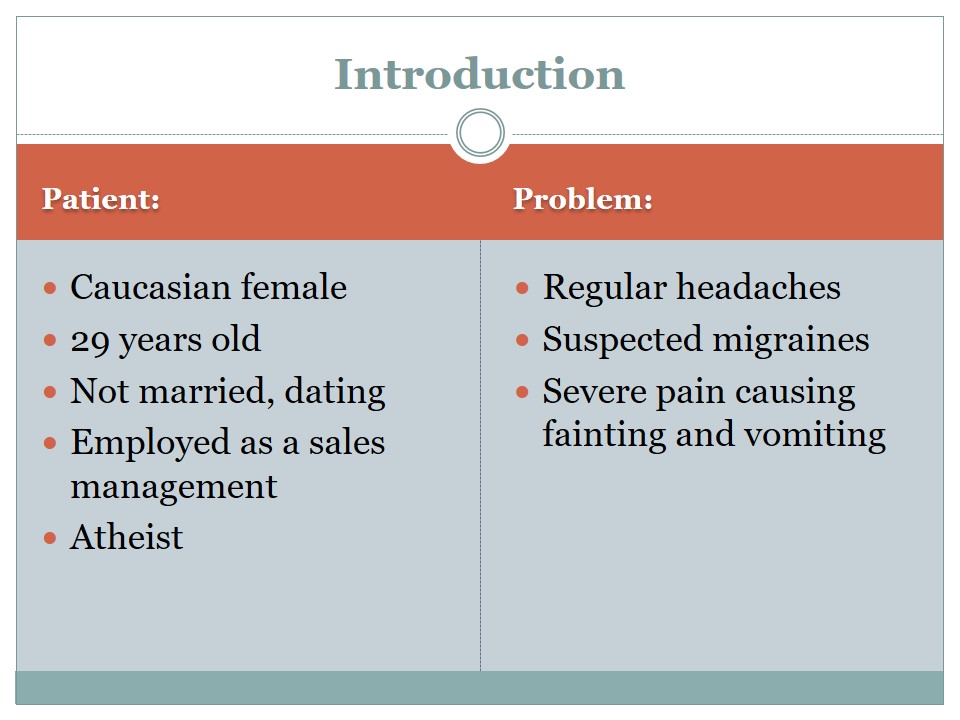
Introduction
- Patient:
- Caucasian female;
- 29 years old;
- Not married, dating;
- Employed as a sales management;
- Atheist.
- Problem:
- Regular headaches;
- Suspected migraines;
- Severe pain causing fainting and vomiting.
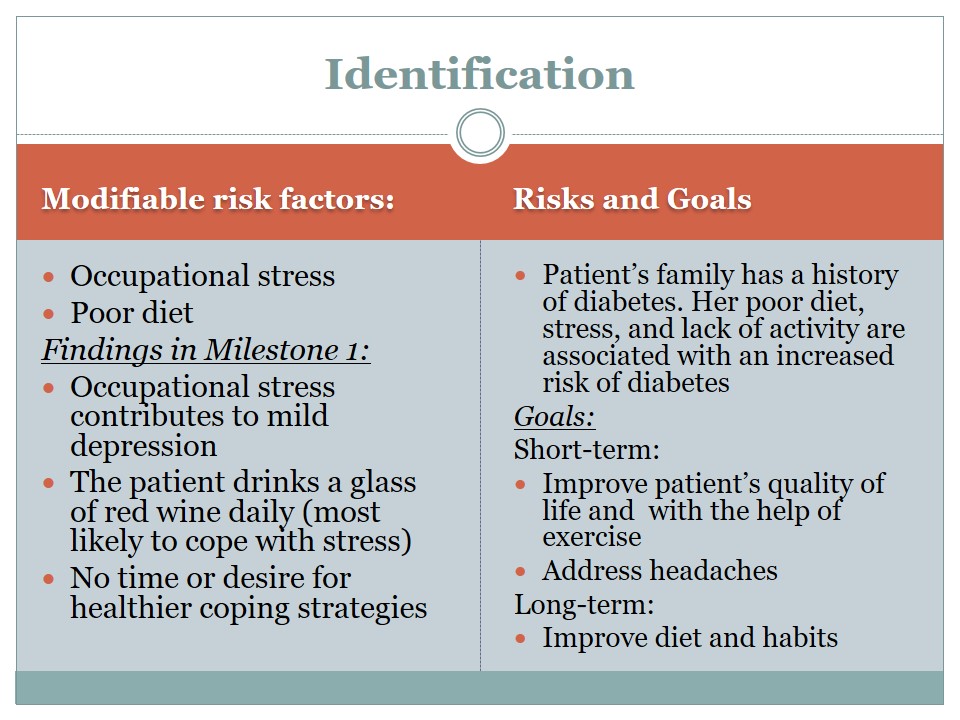
Identification
Modifiable risk factors:
- Occupational stress.
