Introduction
- Hand hygiene – entails routine handwashing, antiseptic or alcohol-based hand rub.
- An effective infection prevention activity:
- Community settings – stops respiratory & diarrheal diseases from spreading;
- The best technique for protecting oneself & family;
- Hospital– prevents HAIs & antibiotic resistance.
- CDC statistics – 2 million patients in US contract HAIs annually:
- Hand hygiene reduces HAI incidence.
Hand hygiene is an effective, evidence-based activity for preventing infections. The CDC-recommended agents for use include soap and water, antiseptics, and alcohol-based sanitizers. In community settings, washing hands can stop the spread of respiratory and diarrheal illnesses. Adherence to this practice can protect individuals and families from communicable diseases. In hospital settings, hand hygiene by providers can prevent hospital-acquired infections (HAIs) and antibiotic resistance. According to the CDC, up to 2 million admitted patients contract HAIs annually in the US. Through hand hygiene, the HAI incidence rate can be reduced.
Indications
- Hands look dirty or soiled – use soap & water.
- Hands not soiled but contaminated – alcohol-based sanitizers.
- After:
- visiting the toilet & touching waste;
- coughing or sneezing.
- Before:
- touching your eyes, nose & mouth;
- Eating.
- For healthcare workers
- Before patient contact & inserting catheters;
- After contact with patient & body fluids.
An opportune time to practice hand hygiene include when hands appear dirty or soiled. In this case, soap and water are recommended since alcohol-based sanitizers may not be effective in killing germs when there is dirt or soil on the skin. Hands should also be washed after visiting the toilet, touching animal waste, coughing, or sneezing. The practice is recommended before eating or touching your eyes, nose, or mouth to prevent respiratory diseases such as Covid-19. For healthcare workers, hand hygiene is required before patient contact, dressing wounds, and inserting catheters and after contact with body fluids.
Causes of Poor Adherence to Hand Hygiene
- Irritation or dryness caused by hand hygiene agents.
- Sinks located far from patient wards.
- Sinks are lacking.
- No hand hygiene protocol.
- Soap & paper towels are not provided.
- Inadequate time – high workloads.
- Prioritizing of patient needs.
- A perception that one handles low-risk patients.
Adherence to hand hygiene practices is often suboptimal in healthcare settings. Many reasons can account for this negative behavior. Hand washing agents that irritate or desiccate the skin will lead to less frequent hand-hygiene practices. Inconvenient location of sinks or a lack of running water, soap, and paper towels can also limit adherence to this routine. Heavy workloads to understaffing reduce the time available to wash hands. The prioritization of patient needs coupled with a perception that one is caring for low-risk patients can lead to non-adherence to hand hygiene practices.
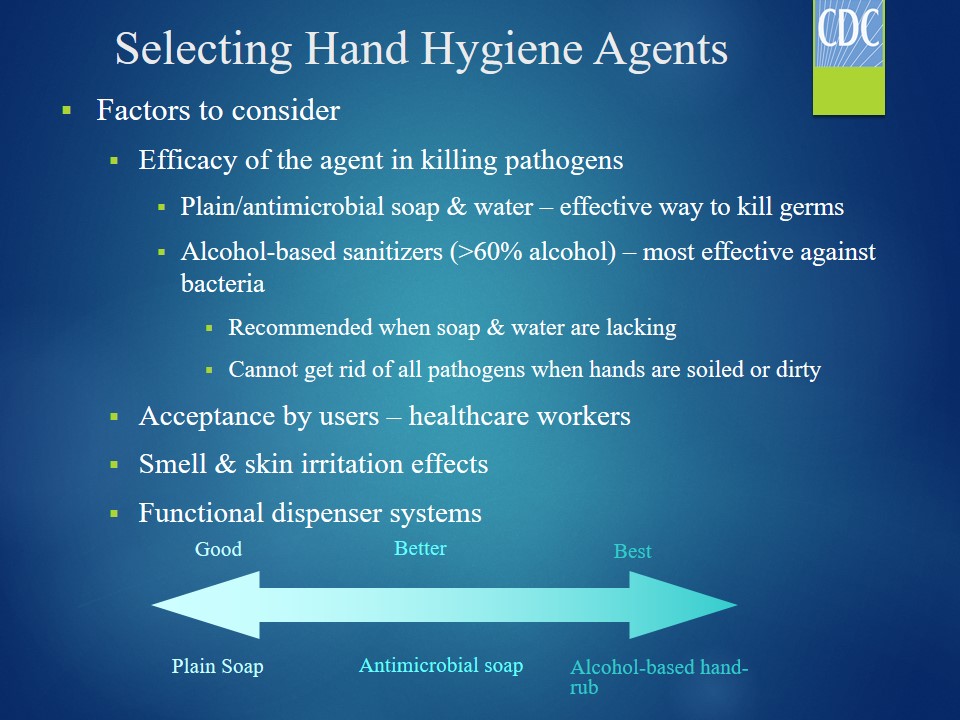
Selecting Hand Hygiene Agents
Factors to consider:
- Efficacy of the agent in killing pathogens:
- Plain/antimicrobial soap & water – effective way to kill germs;
- Alcohol-based sanitizers (>60% alcohol) – most effective against bacteria;
- Recommended when soap & water are lacking;
- Cannot get rid of all pathogens when hands are soiled or dirty.
