, overcrowding in the waiting room, and how chronic disease follow-up visits should be, together with slowness in patient flow in the organization.
As a result, attempt should be made to design a system that supports preventive care reminders, patient follow-up activities, labor cost reduction, and ease documentation of data and information.
The plan should further elaborate on how well the team should conduct an examination of workflow. This is where the workflow discrepancies that lead to waste are identified. After that, selection of the right vendor should be the priority. This should be done with consideration of critical functional requirements that collaborative EMR should have.
This process should culminate in training and education of key stakeholders to be affected by the new system (Scott, Rundall, Vogt and Hsu, 2007).
The training and education needs should address the basics of knowledge about the system, how it works, what skills are required, how operation can be carried, how feedback can be realized, and role of system in the organization needs. The training and education period should not be rushed, but progressively carried out to ensure all stakeholders are accustomed to the new system.
In addition, the system’s maintenance and support process should be defined and communicated to stakeholders (Scott, Rundall, Vogt and Hsu, 2007). This involves identifying the back-up systems for the proposed new system, the knowledge of operating, what to do when the system fails, carrying out of continuous maintenance of the system, and the IT expert to ensure the functionality of the system.
This should again be in form of training, education, and awareness activities largely ingrained in the engineering and installation needs of the new system. The next stage to precede this should be outlining clearly, how monitoring, evaluation, and feedback of the whole system will be realized.
This should include outlining, formulating and communicating M& E strategies, together with the feedback system to ensure the system achieve the organization goals.
Conclusion
As it has been established through this study, computerization in the health care industry is necessary and urgent to ensure activities in the industry are successfully executed. EMR remains a challenge in most organization; a majority of them still operate on the old manual system of medical records.
Therefore, it is envisioned that with adoption of new enhanced collaborative EMR system, health care delivery in most hospitals will be faster, accurate, and with fewer errors. Also, the entire process of patient care will be improved and enhanced greatly.
However, realization of success can only be achieved when there is a clear formulated implementation plan that adequately addresses the issues of education and training, system support and maintenance, and M& E and feedback processes of the new system. On overall analysis and evaluation, the new EMR system has the capability to enhance health care delivery in the country if adopted by health care organizations.
References
Berner, E. T. (2007). Clinical decision support systems: theory and practice. NY: Springer.
Goldstein, M. K. (2008). Evaluating Clinical Decision Support Systems. VA HSR&D Cyber Seminar. VA Palo Alto Health Care System and Stanford University. Web.
Green, M. A., & Bowie, M. J. (2010). Essentials of health information management: principles and practices. OH: Cengage Learning.
Jeffrey, W. & Lonnie, B. (2005). Systems analysis and design method. NY: McGraw-Hill.
Lighter, D. E. (2011). Advanced performance improvement in health care: principles and methods. MA: Jones & Bartlett Publishers.
Murray and American Society of Critical Care Anesthesiologists. (2002). Critical care medicine: perioperative management. PA: Lippincott Williams & Wilkins.
Niles, N. J. (2010). Basics of the U.S. health care system. MA: Jones & Bartlett Learning.
Scott, T., Rundall, T. G., Vogt, T. M & Hsu, J. (2007). Implementing an electronic medical record system: successes, failures, lessons. London: Radcliffe Publishing.
Shankar, R.D., Martins, S. B., Tu, S. W., Goldstein, M. K., & Musen, M. A. (N.d). Building an explanation function for a Hypertension Decision-Support System. Stanford Medical Informatics. Web.
Smith, A. L. (2007). Integrated healthcare information systems: Physician based information systems. NY: Lulu.com.
Varshney, U. (2009). Pervasive healthcare computing: EMR/EHR, wireless and health monitoring. NY: Springer.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2009). Health care information systems: A practical approach for health care management. MA: John Wiley and Sons.