Introduction
A central line bloodstream infection (CLABSI) is a healthcare-related ailment that occurs when bacteria or germs enter one’s bloodstream via a central line, mainly after a catheter is inserted into a large body vein. CLABSI is a severe and potentially life-threatening condition, particularly for people with weakened immune systems. A healthcare facility with effective organizational management will implement the necessary interventions to prevent infection risk during the insertion and maintenance of central lines. The problem of CLABSI is a substantial issue in the healthcare setting and has been linked to increased mortality, healthcare costs, and morbidity (Baier et al., 2020). The report provides an overview of the ABC Hospital, pinpointing the organizational structure, leadership, and communication process. The paper will use the model for improvement framework, including a Plan, Do, Study, and Act (PDSA) cycle to develop an outline for a standardization enhancement pilot project.
Overview of Selected Organization
The healthcare organization selected for the project is a large academic medical center located in an urban setting in Tampa, Florida, United States. The ABC Hospital is a 1040-bed-capacity not-for-profit with highly qualified healthcare practitioners who have contributed to its excellent delivery of healthcare services and enhanced performance (“Pioneering transformative care”, 2023). The hospital has over 8,000 workers, and the facility is one of the largest employers in the area, benefiting many clients (“Pioneering transformative care”, 2023). Notably, people can access healthcare services through its website: https://www.tgh.org/. One of the primary differentiating services offered at the healthcare centre is the advanced cancer care program, which entails clinical trials, surgical oncology, radiation therapy, and cancer genetics.
Organizational Assessment
Organizational Structure
The healthcare organization has a hierarchical structure with clear lines of authority and responsibility. The senior executive comprises the chief executive officer, board of directors, and vice presidents. The ABC Hospital has multiple divisions, such as pharmacy, nursing, radiology, and laboratory, each headed by a departmental director. The hierarchical organizational structure promotes efficient decision-making, sufficient employee communication, and accountability (O’Shea, Boaz, & Chambers, 2019). The general hospital exemplifies a hierarchical structure with a transparent chain of command and authority (“Tampa general hospital”, 2023). The management system is characterized by a top-down approach in decision-making, with power concentrated on the executive team and disintegrated to lower levels. For example, the hospital’s leadership structure consists of the chief executive officer (CEO), the chief operating officer (COO), and the chief nursing officer (CNO), making high-level organizational choices (“Tampa general hospital”, 2023). Such decisions are communicated to the departmental leaders, managers, and frontline workers responsible for executing them.
Leadership Style and Communication
The management deploys the transformational leadership style at the healthcare organization. The CEO and senior executive members emphasize motivating and inspiring subordinates towards achieving a common goal while concentrating on meeting performance metrics and delivering quality patient care, including medically underserved, low-income, minority populace and individuals with limited English proficiency. One of the typical characteristics of the transformational leadership style is individualized consideration, where the leaders listen to each employee’s concerns and demands, thus developing their skills and behaviors while handling patients (Perez, 2021). Another feature of transformational management is idealized influence, where the executive team showcases high standards of moral and ethical conduct, thus improving the trust with employees and making them emulate their actions. The staff members at the ABC hospital follow a formal communication pathway, with the database flowing from the top leadership down to departmental directors and frontline workers (Perez, 2021). Some common conveyance channels the leaders use include emails and meetings to disseminate information among employees at all levels.
Problem of Concern
The problem of concern identified in the healthcare organization is a high incidence of hospital-acquired infections (HAIs), particularly central line bloodstream infections (CLABSIs). According to the statistical reports, the hospital has experienced an average 30-day readmission rate of 18.7%, contrasted to the national benchmark of 15.6% for all-cause readmissions, due to the high rate of CLABSI infections (Baker, Shiner, Stupak, Cohen, & Stoner, 2022). The literature indicates that increased readmission rates are a concern since they show deteriorated care transitions, inadequate quality care, and a lack of coordination between healthcare providers (Baker, Shiner, Stupak, Cohen, & Stoner, 2022). The escalating CLABSIs increase patient readmission rates and may lead to elevated morbidity, mortality, and healthcare costs.
