Introduction
Continuing care is a term that refers to a wide range of supportive services rendered by health care professionals for the benefit of individuals living either at their homes or at long-term residential facilities providing housing and health care. Nowhere has the application of information technologies been so important as in the practice of medicine in general and in continuing care in particular.
Health cares IT systems have emerged as an alternative for paper-based systems that have dominated the field of medicine for hundreds of years (Weaver, Ball, Kim, & Kiel, 2016). These systems have become increasingly complex and allowed health care practitioners to reduce errors, improve patient outcomes, increase patient safety, and facilitate information sharing, among others. Almost all modern healthcare IT systems fall into four categories: operational systems, clinical and administrative systems, subject and task-based systems, and financial systems (Healthcare First, 2016).
There are also systems that enable complex manipulation of admission, discharge, and transfer data, payment and billing information, and patient clinical records. Usually, health care facilities rely on the use of different software applications that support both health care practitioners and administrative staff in performing their daily duties. However, due to “complex and varying patient care and treatment requirements” (Healthcare First, 2016, para. 7), such fragmentary solutions cannot produce effective results. Given the unique demands of continuing care, such heterogynous IT systems cannot be used across a variety of settings.
The aim of this paper is to outline multilevel continuing care IT system for St. Timothy’s Health Care System. The paper will describe the basic components of the system, explicate challenges associated with its planning and implementation as well as discuss external developments associated with the project.
Purpose of the Project
The main purpose of the project is to make sure that patients can be easily tracked over time and place across all care streams and models. It will help to ensure that health care practitioners have timely and person-centered access to patient clinical data, as well as financial and management data, which will allow managers of the facility to coordinate care, improve its efficiency and reduce the number of unmet health needs.
Also, the project aims to align the provision of continuing care services in St. Timothy’s Health Care System with the principles of case management. According to HQCA (2014), case management refers to a “collaborative process between a health care professional, the client family, and other health professionals who may be involved in the client’s care, including the family physician” (p. 15). Given that continuing care services are provided across different settings, the project will help to ensure that there is a high level of coordination between all involved parties.
Analysis of Continuing Care
The first step that has to be taken to design the system is to analyze the basic structure of continuing care systems and compare it to a method of provision of continuing care services that are utilized by St. Timothy’s Health Care System. Continuing care systems are multidimensional in nature and involve three streams of care: home care, supportive care, and facility care (long-term services) (Weaver et al., 2016). Across these streams of care, various models of care can be offered: adult family care, transitional living care, and group homes, among others.
Home care refers to a set of health care services that support a patient’s health and well-being in their own residential setting. Continuing home care services include, but are not limited to, prevention, screening, evaluation of health status, medication administration, palliative care, home support, rehabilitation, teaching, treatments and health care procedures, and support for family members (HQCA, 2014).
Given that the multilevel continuing care IT system for St. Timothy’s Health Care System presupposes the provision of a wide range of both long-term and acute services, it is important to consider the inclusion of time-sensitive services such as cardiology and coronary care in this stream of care. Supportive care refers to the provision of supportive health care services in a home-like setting. Services that are dispensed at supporting living facilities do not differ from those provided at-home care settings. Facility care is the third stream of care that is usually provided in nursing homes or specialized hospitals (HQCA, 2014).
Clinical Data Electronic Recording
The development of the system is a process that has to be in line with the “fundamental requirements of the clinical data electronic recording” (Santos, Bax, Kalra, 2012, p. 259). Such requirements exist to guarantee uninterrupted access to medical information as well as interoperability with other health care IT systems. The second step that has to be taken when developing the system is to choose a proper interoperability standard.
The interoperability standard that will be used for the project is ISO 13606. The standard is used to ensure that there is an agreement in structure, class, and meaning of data that is being transmitted between different systems Electronic Health Record (EHR) systems (Santos et al., 2012). Given that the multilevel continuing care IT system for St. Timothy’s Health Care System will have to include components of the four major types of health care IT systems, which will make possible their application for clinical, financial, and management purposes, it stands to reason to standardize data that will be used across all domains of care.
