Introduction
The operations of a hospital involve various intersecting activities. This paper looks at three major operations of a hospital. The three areas are the alignment of capacity with demand, the measurement of human resource productivity and supply chain management issues in a hospital.
The capacity of a hospital is a critical measure when determining the number of people it should serve. In this sense, the capacity of a hospital must meet the demand for the services provided by the hospital (Jacobs, Rapoport, & Jonsson, 2009). A large unutilized capacity or higher demand than the existing capacity means that the hospital is losing potential revenue. Unutilized capacity raises the fixed costs in terms of human resource outlay and maintenance costs. On the other hand, high demand that outstrips capacity leads to poor services and lost revenue. It can also lead to reputational loss.
On the issue of productivity, it is important for any hospital to understand how well it is utilizing its productive capacity. There is a need for every hospital to consider the value it derives from each employee. This is challenging to achieve in the medical profession because high quality usually means spending more time and attention on a few patients. This reduces productivity when the number of patients served is a factor. In public institutions, productivity is very important because of the expectations of the government.
Finally, supply chain management in hospitals is a very complex affair because of the large volume of inventory. The inventory also varies widely. There is a mix of perishable and non-perishable items, slow-moving and fast-moving items, expensive and cheap supplies, among others (Leeman, 2010). In the case of syringes, the hospital can access certain benefits by using a vendor-managed inventory system.
Analysis
Aligning Capacity with Demand
The alignment of capacity with demand is a very important process in a medical institution. It is imperative to understand the demand patterns for services in any section of a medical facility in order to plan effectively. The section of the medical facility chosen for the alignment of capacity with demand is the ER in a government hospital. The five steps that will help in the alignment of capacity with demand are as follows.
Demand Forecasting
Demand forecasting requires an understanding of the demand patterns of the ER in order to determine future needs. There are several techniques used to determine existing demand, as part of the process of determining future demand. The following data relates to the demand for ER services for a period of seven days. The figures provided are the total number of patients handled in the ER in the given days. For ease of illustration, the figures do not take into account the severity of the conditions of the patients seeking services in the ER.
Table 1: Number of Patients Served in the ER Section
The hospital will serve 33 patients on Monday based on the 3-day moving average. However, the number of patients may be more or less by 4.5 since this is the mean forecast error for the period in review. The value will most likely be lower by 4.5 since the mean forecast error is 4.5. In the same vein, the means absolute deviation of the values considered in the review is 14.83. This is the mean absolute deviation of the 3-day forecast. Table 1 below and figure 1 below display these values.
Table 1: Forecasting using 3-day moving average
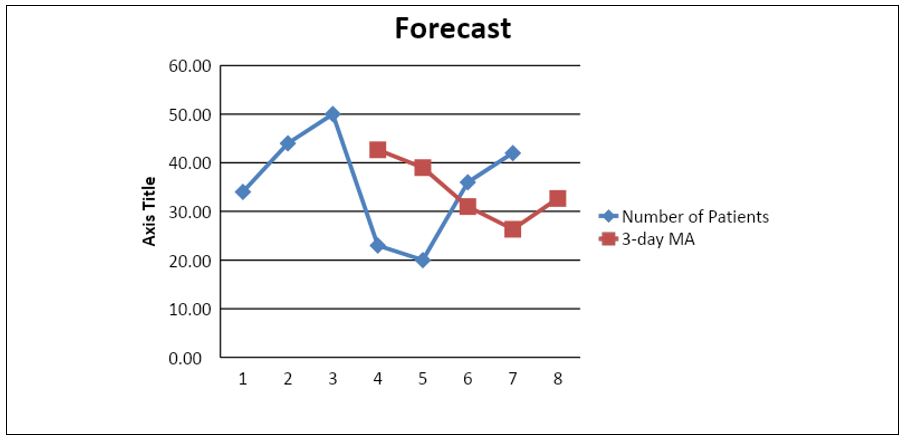
Figure 1: Trend in Demand for ER Services
The graph above predicts that the demand for the next days will be 32.76+-4.5. The likelier figure is 28 patients.