System Contributors
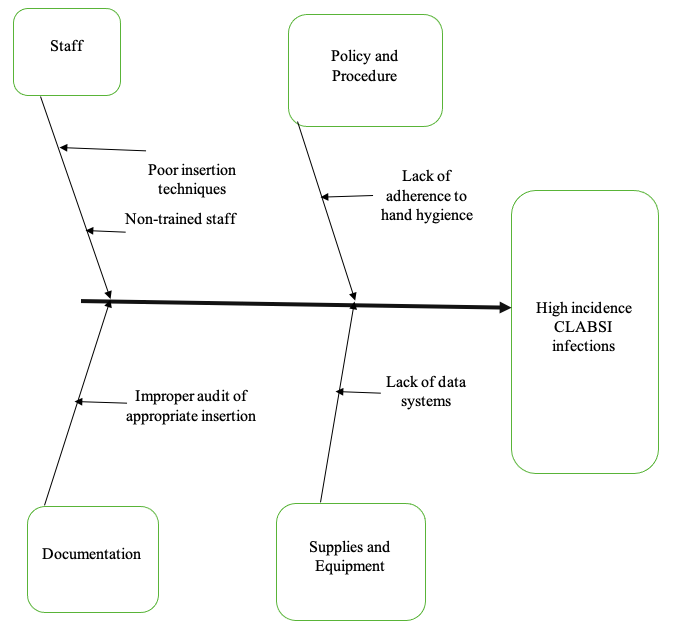
After conducting a cause-and-effect analysis, several unique system contributors to the problem of increased infection rates of CLABSIs were identified at the healthcare organization. Regarding the staff aspect, the lack of adequate subordinate training and deteriorated knowledge of the insertion techniques significantly contributed to the escalated infection levels of CLABSI at the ABC Hospital (Nelson, Huang, & Kuo, 2022). In addition, most healthcare practitioners did not adequately comply with the surgical operation policies and procedures, including adhering to hand washing measures. Concerning the documentation element, the staff members did not conduct the appropriate audit for the proper insertion to avoid transmitting germs and bacteria to the patient’s bloodstream and the central line. The hospital’s inadequate supplies and equipment, involving the absence of data systems that would offer a clear database on the loopholes about hospital-acquired infections, escalated the CLABSI infection rates. Figure 1 illustrates the cause-effect analysis of contributors to increased infection rates of CLABSIs.
Improvement Strategies
To a great extent, the increased infection rate of CLABSI is a substantial cause of mortality, morbidity, and increased healthcare costs, due to massive hospitalizations of patients. However, interdisciplinary professionals suggest multiple strategies to address the concern of CLABSI in healthcare organizations. One of the most effective approaches is the implementation of the central line bundle (CLB). CLB comprises five key elements: maximal sterile barrier precautions during insertion, hand hygiene, daily review and prompt removal of unnecessary lines, and optimal catheter site selection (Kim & Heo, 2019). The studies have showcased that the execution of CLB can significantly reduce the incidence of CLABSI in medical facilities. For example, a survey conducted by Kim & Heo (2019) found that implementing CLB led to a 66% reduction in the incidence of CLABSI in intensive care units (ICUs) across the United States. At the same time, the execution of other strategies, such as antimicrobial-impregnated catheters, minimizes the high infection rates of CLBSI by approximately 70% (Kim & Heo, 2019). In addition, using nurse-led education initiatives enables the workers to acquire the required knowledge regarding the proper insertion of catheters and adherence to hand hygiene policies.