- Poor diet.
Findings in Milestone 1:
- Occupational stress contributes to mild depression.
- The patient drinks a glass of red wine daily (most likely to cope with stress).
- No time or desire for healthier coping strategies.
Risks and Goals:
Patient’s family has a history of diabetes. Her poor diet, stress, and lack of activity are associated with an increased risk of diabetes.
- Goals:
- Short-term:
- Improve patient’s quality of life and with the help of exercise.
- Address headaches.
- Long-term:
- Improve diet and habits.
- Short-term:
Intervention
- Evidence-based practices:
- Physical exercise is helpful for the patients with work-related stress and anxiety (Freitas, Carneseca, Paiva, & Paiva, 2014).
- Physical exercise helps alleviate work and stress-related pains in different parts of the body (Freitas-Swerts & Robazzi, 2014).
- It also helps the workers with stress and burnout feel happier and enjoy a better quality of life (Freitas et al., 2014).
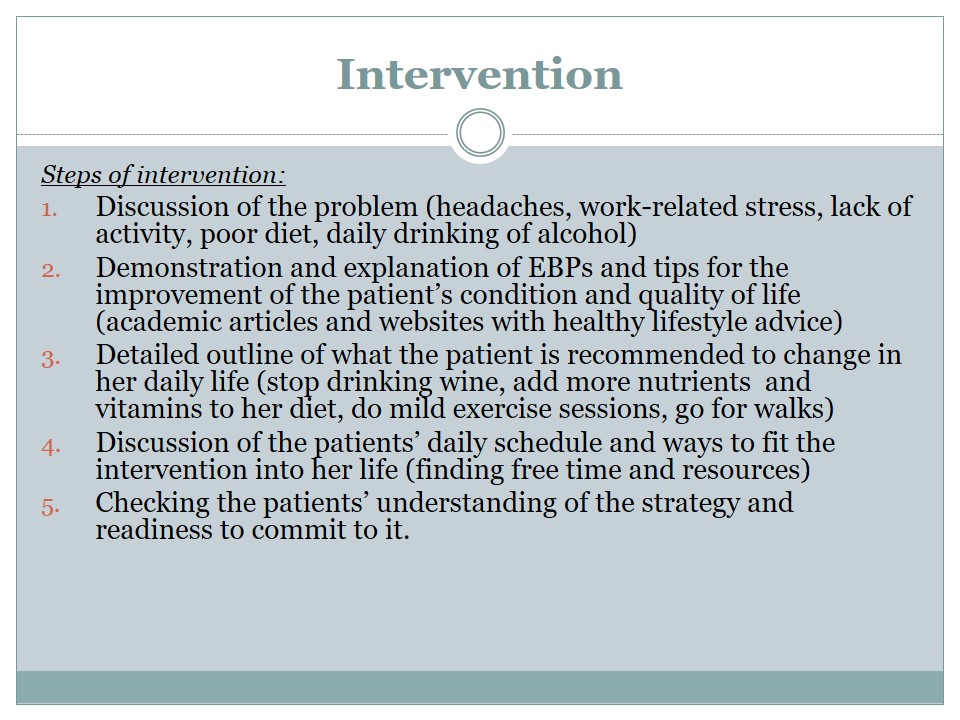
- Steps of intervention:
- Discussion of the problem (headaches, work-related stress, lack of activity, poor diet, daily drinking of alcohol).
- Demonstration and explanation of EBPs and tips for the improvement of the patient’s condition and quality of life (academic articles and websites with healthy lifestyle advice).
- Detailed outline of what the patient is recommended to change in her daily life (stop drinking wine, add more nutrients and vitamins to her diet, do mild exercise sessions, go for walks).
- Discussion of the patients’ daily schedule and ways to fit the intervention into her life (finding free time and resources).
- Checking the patients’ understanding of the strategy and readiness to commit to it.
- Exercise:
- Yoga (beginner level, short routines of 20-25 min);
- Walks (15 min);
- Exercise at work (self-massage of shoulders and neck, moving around the available space, stretching).