Capacity Requirements
Serving patients in the ER requires the concerted effort of the receptionists, nurses, and ER physicians. All the patients undergo basic checks relating to their heart rate, weight, and temperature at the station of the reception nurse. This nurse then sends them to a queue to await the next available physician. In dire cases, the physicians take the patient in as soon as they arrive at the hospital. The main processes that a patient goes through to receive treatment include registration in the ER reception, measurement of vitals, seeing a physician, and then receiving drugs from the pharmacy (Young, 2009). If the patient requires admission, then the nurses and physicians take over the coordinated care of the patient under the inpatient section of the hospital. All patients must clear their dues if they do not have insurance before releasing from the facility. This means that for the hospital to meet the needs of 37 patients on any day, each section of the hospital must have someone taking care of it. In this sense, the hospital must have a receptionist, a nurse, a physician, a pharmacist and a cashier. The patient spends the most time with the physician. One nurse can serve up to five physicians. One physician can serve up to twenty patients in a day. Therefore, to serve 36 patients, the ER needs at least two physicians, and one emergency response physician to cover any urgent cases. The rest of the service points simply need one person per shift. Therefore, the total human resource capacity needs are as follows.
Table 3: Personnel Demand
Analysis of Current Levels of Capacity
The current level of capacity is very close to the numbers presented in Table 3. The number of physicians varies according to the demand for their services in the ER. The physicians work in shifts with more physicians available during peak hours. It is common to find up to five physicians working for a few hours during peak hours. The number of nurses dedicated to the ER usually follows the number of physicians available at any time. The reason for this is that the rate of services in the ER depends on the speed at which the physicians attend to each patient. One nurse usually remains on standby to handle imminent emergencies to ensure that patients requiring immediate attention receive it as soon as they arrive in the ER.
Estimation of Discrepancy between Current Capacity and Demand
The estimates generated via the forecast presented above show that the ER can work with fewer members of staff if it reduces its capacity to deal with emergencies. Since this is an ER, it is impossible to work with fewer members of staff. However, the need to use the emergency staff never arises more than twice in any one week. This means that the entire quick response capacity of the ER exists to handle a situation that arises only twice a week. It is possible to assign other duties to the staff assigned to quick response roles that they can leave under short notice to maximize the hospital’s human resource capacity. The demand pattern in the hospital is very erratic. The difference in the number of people arriving in the hospital varies by almost one hundred percent across the week. This makes planning very difficult because it is impossible to transfer the extra demand to the next day to regularize services.
Strategy for Aligning Capacity with Demand
The best strategy for aligning capacity with demand seems to be the one already in use. The nature of demand for medical services in the hospital is such that it needs to have the flexibility to handle any spikes or dips in demand. This inevitably leads to an oversupply of labor. However, the risk is not in the oversupply of labor. The risk the ER must plan for is the occurrence of medical emergencies needing a large number of staff members. The current situation where there is an extra physician and nurse on standby to handle any unexpected occurrences is ideal. In addition, the hospital is in a better position to handle emergencies if it has the capacity ready rather than scrambling to find this capacity when the need arises.
Human Resource Productivity Measurement
The most basic expression of productivity is the ratio of outputs over inputs (Flannes & Levin, 2005). However, many measures exist that can help organizations to measure the productivity of their employees. In the medical services sector, measuring productivity is challenging for various reasons. First, the lack of reliable data hinders the measurement of productivity. Unlike some industries, many healthcare institutions do not find it necessary or appropriate to assign quantitative measures of productivity to the activities of key staff. The underlying assumption is that quality care calls for the attention of medical services personnel. Therefore, the use of quantitative productivity measures may affect the quality of the services provided by the personnel in question.