Notably, implementing surveillance programs, such as data systems, enables effective monitoring of the incidence of CLABSI and pinpointing potential outbreaks, resulting in increased readmission rates caused by high infection of CLABSI. Furthermore, statistical evidence indicates that multidisciplinary communication and teamwork are essential to preventing CLABSI. The involvement of nurses, quality improvement personnel, infection control specialists, and physicians in the development and execution of CLABSI regulation programs can improve the effectiveness of the interventions and enhance patient outcomes (DiGiovanni, 2019). Implementing such strategies enables medical practitioners to improve patient safety, minimize healthcare costs, and enhance the overall quality of care.
Model of Improvement
The Model for Improvement is a framework for quality enhancement that offers a structured approach to plan, test, execute, and sustain changes in healthcare settings (Destine, Capes, & Reynolds, 2023). For the project, the improvement team includes the following members: a nurse manager with authority within the system (Eliud Matthews) and a physician champion with technical expertise (Lucy Wells). Other team members are a quality improvement specialist with day-to-day leadership (Georgina Kelly) and a staff nurse representative (George Williams). Notably, all the teammates represent all the processes impacted by the project aim.
Aim of the Project
The pilot project aims to improve the compliance rate of hand hygiene among healthcare workers in the ICU, causing a high infection rate of CLABSI from the current baseline of 60% to 90% within six months. Therefore, the anticipated infection rate will be 3 CLABSI cases per month. The goal of this project aligns with the external benchmarks and guidelines set by the World Health Organization (WHO) and the Centers for Disease Control (CDC). Such organizational management recommends a hand hygiene conformity rate of at least 90% to prevent healthcare-associated infections and promote patient safety (Roshan, Feroz, Rafique, & Virani, 2020). To achieve the project aim, the team will implement a multifaced intervention strategy grounded on evidence-based practices and behavior change theories.
QI Using a PDSA Cycle
Plan
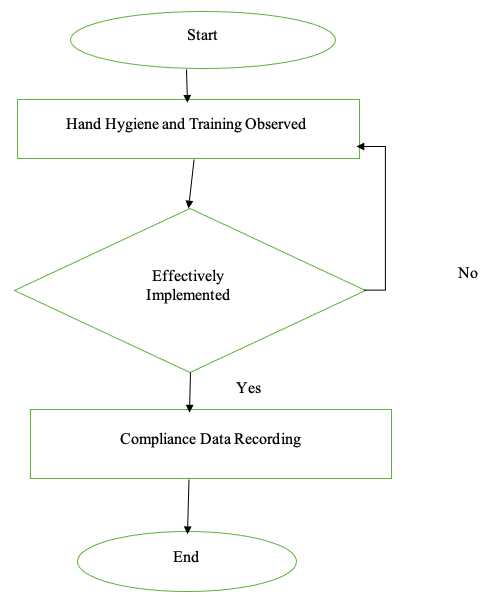
To achieve the project aim, the team will implement a multifaceted intervention strategy based on evidence-based practices and behavior change theories. The project will be undertaken at the ICU of the hospital for six months. Kottler’s 8-step model includes creating a sense of urgency in reducing the infection rate of CLABSI. The team leaders involved in the project include an ICU physician, a nurse representative, a quality improvement specialist, and a nurse manager. The primary barriers involving inadequate staff training and ineffective hand hygiene will be removed through sensitization sessions and having enough gloves, soap and water, and alcohol-based hand sanitizers in the ICU (Nelson et al., 2022). The team will gather data on hand hygiene compliance rates among healthcare workers in the ICU using direct observation and feedback. Figure 2 illustrates the process mapping regarding hand hygiene and staff training.
Do
To implement the project, the team will organize hand hygiene education and training sessions for all healthcare workers in the ICU. The data acquired from the meetings will assess the effectiveness of training, and the observations will be documented via note-taking (Nelson et al., 2022). The project team will meet with hospital administrators to inform them of objectives, timeliness and expected outcomes and secure necessary resources for the project’s success. Notably, to implement a small test of change to start, the team will select a sample of healthcare workers in the ICU. The project group members will train subordinates on proper hand hygiene techniques and compliance with hand hygiene protocols. The nurse manager will be responsible for the implementation process, and the project progress regarding compliance rate will be communicated bi-weekly to stakeholders.
