Introduction
- Emerging Field in the Area of Nursing Competencies;
- Digitalization of Nursing Protocols;
- Information Sharing;
- Many Instruments and Machines are Computerized;
- Present a New Set of Requirements and Challenges.
Modern healthcare is one of the most organized and regulated fields of industry. With peoples’ lives on the line, healthcare workers require every bit of information they could get in order to establish a proper diagnosis and facilitate treatment. Healthcare has seen immense progress in the past several decades, making a leap from paper documentation to computerized databases. MRI, PET and CT scanners, x-ray machines, and many other instruments now operate using specialized software. With the integration of computer systems into healthcare, nursing informatics became even more relevant than before. This presentation will provide an overview of nursing informatics, its history, organization, theoretical background, and systems life cycles.
What is Nursing Informatics?
- Integrates computers into hospital routines;
- Caring: Operation of computers and data analysis;
- Sharing: Transfers of patient data and formulating a coherent health picture;
- Comparing: Tracking progress and conducting research (McGonigle & Mastrian, 2015).
Nursing informatics is an emerging area of healthcare competencies that dedicates itself to integrating computerized and information-sharing systems into hospital routines, enabling nurses and patients to benefit from quick and secure transfer, analysis, and use of personal data, medical data, and any other information required to achieve a higher quality of care. The basis of nursing informatics is formed around the concepts of Caring, Sharing, and Comparing information (McGonigle & Mastrian, 2015). The caring aspect involves operating all kinds of computerized instruments and machinery as well as software used in analyzing patient data. Sharing stands for transferring patient data to healthcare professionals in different hospitals. Comparing stands for research as well as analysis of the patient’s progressive healthcare records. Nursing informatics is a relatively new field of expertise, with its own set of laws, regulations, and demands towards patient and data security.
History of Nursing Informatics
- Finds its routes in the standardized record and documentation system (Collen & Ball, 2015).
- Concepts were established in 1970s.
- First put into practice in the 1980s.
Although the term “informatics” is relatively new, the basics of the modern discipline were established by Florence Nightingale, who outlined the use of technology in medicine as a systematic treatment and as a scientific method of approaching clinical situations. Doctors around the world have understood the usefulness of a functional bureaucracy and the standardization of patient files, enabling other healthcare professionals to understand what was being done on a systematic basis. With the advancement of computers and the internet, it became possible to move the bureaucracy into the digital space, making it faster and more efficient. First ideas of utilizing modern electronic technology in medical records have appeared in French medical journals in the 1970s, which were then transferred to nursing a decade later, once personal computers started appearing in the market (Collen & Ball, 2015).
- International viewpoint established in 1998.
- Standard of practice in the USA since 1995 (Piscotty, Kalisch, & Gracey-Thomas, 2015).
- In 2018, 15% of the entire workforce are Informatics Nurses (Collen & Ball, 2015).
The American Association of Nurses (ANA) had been persistent in its integration of computers into the hospital system. By 1995 nearly all hospitals had at least several personal computers used to store databases and process files. It required the establishment of new standards of practice for the emerging Informatics Nurse profession. A certification commission helped expand the individuals operating these machines beyond the generalist practitioner, and certifying over 400 nurses within the first year (Piscotty et al. 2015). With the digitalization of healthcare and various government policies like the electronic healthcare record initiative, the number of informatics specialists grew larger. As it stands, over 15% of the entire nursing staff have either majored or minored in nursing informatics (Collen & Ball, 2015).
Nursing Informatics Theories
- Initially based on the Four Metaparadigms of Nursing.
- Information and Communication Technology Acceptance Model (ICTAM).
- Multidisciplinary approach makes it difficult.
- Lack of solid ethical models to guide nurses (Korhonen, Eriksson, & Nordman, 2015).
Nursing informatics is a complex and relatively new field of practice that interconnects medicine with various other fields, such as technology, physics, engineering, and social work. Although nursing informatics were based on the four metaparadigms of nursing, they did not have any established frameworks from time to time. Technology was used by nurses as they saw fit, which created a great degree of variance between practices. The ICTAM model is based on 5 parameters, which include the subjective norm, image, output quality, result demonstrability, and compatibility in order to integrate technology into healthcare. However, the ethical part of using technology and informatics in healthcare remains a gray area (Korhonen et al., 2015).
- Empowerment Informatics Framework (Knight & Shea, 2013).
- Examines health-enabling technologies.
- Has an informatics-based perspective.
- Too narrow and does not encompass the whole field.
Knight and Shea (2013) have provided the medical community with a patient-focused self-management framework, which utilizes healthcare benefits as primary foundations for determining the usefulness and ethics of implementing IT technology. It justifies the use of technology by perceiving potential benefits to patients either directly or indirectly. Direct benefits are provided through self-care and self-management techniques which enable patient autonomy. Indirect benefits come from assisting doctors and nurses, which, in turn, help the patients get better. However, the limit of this theory is that it is focused on long-term chronically ill patients and cannot be completely extended to envelop the entire field.
Systems Development Life Cycles
- Waterfall Model (“Nursing informatics,” n.d.).
- Feasibility;
- Analysis;
- Design;
- Implementation;
- Testing;
- Maintenance.
