Abstract
This paper presents a project on researching the topic of treatment-resistant depression (TRD). The significance of the problem, the project’s aims, the impact that the project may have on the nursing practice, and the coverage of this condition are the primary focuses of this paper. The prevalence of the condition and the innovative ways of its treatment are also elucidated in the paper. It is concluded that, although the problem is steadily being resolved, additional effort is still required.
Introduction
Treatment-resistant depression (TRD) is often referred to as treatment-refractory depression. It is a human condition that is related to some cases of major depressive disorder (MDD). The primary factor separating TRD from other conditions is that the patients diagnosed with this disease do not adequately respond to two or more antidepressants. The term itself was introduced to health care society in 1974 with the development of the concept of treatment-resistant depression.
Naturally, such condition presents a number of challenges to health care specialists (both practitioners and researchers). Although it is not a typical case of clinical depression, this condition also has a particular prevalence that is monitored and measured annually. This paper will focus on describing the condition in general as well as covering certain agents used to treat this type of depression.
Project’s Aims, Goals, Objectives, Relevance, and Timeline
The primary purpose of this project is to provide coverage of treatment-resistant depression and potential ways of its treatment. Therefore, the professional goals that this project will achieve will enhance the development of the role as FNP/PMHNP or Nurse Educator because of the additional understanding created by this project. Description of the issue’s scope, as well as its prevalence and challenges regarding treatment, will provide motivation to research the topic further and create awareness of this problem.
Within the framework of the SMART objectives’ system, the following goals were determined: evaluate the scope of the problem, gather research elucidating the relevance, research currently available means of resolving the problem. It is relevant to achieve these goals due to the fact that TRD affects the communities’ well-being more and more each year. Therefore, the contemporary nursing practice must adjust to this tendency and develop effective ways of overcoming the challenge.
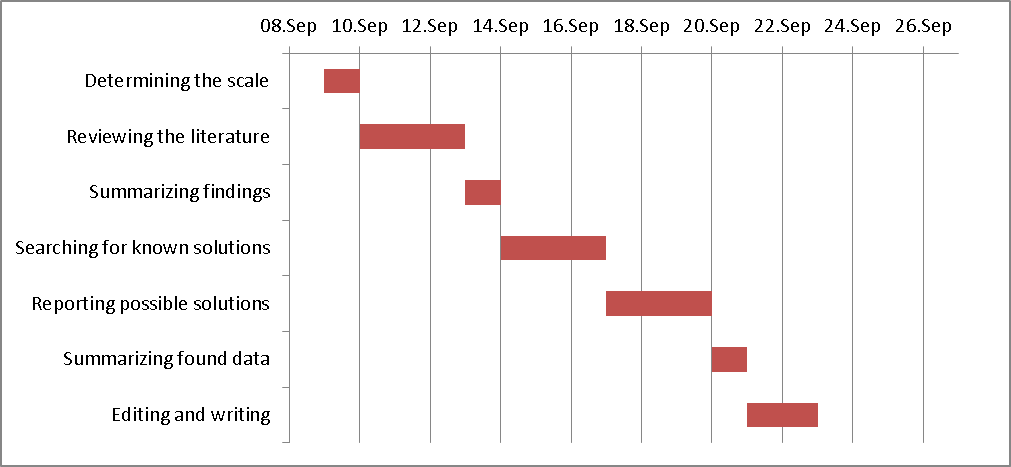
For the goals of this project to be achieved in full, a moderate amount of time is required. The steps mentioned in the figure below represent various stages of this project. The time needed to finish this project is stipulated by the completion of these stages.
Condition’s Review
Depression creates a significant adverse impact on any patient’s life. This statement is even more correct for patients with treatment-resistant depression since their options, as well as their quality of life, are severely limited by their condition. Even if the condition itself is present in a somewhat mild form, its treatment is also able to affect a patient’s life. As stated by Mrazek, Hornberger, Altar, and Degtiar (2014), “treatment-resistant depression may present an annual added societal cost of $29–$48 billion” (p. 977). This will increase the total amount of resources spent to treat major depression by about $106–$118 billion.
Needless to say that such sums are excessive, especially concerning that they are spent to treat only one condition. The authors also note that cases of treatment-resistant depression remain at 12%-20% among depressed patients overall. Therefore, although the prevalence of this condition is not as large, it is safe to assume that these numbers of patients with TRD alone may require significant additional government expenditures to fight off this condition.