Secondly, the fact that most hospitals are not part of the stock market reduces the incentive for them to publish their productivity measures in the same way that publicly listed companies publish their data (BCG, 2010). This problem compounds the lack of data that can help to calculate the productivity in health institutions. In addition to these issues, productivity measurement usually ignores the quality of services provided. High productivity rates may come at the expense of the quality of services. For instance, for a physician to increase his productivity, it may be necessary to reduce the time spent with each patient. While there are options that can help the physician to achieve this without reducing service quality, the physician can end up hurrying some aspects of care that eventually affect the overall quality of care. The lack of a means of capturing quality issues in productivity leads is one of the fundamental flaws of productivity measurement in healthcare.
Productivity measurement may employ single measures or multiple measures. Since productivity is a ratio, it is a dimensionless quantity (Corson, Heath, & Bryant, 2000). Usually, it is imperative to determine productivity across a period to determine whether a particular value derived from productivity measurement is good or bad. A periodic assessment of productivity can allow a hospital to determine whether the productivity of an employee, department or the entire hospital is increasing or decreasing.
Based on the data presented in Table 1 above, the human resource productivity measurement presented in this section covers the work of one physician and one nurse in one day. The productivity measures chosen are the number of patients served as the output, while the input is the time spent in those two days by the medical personnel.
Table 4: Productivity Data of the Duty Nurse
The overall productivity of the duty nurse in the two days is the ratio of the inputs to the outputs. On Monday, the productivity of the nurse was 4 patients per hour. The rate on Tuesday was 3.5 patients per hour.
The productivity rate for one of the physicians on duty was as follows
Table 5: Physician Productivity Data
The productivity of the physician on Monday was 2.5 patients per hour, while the productivity of the physician on Tuesday was 2.25 patients per hour.
Theoretical calculations show that one duty nurse taking readings of the patients’ vitals can serve up to five doctors. This is because it takes about three minutes to collect the readings from one patient. On the other hand, one physician needs an average of fifteen minutes to serve one patient. The hospital, therefore, allows one duty nurse to every five physicians during the peak shifts. The productivity calculation presented in the table above shows that the duty nurse served only four patients per hour when she has the capacity to serve up to twenty patients per hour. On the second day, the nurse served 3.5 patients. This means that the current capacity of the duty nurse is underutilized. The physician on the other hand only served 2.5 patients per hour on Monday, compared to a theoretical capacity of four patients per hour (capacity utilization was 62.5% ). In the second day, the physician served only 2.25 patients per hour (capacity utilization of 56.25%).
This means that the hospital can increase the number of patients served based on the same resource outlay for the two days. Increasing the productivity of the physician and the nurses depends on the number of patients that come to the hospital. This is entirely out of the hands of the hospital.
Supply Chain
Syringe Supply Chain
One of the items physician use on a daily basis are syringes. Syringes are an essential part of patient care in the hospital. Physicians use syringes to administer treatment to patients. Medical caregivers use syringes to extract blood samples for laboratory tests, inject medicine to patients and in drips, and in rare cases, feed patients with eating problems. Usually, patients prefer to take injections from hospitals rather than from their homes (Jacobs, Rapoport, & Jonsson, 2009). It is possible to train a patient how to self-administer injections. However, many of them, especially those in short-term care or in those admitted for treatment in the hospital prefer when physicians or nurses administer the injections.
The need for syringes is constant. It is possible to determine the quantities needed per unit time. The syringes are also long-lasting. They do not expire quickly as long as they remain in their sterile packaging. The fact that current health standards dictate that syringes are for single use only means that there is a continuous demand for syringes in the hospital. A shortage of syringes can affect care negatively. It is imperative for the hospital to retain a supply of syringes at all times.
The supply chain for syringes in the hospital is as follows. The hospital places an order for fixed quantities of syringes every week. The syringes are not very bulky and do not require special storage conditions provided they remain in their original packaging. The ordering process within the hospital involves the placement of an internal requisition for syringes from the local store by physicians and nurses. This requisition is necessary only if the daily supply runs out. The hospital pharmacy and stores section places an order with the vendors. The hospital uses several types and sizes of syringes. In order to guarantee supply, the hospital maintains two syringe supply contracts at a time. Usually, the contracts cover different sizes of syringes but the vendors must demonstrate the capacity to supply all the sizes of syringes used by the hospital on short notice. This measure guards against the risk of stock-outs in case of supply disruptions affecting one vendor. The vendors receive their syringe supplies from various manufacturers. The vendors have branding and quality contracts with the manufacturers based on the needs of the hospital and the guidelines issued by the Health Department.