- Diet:
- Protein (white meat, fish, nuts);
- Oils in form of capsules (fish oils);
- Herbal teas (ginger root, green, cinnamon, lemon balm);
- Vitamin B complex (“Why your job is causing you headaches—and what to do about it,” 2014).
- Hydration (no less than 1.5 or 2 liters of water daily).
- Final steps:
- Testing the patient’s understanding of the importance of intervention.
- Checking her level of readiness to commit to the practices outlined in her plan.
- Asking her to list her tasks regarding her diet and daily exercise.
- Providing her with a list of necessary practices. Possibly, helping her create a schedule of healthy practices matching her daily routine.
- Offering additional tips for pain and stress and migraine relief options – massage, a visit to a chiropractic, meditation.
During the intervention, the patient will be informed about the likely connection between her occupational stress, overloaded working schedule and her headaches, drinking, and poor diet. Further, a couple of evidence-based practices described in recent academic articles will be used in order to help the patient understand that her problem can be addressed with the help of exercise.
A simple language will be used during the educational session in order to ensure the patient’s understanding of her problem and the required intervention. The latter will be broken down into bullet points and tasks with detailed descriptions and provided alongside a set of tips helping address her issue so that she can choose the strategies that are the most suitable for her daily life.
Since the patient is an atheist but is interested in Buddhism, she may respond well to a suggestion to use yoga as a form of stress release and mild exercise. She could either find time to go to a yoga class once or twice a week or simply try some of the safe and easy routines at home. Also, she will be recommended to go for short but brisk walks on a daily basis or every other day and do other forms of active exercise such as light jogging or cycling (The Migraine Trust, 2017).
As for her diet, she is recommended to consume more protein to improve the level of her energy and also add more oils in her diet and hydrate regularly.
According to Healthy People 2020, only 36% of employees report having access to occupational stress reduction programs (ODPHP, 2017).
The employees suffering from work-related stress and its symptoms need to be equipped to manage the condition independently if their workplace does not provide a corresponding initiative
Evaluation
- Method:
- The patient will be asked to mark the healthy activities in a journal on a daily basis. This would serve as an activity log led by the patient.
- The primary markers of the positive result of the intervention will be the decreased severity of headaches, their diminished frequency, or complete disappearance.
- Also, the patient will be asked to register her headaches and vomiting or fainting incidents and the time when they occur or how long they last.
- Desired Outcomes:
- Minimized severity of headaches.
- Diminished frequency of the headaches.
- Complete disappearance of pains.
- Better moods daily.
- Higher level of satisfaction with day-to-day life.
- Alleviation of the patient’s mild depression.
- A higher level of energy.
- Lower frequency of fainting and vomiting incidents caused by headaches.
- Additional Steps (in case of ineffectiveness of the intervention):
- Evaluation for depression and burnout using standardized assessments and scales.
- Recommendation of therapy for occupational stress.
- If headaches continue or become worse – start assessment for an alternative cause other than occupational stress.
In her activity log, the patient will be asked to put down the activities she accomplished (such as walking, exercise, meditation session) and healthy diet components she added (vitamins, oils, fish, and white meat). She will be requested to mark the time when the practices were carried out and the length of the ones that are lasting (such as yoga session at 11 am – 20 minutes). This approach will help the patient maintain self-discipline and motivation. Most importantly, this method will help me, as a practitioner, see how well the patient followed the instructions. The patient’s records of headache, vomiting, and fainting incidents will help track the improvement (if any) and correlate it with the practices thus identifying the most effective ones.
Summary
- The patient is suffering from headaches and mild depression most likely caused by her unhealthy lifestyle and overloaded working schedule.
- The intervention targets her diet and physical activity as strategies to improve quality of life and reduce stress.
- The patient will be given an educational session focusing on the nature of her problems and the need for intervention.
- An activity log will be used as an evaluation method of the intervention and improvement or lack thereof.
References
Freitas, A. R., Carneseca, E. C., Paiva, & Paiva, B. S. R. (2014). Impact of a physical activity program on the anxiety, depression, occupational stress and burnout syndrome of nursing professionals. Revista Latino-Americana de Enfermagem, 22(2), 332-336.
Freitas-Swerts, F. C., & Robazzi, M. L. (2014). The effects of compensatory workplace exercises to reduce work-related stress and musculoskeletal pain. Revista Latino-Americana de Enfermagem, 22(4), 629-636.
ODPHP. (2017). Occupational safety and health. Web.
Why your job is causing you headaches—and what to do about it. (2014). Web.