Wiles et al. (2013) also note that “depression is a major public health problem. It is predicted to be the leading cause of disability in high-income countries by 2030” (p. 377). The significance of this statement is in the fact that modern health care science is unable to develop an effective approach to treating depression, more so if it is the TRD. There are several attempts at developing treatment measures that do not rely on pharmaceutical means.
Research by Wiles et al. (2013) demonstrates that one of the possible ways to effectively prevent the disease from developing in patients and treat it is cognitive-behavioral therapy (CBT). However, this approach still must be connected to a usual treatment implemented for patients with depression of various types.
An even more distressing report is made by Raison et al. (2013) who states that amongst all cases of clinical depression, about one-third of the patients fail to respond to pharmaceutical treatment. The authors also report that patients with significant inherent inflammatory biomarkers also may suffer from worsening depression-related symptoms. Therefore, some other diseases may also increase the severity of clinical depression.
Morishita, Fayad, Higuchi, Nestor, and Foote (2014) report on a number of invasive treatment methods implemented in the treatment of TRD. The authors state, however, that reports on these procedures lack modern methodology and are, therefore, somewhat unreliable. The authors also note that current surgical treatment is implemented using a number of neuromodulation procedures have also been used to increase a patient’s chances of successful recovery further.
All in all, depression-related disorders and treatment-resistant depression, in particular, are characterized by extremely low recovery chances and a significantly recurrent nature. Costs of treating the condition are at very high levels (about $83 billion annually) (McIntyre et al., 2014). This condition also creates an adverse effect on the quality of life and work amongst patients. It is estimated that companies and their employees lose an average of twenty-seven workdays annually due to depression-related disorders in workers. Individuals diagnosed with depression of various types seldom demonstrate full recovery, and the symptoms are worsening with time and are becoming more and more resistant to treatment with each relapse.
Primary Agents
Across the years of researching depression in general and treatment-resistant depression in particular, researchers have been able to determine the number of agents with different amounts of effectiveness. There are many agents that were proven to work in theory but failed to create any significant impact when implemented directly. Moreover, most of the researches focuses on treating depression in general, while TRD is considered to be an exception and, therefore, is not focused on as much. Nevertheless, health care specialists carry out various researches to test and describe agents that have the potential to allow treating treatment-resistant as well as general types of depression.
One of the particularly advantageous studies is carried out by Murrough et al. (2014). This research’s aim was at performing field tests to determine the amount of effectiveness that ketamine (as an antidepressant) is able to demonstrate when used as a means of treating the TRD. Ketamine was compared to midazolam via distributing it amongst the test group, and its efficiency was confirmed twenty-four hours later. The authors then concluded that ketamine is “further supporting NMDA receptor modulation as a novel mechanism for accelerated improvement in severe and chronic forms of depression” (Murrough et al., 2014, p. 1135). However, the authors also note that this treatment approach must also be further studied mainly due to the fact that the test was implemented in an optimized environment, and the results are yet insufficient to make it possible for ketamine to be fully accepted in clinical practice.
There is also support for ketamine use in treating depression amongst other researches. Since one of the most prominent symptoms of depression (of any type) is suicidal cognition, health care specialists are searching for means to eliminate this symptom along with the condition itself. Price et al. (2014) conclude in their publication that “Intravenous ketamine produces rapid reductions in suicidal cognition over and above active placebo” (p. 336). Although the research itself was carried out in low-risk samples, it is possible to further expand coverage of ketamine as well as its implementation in clinical practice. The authors themselves support this assumption.
In recent years, NMDA receptor modulation became one of the most promising ways to treat clinical depression and even TRD. Ketamine is already supported by a number of the publications mentioned above, and there are other researches that further support its implementation. Shiroma et al. (2014) also note that “repeated infusions achieved superior antidepressant outcomes as compared to a single infusion with different trajectories of response and remission” (p. 123).
This suggests that, at least in low-risk samples, repeated ketamine injections are proved to be both safe and highly effective. This is especially important due to the fact that TRD had often been viewed as a condition that cannot be treated via pharmaceutical means. Researches carried out recently, however, proves otherwise making it possible for health care specialists to implement ketamine in clinical practice. Nevertheless, the experts are mostly advised by the researchers to approach this type of treatment with increased caution.