As nursing informatics is constantly being updated and improved, system development life cycles need to be implemented in order to decide how and what to develop in the scope of the industry, the region, or even a singular healthcare institution. The Waterfall Model is an old and very simple tool, which can be implemented in a variety of healthcare settings (“Nursing informatics,” n.d.). It starts with the feasibility stage, which helps determine if the project is needed and sustainable. The analysis stage helps flash out the requirements for a particular system or project. Design stage is responsible for data and interface decisions. Implementation means creating the program or a system using the appropriate hardware and software. During the testing phase, any potential errors and misconfigurations are ought to be found. Maintenance concerns itself with keeping the system operational in its day-to-day use.
- RAD – Rapid Application Development (“Nursing informatics,” n.d.).
- Lifecycle used for short-term applications and prototypes;
- Quick to develop;
- Fits a tight schedule;
- Lacks pre-testing.
The RAD lifecycle is used in situations when a hospital requires a nursing informatics implementation urgently, in order to fit a tight schedule or budget. It consists out of the same steps as the waterfall schedule, with the difference being that design and implementation are molded into a single function (“Nursing informatics,” n.d.). Additionally, any pre-testing is being placed on the shoulders of the users, who are supposed to return information about any quirks or malfunctions. The lack of testing makes these prototype systems vulnerable to security breaches.
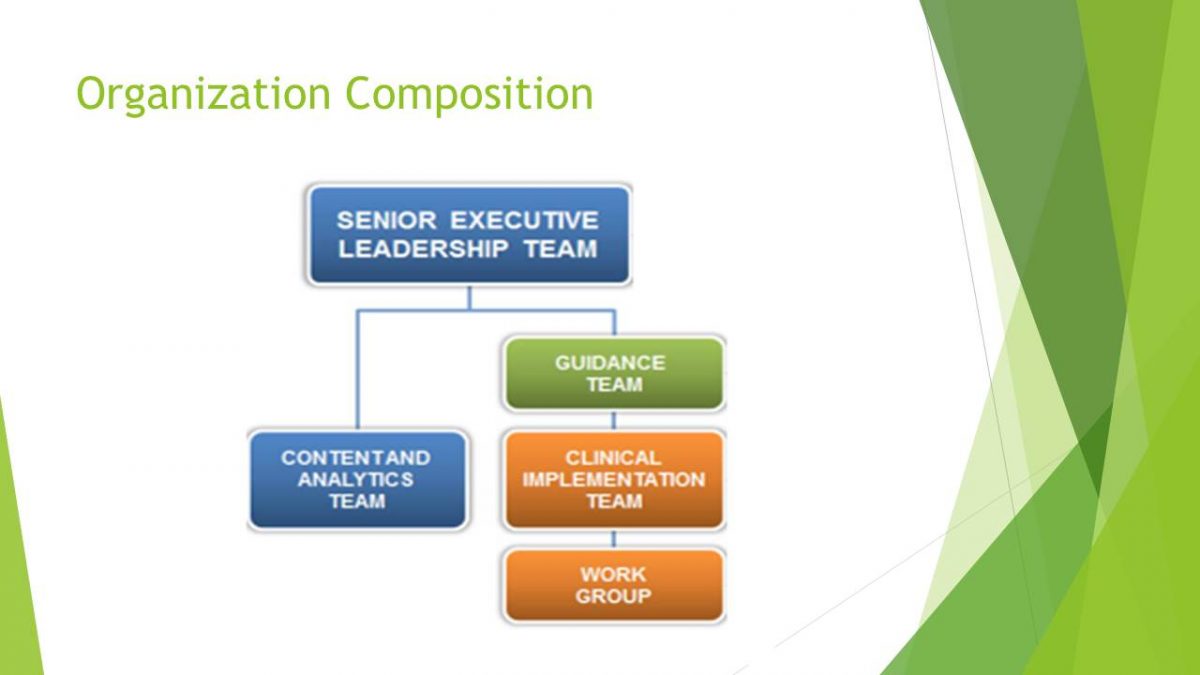
Organization Composition
In a hospital setting, the organization composition for nursing IT looks as follows (“Nursing informatics,” n.d.):
- Senior executive leadership team. Provides overall governance and prioritization of initiatives.
- Content and analytics team. Supports development of critical content and analytics feedback.
- Guidance team. Provides steady state domain and oversight.
- Work group. Provides clinical forum to develop content and analytics feedback.
- Clinical implementation team. Refines work group output and leads implementation.
Conclusions
- Nursing Informatics is necessary for facilitating a high quality of care;
- The area requires better theoretical frameworks;
- Internet security and privacy concerns are ought to be addressed;
- NI must continue to evolve.

References
Collen, M. F., & Ball, M. J. (2015). The history of medical informatics in the United States (2nd ed.). New York, NY: Springer.
Knight, E. P., & Shea, K. (2013). A patient-focused framework integrating self-management and informatics. Journal of Nursing Scholarship, 46(2), 91–97.
Korhonen, E., Eriksson, K., & Nordman, T. (2015). Technology and its ethics in nursing and caring journals: An integrative literature review. Nursing Ethics, 22(5), 561-675.
McGonigle, D., & Mastrian, K. (2015). Nursing informatics and the foundation of knowledge (3rd ed.). Burlington, MA: Jones & Bartlett.
Nursing informatics administrative applications: Precare and care support. Web.
Piscotty, R., Kalisch, B., & Gracey-Thomas, A. (2015) Impact of healthcare information technology on nursing practice. Journal of Nursing Scholarship, 47(4), 287-293.