Two-level modeling is an approach to interoperability that can satisfy rigid requirements for the clinical data recording. The approach is based on the idea of separating health record data according to its properties: information model and knowledge model. The generic properties of health record data are presented on the information level (Santos et al., 2012). Specific information and its reference to a particular clinical domain, on the other hand, are recorded on the knowledge level. It means that all data that will be used in the system has to be split into two classes, which will be subdivided into more groups according to their origin and destination. To this end, it is necessary to gather multidisciplinary teams that will help to systematize all clinical, management, and financial information.
Archetype Modeling
The process of data systematization or archetype modeling will consist of four steps. The first step is to search for paper and electronic records, clinical guidelines, health care articles, financial records, enrollment files, administrative files, surveys, and other sources of information for possible codes and terminologies. The second step is to group all data elements produced during the first step into coherent concepts. The next step is to develop data archetypes that match the concepts. The final step involves the combination of different archetypes into groups according to particular documentation workflows (Weaver et al., 2016).
The process of archetype modeling has to be discussed by multidisciplinary teams. Most importantly, both data units and archetypes produced during this stage of the system development should be “the result of a consensus among the teams of various clinical specialties” (Santos et al., 2012, p. 262).
Basic Components of the System
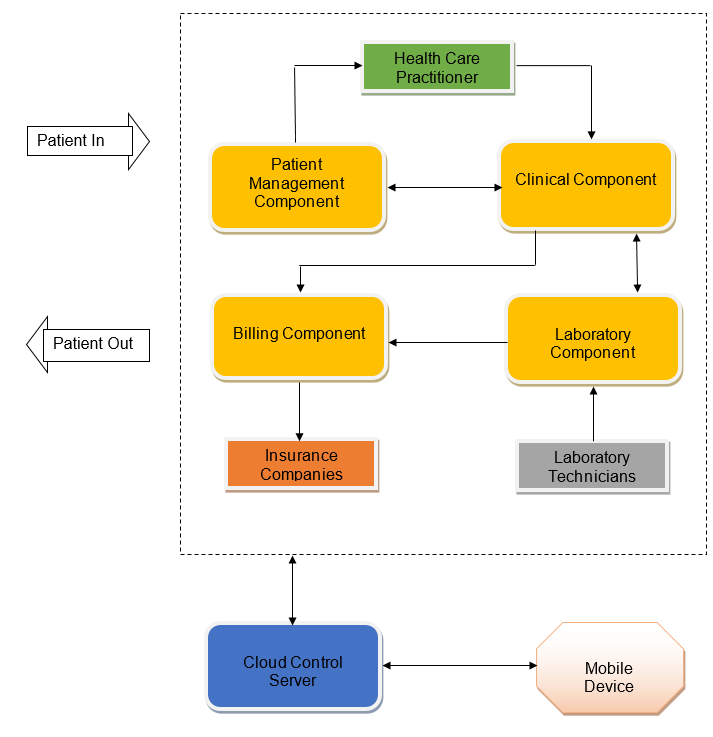
After having established the sources of information and their dimensions, it is necessary to outline the basic components of the system. The system will be based on the principles of software scalability, interoperability, and service-oriented architecture; therefore, its main and ancillary components will have to be self-contained. It means that services such as outpatient admission, billing, or clinical decision support will not depend on the context of other applications (Yang, Sun, & Lai, 2011). Taking into consideration the fact that the system has to perform clinical, financial, and management purposes, it will have the following basic components: patient management component, clinical component, laboratory component, and billing component.
The patient management component is a part of the system that is responsible for managing information related to admission, registration, transfer, and discharge of patients (Weaver et al., 2016). The component will have demographics, insurance, and contact information of St. Timothy’s Health Care System patients. Unique IDs and timetables generated by the component will help to track patients over time and place.
The clinical component of the system will include clinical decision support tools, discharge notes, operative notes, medication administration records, and medical history, among others. This component is necessary to make sure that all patients’ records can be easily accessed and managed. The ease of access is especially important because patients’ data has to be available from a mobile device in case of home care (Accidental Speculation, 2013).
The laboratory component is necessary to provide lab workers with the ability to access and update patient’s records. The component will have to be integrated with the billing component.