Zhou et al. (2015) conclude in their research that “quetiapine and aripiprazole appear to be the most robust evidence-based options for augmentation therapy in patients with treatment-resistant depression” (p. 487). The research itself was carried out in a relatively large group of participants (more than 6,600 individuals) which allows assuming that it is reliable enough.
Nevertheless, it is also mentioned that health care specialists must interpret these results with caution since the agents were proven to have severe side effects. Some participants even ceased to take part in the research due to the severeness of effects that they experienced after being exposed to the agents. It is, therefore, up to health care specialists to determine what determines the severeness of the effects and which patients might experience these side-effects.
As already mentioned, neuromodulation – coupled with pharmaceutical and surgical means – may significantly increase the efficiency of any treatment. It is reported by Schlaepfer, Bewernick, Kayser, Mädler, and Coenen (2013) that “bilateral stimulation of the superolateral branch of the medial forebrain bundle may significantly reduce symptoms in treatment-resistant major depressive disorder” (p. 1204). However, some researchers tend to view brain stimulation measures as an addition rather than separate means of treating depression of any type.
Conclusion
It is, therefore, safe to assume that treatment-refractory depression may soon be perceived as a condition that may easily be treated. The studies covering the use of ketamine are the most prominent ones. The authors note, however, that ketamine implementation must be carried out with significant caution as there may be severe side-effects and unforeseen consequences of infusions in high-risk patients. All in all, the severity of TRD is undeniable, and it is only natural that health care science tries to develop as many innovative means of treating it as possible.
References
McIntyre, R. S., Filteau, M., Martin, L., Patry, S., Carvahlo, A., Cha, D. S., … Miguelez, M. (2014). Treatment-resistant depression: definitions, review of the evidence, and algorithmic approach. Journal of Affective Disorders, 156(1), 1-7.
Morishita, T., Fayad, S. M., Higuchi, M., Nestor, K. A., & Foote, K. D. (2014). Deep brain stimulation for treatment-resistant depression: Systematic review of clinical outcomes. Neurotherapeutics, 11(3), 475-484.
Mrazek, D. A., Hornberger, J. C., Altar, C. A., & Degtiar, I. (2014). A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996–2013. Psychiatric Services, 65(8), 977-987.
Murrough, J. W., Iosifescu, D. V., Chang, L. C., Al Jurdi, R. K., Green, C. M., Perez, A. M., … Mathew, S. J. (2014). Antidepressant efficacy of ketamine in treatment-resistant major depression: A two-site randomized controlled trial. The American Journal of Psychiatry, 170(10), 1134-1142.
Price, R. B., Iosifescu, D. V., Murrough, J. W., Chang, L. C., Al Jurdi, R. K., Iqbal, S. Z., … Mathew, S. J. (2014). Effects of ketamine on explicit and implicit suicidal cognition: A randomized controlled trial in treatment-resistant depression. Depression and Anxiety, 31(4), 335-343.
Raison, C. L., Rutherford, R. E., Woolwine, B. J., Shuo, C., Schettler, P., Drake, D. F., … Miller, A. H. (2013). A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression. The role of baseline inflammatory biomarkers. JAMA Psychiatry, 70(1), 31–41.
Schlaepfer, T. E., Bewernick, B. H., Kayser, S., Mädler, B., & Coenen, V. A. (2013). Rapid effects of deep brain stimulation for treatment-resistant major depression. Biological Psychiatry, 73(15), 1204-1212.
Shiroma, P. R., Johns, B., Kuskowski, M., Wels, J., Thuras, P., Albott, C. S., & Lim, K. O. (2014). Augmentation of response and remission to serial intravenous subanesthetic ketamine in treatment-resistant depression. Journal of Affective Disorders, 155(1), 123-129.
Wiles, N., Thomas, L., Abel, A., Ridgway, N., Turner, N., Campbell, J., … Lewis, G. (2013). Cognitive-behavioral therapy as an adjunct to pharmacotherapy for primary care-based patients with treatment-resistant depression: Results of the CoBalT randomized controlled trial. The Lancet, 381(9864), 375-384.
Zhou, X., Ravindran, A. V., Qin, B., Del Giovane, C., Li, Q., Bauer, M., … Xie, P. (2015). Comparative efficacy, acceptability, and tolerability of augmentation agents in treatment-resistant depression: Systematic review and network meta-analysis. Journal of Clinical Psychiatry, 76(4), 487-522.