- Acceptance by users – healthcare workers;
- Smell & skin irritation effects;
- Functional dispenser systems.
The choice of a hand hygiene agent depends on its efficacy in killing various pathogens, accessibility and acceptance by users, and characteristics. Overall, alcohol-based hand-rubs are the most effective means of getting rid of bacteria followed by antimicrobial agents and plain soap. However, they cannot kill all pathogens when used on soiled or dirty hands. Product acceptance by users depends on smell, color, and effect on the skin. Soap dispensing systems should be functional and filled to avoid the risk of contamination.
Recommended Hand Hygiene Technique
- Hand washing – five steps:
- Wet your hands with cold/warm running water;
- Lather hands with soap – fingers, knuckles & nails;
- Scrub for at least 20 seconds;
- Rinse with running water;
- Dry with a clean disposable towel.
- Turn off the valve with the towel.
The recommended hand hygiene technique depends on the agent used. When washing hands, one should first wet his or her hands in cold or warm running water before applying the soap. The next step is lathering up the palms, between fingers, the knuckles, palms, and nails. Subsequently, the hands are scrubbed for a minimum of 20 seconds before rinsing them in clean running water for some time. Finally, a tidy cloth or disposable towel is used to dry them. The same material is utilized to turn off the tap.
Using Alcohol-based Hand-rubs
- Apply gel on the palm:
- Volume – depends on manufacturer recommendations.
- Rub hands together.
- Rub the gel on the back of the hand, between fingers & nails.
- Continue the activity until dry – about 20 seconds.
- Do not wipe the gel off before drying.
Using alcohol-based hand rubs entails three basic steps. First, a small volume of the gel is placed on the palm. Second, the hands are rubbed together to spread the gel on the back of the hand, between fingers, and nails. Third, this activity is continued until the hand-rub dries out, which takes about 20 seconds. One should not rinse or wipe off the gel before drying, as this action will render it ineffective against pathogens. Alcohol-based hand-rubs should have a minimum of 60% alcohol to kill bacteria and other microbes.
Surgical Hand Hygiene
- Antimicrobial soaps or alcohol-based sanitizers are recommended.
- Anti-microbial soap – hands & arms should be scrubbed according to the manufacturer’s recommendations.
- Alcohol-based hand-rubs:
- Hands should be pre-washed with plain soap before applying.
- Adhere to the manufacturer’s recommendations.
Surgical hand-hygiene practice or antisepsis is more stringent than regular hand washing due to the higher risk of contact with microbes, including bacteria. Scrubbing the hands and forearms after applying an anti-microbial soap for a period prescribed by the manufacturer can eliminate all microbes. For alcohol-based hand-rubs, pre-washing hands with plain soap is required before applying the gel. The aim is to remove dirt or grease that may limit the efficacy of these agents. The healthcare professional should apply the recommended volume of the gel and rub the hands until dry before putting on gloves.
Conclusion
- Hand hygiene: an effective infection prevention technique.
- It may entail:
- Washing hands – plain soap & water;
- Antiseptic handwash – anti-microbial soap or detergent & water;
- Alcohol-based hand-rubs – scrubbing hands in sanitizers containing 60% alcohol;
- Surgical hand hygiene – either hand washing (anti-microbial soap) or sanitizers;
- Indicated when hands are soiled or contaminated.
Hand hygiene is a simple, yet effective infection prevention strategy. Different techniques can be used to kill pathogens deposited on hands. Routine hand washing with plain soap and running water can achieve this purpose. Also, using anti-microbial soaps or detergents can eliminate pathogens that cause infection. Alcohol-based hand rubs can also be used when the other agents are not available. Specific protocols for using sanitizers or plain soap have been provided by the CDC. The minimum amount of time one should spend scrubbing the hands, fingers, and nails is 20 seconds. A surgical hand hygiene protocol is also available for healthcare workers in theater settings. It is indicated before and after patient contact.