Reorder Point and Economic Order Quantity
The Physicians receive a daily quota is syringes from the supplies sections of the hospital. A physician needs to order for a fresh batch only if the current batch runs out. To order fresh syringes, a physician sends an email to the supplies sections requesting syringes. The supplies department packs and sends the required amount of syringes by the physician. The current distributions systems take into consideration the needs of all physicians such that physician reordering is rare.
Historical data from the hospital shows that the hospital uses an average of 300 syringes per day for both inpatient and outpatient care. The efficiency of the suppliers is a maximum of three days from the day of ordering. However, the suppliers typically fill orders within the second day (within 24 to 48 hours of placing the order). Internal hospital policy requires a three-day buffer for all syringes because is the theoretical time it can take the suppliers to resume supplies in case of severe supply chain disruptions. Therefore, the hospital pharmacy and store sections place orders whenever the stock levels fall within three days supply, in addition to the reorder time requirements. This is about six days prior to stock-out. Since the consumption of syringes is not constant, the pharmacy and store section of the hospital orders for fresh syringes each time the quantities drop to 1800 units. The reorder point for syringes is when stocks drop to within a six-day supply of 1800 units of syringes.
Improvement Strategy
The current system is efficient because the hospital never carries more than 1500 syringes at any one time. In addition, the hospital consumes all the syringes supplied within two weeks in the hospital’s supply chain reducing the risk of contamination and pilferage. The management of syringes is a delicate affair requiring prudent use and hygienic handling. The packaging of the syringes usually protects them from physical and chemical contamination. The hospital must regularly inspect the stores to confirm that the syringes are in good condition.
Syringes are low-cost items. The current system uses a supply to stock philosophy. This is ideal for the inventory. Further optimization of the supply chain does not promise commensurate returns. The hospital may increase the quantity of inventory held to cut back on the transport and reorder costs provided the savings are not less than the cost of storage.
Conclusion
The main recommendations to the hospital in relation to the three areas reviewed are as follows. First, the hospital has a greater capacity to treat more patients in the ER section. However, this capacity is available at a high cost to the hospital. The hospital needs to consider methods of deploying the current stand-by staff to other high-need areas such as outpatient services. However, this should come with a rapid deployment plan in case there is a sudden demand for extra capacity in the ER.
Secondly, the evaluation of human resource productivity suggests that the hospital can handle more patients in the ER. The hospital needs to consider marketing its services to increase returns from the current resource outlay.
Thirdly, on the issue of supply chain management, the main recommendation on the procurement of syringes is to deploy a vendor-managed inventory system. This will reduce the warehousing and inspection costs. In addition, it will shield the hospital from legal liabilities associated with contaminated syringes.
References
BCG. (2010). Creating People Advantage in 2010: How Companies can Adapt their HR Practices for Volatile Times. Boston, MA: The Boston Consulting Group.
Corson, D., Heath, R. L., & Bryant, J. (2000). Human Communication Theory and Research: Concepts, Context, and Challenges (2nd ed.). Mahwah, NJ: Lawrence Erlbaum Associates, Inc.
Flannes, S., & Levin, G. (2005). Essential People Skills for Project Managers. Vienna, VA: Management Concepts.
Jacobs, P., Rapoport, J., & Jonsson, E. (2009). Cost Containment and Efficiency in National Health Systems: A Global Comparison. Weinheim: Wiley Verlag.
Leeman, J. J. (2010). Supply Chain Management: Fast, Flexible Supply Chains in Manufacturing and Retailing. Dusseldorf: Books on Demand.
Young, S. T. (2009). Essentials of Operations Management. London: Sage Publications Inc.