Background
The analysis of the current situation demonstrates that the facility features specific capacity figures that deserve attention. On the one hand, the efficiency of 99% demonstrates that the healthcare organization properly uses all the available resources and does not waste them. On the other hand, the utilization of 98% reveals that the facility does not have free resources. In other words, the obtained figure indicates that 98% of the organization’s resources, including workforce, equipment, and others, are being used for their purposes.
Calculations,
- Efficiency = 295/297 x 100% = 99%.
- Utilization = 295/300 x 100% = 98%.
Determinant Factors
When assessing the organization’s actual output, one should clarify that various determinant factors can affect it. Firstly, ignoring the connection between output and the organization’s size is impossible. The larger a facility, the higher number of patients who can receive adequate care in it.
Secondly, one should look at the financial state of an organization. There is no doubt that those healthcare institutions that do not have economic issues can impress with better output figures (Ridgely et al., 2020). Thirdly, workplace culture can significantly affect the issue under analysis. According to Ridgely et al. (2020), this culture consists of many features, including teamwork, accountability, patient-centered service, and others.
Finally, further essential determinant factors are innovation, leadership, healthcare environment, employees’ skill level, and so on (Ridgely et al., 2020). This information demonstrates that organizations should understand that the stipulated phenomena can significantly affect the organization’s output, denoting that senior management should do its best to control and benefit from them. In particular, promoting teamwork, innovation, and patient-centered can positively affect the organization’s output.
Risk Factors
Different risk factors can result in significant limitations of the facility’s output. On the one hand, it is possible to mention that supplies can be impactful. For example, insufficient or delayed supplies of medicines can denote that the facility cannot provide service to many patients. In addition to that, a failure to receive the required medical tools and appliances in time is a dangerous scenario because it means that the organization can conduct needed testing and examination procedures.
On the other hand, various unexpected events are significant risk factors, and the COVID-19 pandemic is a suitable example. As of April 2020, there were more than 895 thousand reported cases in the United States (Boserup et al., 2020).
Similar to coronavirus, all the other unexpected outbreaks of disease and pandemics are a threat for healthcare organizations. The rationale behind this statement is that these events result in a higher number of patients, meaning that medical institutions are forced to work at full or even extra capacity. In this case, the availability of free resources can make a significant difference.
Recommendation
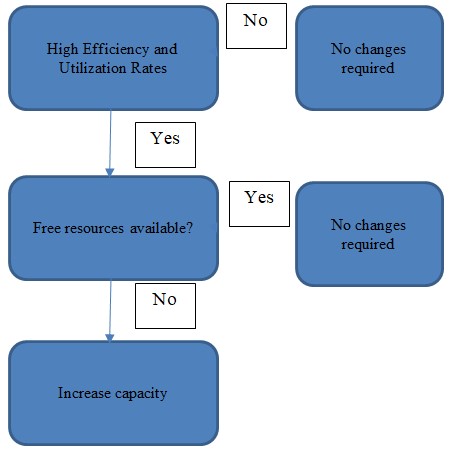
The current rates of efficiency and utilization are sufficient, but one should understand that this conclusion is obtained under the present conditions. The information above demonstrates that numerous factors can change this state of affairs. That is why it is better for the organization to become prepared for such occurrences. Consequently, a recommendation is to increase the current design capacity. The rationale behind this suggestion is that the medical facility needs free resources that can be used to meet an unexpectedly increased demand among patients.
References
Boserup, B., McKenney, M., & Elkbuli, A. (2020). The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. The American Journal of Emergency Medicine, 38(9), 1732-1736.
Ridgely, M. S., Ahluwalia, S. C., Tom, A., Vaiana, M. E., Motala, A., Silverman, M., Kim, A., Damberg, C., & Shekelle, P. G. (2020). What are the determinants of health system performance? Findings from the literature and a technical expert panel.The Joint Commission Journal on Quality and Patient Safety, 46(2), 87-98.