Study
The strategy to analyze data and evaluate progress toward enhancing hand hygiene compliance rate involves regularly monitoring and measuring compliance rates using feedback from healthcare subordinates. The data will be analyzed using statistical methods and comparing the baseline and post-intervention data to determine if the change resulted in the expected outcome. To evaluate progress, the team will create a scorecard to track key performance indicators, such as CLABSI rates and hand hygiene compliance levels (Perez, 2021). If the change results in the expected outcome of increasing hand hygiene compliance to 90% within six months and reducing the CLABSI rates to three cases per month, the team will consider the project a success.
Act
The team will identify additional changes for the next PDSA cycle by reviewing the project’s progress and identifying improvement areas. The team will share this information with the stakeholders, including ICU nurses, infection control nurses, physicians and hospital administrators. The team will communicate the project results to the stakeholders and share the best practices identified during the project’s implementation (Perez, 2021). The group members will document the lessons learned during the project for future reference.
Conclusion
The problem of CLABSI is a substantial issue in the healthcare setting and has been linked to increased mortality, healthcare costs, and morbidity. The involvement of nurses, quality improvement personnel, infection control specialists, and physicians in the development and execution of CLABSI regulation programs can improve the effectiveness of the interventions and enhance patient outcomes. One of the most effective approaches to reducing the infection rate of CLABSI is the implementation of the central line bundle (CLB).
References
Baier, C., Linke, L., Eder, M., Schwab, F., Chaberny, I. F., Vonberg, R. P., & Ebadi, E. (2020). Incidence, risk factors and healthcare costs of central line-associated nosocomial bloodstream infections in hematologic and oncologic patients. Public Library of Science One, 15(1), 227-235. Web.
Baker, S., Shiner, D., Stupak, J., Cohen, V., & Stoner, A. (2022). Reduction of catheter-associated urinary tract infections: A multidisciplinary approach to driving change. Critical Care Nursing Quarterly, 45(4), 290-299. Web.
Destine, Y., Capes, K., & Reynolds, S. S. (2023). Reduction in patient refusal of CHG bathing. American Journal of Infection Control, 17(5), 26-37. Web.
DiGiovanni, S. (2019). A multidisciplinary approach using audits in reducing the rate of catheter-associated urinary tract infections. American Journal of Infection Control, 47(6), 43-57. Web.
Kim, M. H., & Heo, J. (2019). Study on central line bundle cognition, knowledge and performance level of infection management on central venous catheter among intensive care nurses. Korean Journal of Healthcare-Associated Infection Control and Prevention, 22(1), 21-30. Web.
Nelson, E. C., Wang, C. H., Huang, G., & Kuo, N. W. (2022). Institutional factors associated with the incidence rates of central line-associated bloodstream infection in California community hospitals. Public Library of Science One, 17(9), 274-289. Web.
O’Shea, A., Boaz, A. L., & Chambers, M. (2019). A hierarchy of power: the place of the patient and public involvement in healthcare service development. Frontiers in Sociology, 4(7), 38-45. Web.
Perez, J. (2021). Leadership in healthcare: Transitioning from clinical professional to healthcare leader. Journal of Healthcare Management, 66(4), 280-302. Web.
Pioneering transformative care: Innovation is in our DNA. Tampa General Hospital. (2023). Web.
Roshan, R., Feroz, A. S., Rafique, Z., & Virani, N. (2020). Rigorous hand hygiene practices among healthcare workers reduce hospital-associated infections during the COVID-19 pandemic. Journal of Primary Care & Community Health, 11(5), 115-127. Web.
Tampa general hospital. Orgio, Inc. (2023). Web.