The billing component of the system will be used to “capture all charges generated in the process of taking care of patients” (Accidental Speculation, 2013, para. 11). This component will rely on the data from the laboratory component and will be synchronized with the core applications of the clinical component. As it is shown in Figure 1, the information gathered by the billing component will be used by insurance companies.
Challenges
The process of planning and implementing the system is associated with a wide range of challenges and obstacles that will have to be overcome. All health care professionals of St. Timothy’s Health Care System need to have uninterrupted access to the system’s data from both clinical and home care settings. Therefore, the system’s architecture will rely on cloud computing, which will help to increase access agility and reduce infrastructure costs (Padhy, Patra, & Satapathy, 2012).
Another challenge associated with the adoption of the system is the quality and safety of patients’ data. In order to guarantee that the safety of patient’s information is not compromised, the system’s design has to be based on high-quality architecture, certification criteria, and implementation specification of which are controlled by federal regulations (Bowman, 2013).
A lack of support from health care professionals during the implementation stage of the project is a substantial barrier to its success. In order to reduce the resistance of the system users, it is necessary to maximize its perceived usefulness during the development stage. Also, the system implementation will be based on the adoption of the Technology Acceptance Model, which will help to manage health care practitioners’ attitudes towards the system.
According to Pai and Huang (2011), during the development and implementation stages, it is necessary to put emphasis on the following elements of the project: “making sufficient information available, having good interface design and ensuring on-time updating of information on the system” (p. 653).
Other barriers associated with the process of planning and implementing the system include, but are not limited to, availability and utility, audit and archiving, patient consent and authorization, ownership of information, and authenticity and authentication (Chen, Lu, & Jan 2012). Cloud computing will help to overcome these challenges.
External Developments
Recent progress in cloud computing will help to enhance the development and implementation of the project. Cloud computing infrastructure will be used to rent software and computing power, thereby substantially reducing costs and enhancing the safety of the system. Furthermore, the new technology paradigm will provide access to a shared storage pool, which will allow streamlining the maintenance of home care, supportive care, and facility care data (Chen et al., 2012).
Changes in Health Insurance Portability and Accountability Act (HIPAA) is a recent development that might impede the implementation of the project. According to new HIPAA requirements, health care providers are obliged to provide patients with “a written notice about how their health information is used and shared” (Medical Records, n.d., para. 9).
Conclusion
The paper has outlined the process of development of the multilevel continuing care IT system for St. Timothy’s Health Care System. It has presented basic components of the system as well as explicated challenges associated with its planning and implementation. Furthermore, the paper suggested strategies for overcoming implementation barriers and discussed external developments associated with the project.
References
Accidental Speculation. (2013). Basic components of an electronic health record. Web.
Bowman, S. (2013). Impact of electronic health record systems on information integrity: Quality and safety implications. Perspectives in Health Information Management, 10(1), 112-119.
Chen, Y., Lu, J., & Jan, J. (2012). A secure EHR system based on hybrid clouds. Journal of Medical Systems, 36(1), 3375-3384.
Healthcare First. (2016). 4 types of healthcare information systems. Web.
HQCA. (2014). Review of quality assurance in continuing care health services in Alberta. Web.
Medical Records. (n.d.). General overview of EMR regulations for health care providers. Web.
Padhy, R., Patra, M., & Satapathy, S. (2012). Design and implementation of a cloud based rural healthcare information system model. UNIASCIT, 2(1), 149-157.
Pai, F., & Huang, K. (2011). Applying the technology acceptance model to the introduction of healthcare information systems. Technological Forecasting & Social Change, 78(1), 650-660.
Santos, M., Bax, M., Kalra, D. (2012). Dealing with the archetypes development process for a regional EHR system. Applied Clinical Informatics, 3(3), 258-275.
Weaver, C., Ball, M., Kim, G., & Kiel, J. (2016). Healthcare information management systems: Cases, strategies, and solutions (4th ed.). New York, NY: Springer.
Yang, T., Sun, Y., & Lai, F. (2011 ). A scalable health information system based on a service-oriented architecture. Journal of Medial Systems, 35(1), 391-407.