Introduction
As De Herdera et al (2006, 183-184) argue, although the insulinomas are the primary functioning syndromic subclass of the endocrine pancreatic tumors, they are the most uncommon subtype of tumors of the neuroendocrine family. These tumors grow in the insulin producing beta cells; hence, play a central role in regulating the body’s blood glucose levels, through producing insulin. Most tumors of this form mostly occur as isolated benign pancreatic nodules; hence, it is very rare to find cases of patients with multiple Insulinoma tumors.
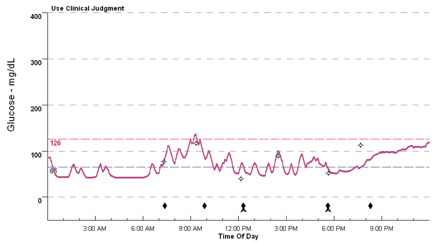
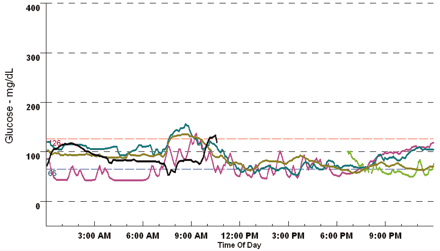
Failure by these tumors to regulate the amount of insulin produced can cause a reduction of the amount of the blood sugar to unhealthy levels hence, leading to a health complication called hypoglycemia. In most cases, most individuals tend to confuse symptoms of low blood sugar levels with psychosis hence, unless doctors perform the require tests, chances of misdiagnosis are high. On the other hand, as clinical tests on patients with diabetes show, there is a small correlation between diabetes and insulinoma, although both are result due blood sugar level anomalies (Refer to figure 1 and 2).
Unlike other body tumors that are cancerous, only a small portion of insulinomas are cancerous (less than 10%), therefore Insulinoma is curable condition. Considering this, to avoid the occurrence of side effects or health complications that may occur due to reduced blood sugar level, it is important for individuals to seek medical attention once they experience neurological and psychiatric symptoms.
Historical Background
The first documented case of Insulinoma was discovered in 1923, by Campbell and Fletcher. This led to a first surgery case to remove an Insulinoma from a patient in 1927, by Mayo. Later on in 1938, the Whipple wrote the first publication on Insulinoma; hence, opening room for more medical researches to discover the condition fully. In 1954, through the help of other medical researchers Werner documented the first case of a family with multiple endocrine neoplasia (a medical condition closely related with gastrinomas). Due to these development and need to discover more about Insulinoma, medical researchers organized collective seminars, whose findings gave birth to the present developments in treatment of Insulinoma (Moses, (n.d.), p.4).
Signs and Symptoms of Insulinoma
Insulinoma almost shares the same symptoms with psychosis, although doctors can differentiate the two through thorough medical examination. Insulinoma is primarily characterized by sympathoadrenal and neuroglycopenic symptoms, which are primarily triggered by hypoglycemia. These symptoms include persistent headaches, lethargy, occasional seizures, neurological damages, blurred vision, diplopia, and in untreated cases, it can cause comas and excessive weight gain. In addition, symptoms associated with catecholaminergic reactions to hypoglycemic, for example, sweating, queasiness, quivering, and tremulousness, can also indicate the presence of Insulinoma (Ebady, Arami, & Kucheki, 2005, p.1).
Cytology and immunohistochemistry
The primary components of Insulinomas are single cells that have an eccentric nuclei and a granular cytoplasm. Hence, because the normal islet cells have the same characteristics, it is usually very hard for one to differentiate the two by only using an electron microscope. Most insulinomas have a smaller quantity of insulin than beta cells hence, in most cases, the overproduction of insulin by insulinomas occurs due to the inability of the cells to control the storage and secretion of insulin. The storage and release problem, rather than overproduction forms the primary basis of diagnosing the tumors, because of the excessive amounts of proinsulin (un-metabolized insulin) in Insulinoma cells (Moses, (n.d.) pp.6-7).
Diagnosis
To diagnose Insulinoma correctly, doctors must ascertain the presence of three primary conditions (common called Whipple’s conditions). These conditions include a patient must exhibit distinct signs of hypoglycemia, a patient should have a plasma glucose amount of 45mg/dl or a more reduced amount, and a patient must show sings of acquiring their normal health status when given glucose. If a patient meets these conditions, then a patient will undergo a series of blood tests to test the level of insulin, glucose, and C-peptide in the blood. In addition to this, doctors can use suppression tests that require fasting under close supervision of a medical practitioner.
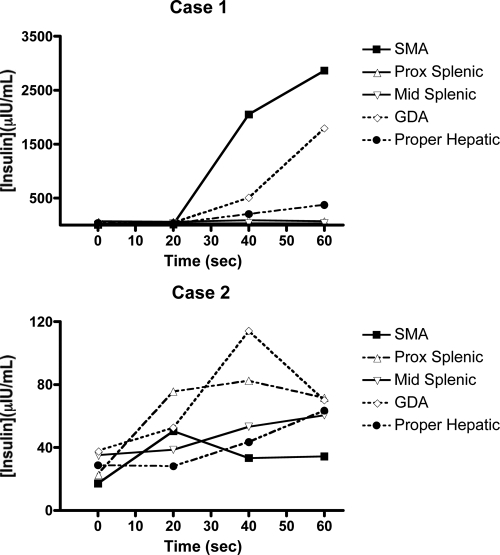
Other common diagnostic methods include using ultra sound, Computed tomography scans, infusion of calcium, pancreatic vein catheterization, and use of magnetic resonance imaging to localize the tumor. (De Herdera et al, 2006, pp. 184-186) Although all these methods can give dependable results, for proper tumor localization, most doctors prefer to use calcium arterial stimulation (CaStim), using calcium infusions (Guettier et al, 2009, pp. 1074-1080). (Refer to figure 3)
Treatment
The most definitive method of dealing with the complication is through the use of a surgical operation to remove the tumor and its capsule. In cases where it is impossble to use enucleation, medicsa can remove some sections of the pancrease (the affected), or conduct a distal pancreatectomy or pancreaticoduodenectonmy to remove the tumor. On the other hand, treatment remedies for patients with unoperatable tumors include, use of medications, for example, diazoxide and somatostastatin.
This medication helps the body to inhibit the production of insulin. Further, the most recommondable remedy for patients with metastasizing tumors that are charactrised with intrahepatic growths, is the use of heraptic arterial occlusion or embolization (a non-surgical procedure of treating the affected area) (Shah, Patel, Prajapati, Modi, Sharma, & Arora, 2010, p.1).
Reference List
De Herdera, W., et al. (2006). well-differentiated pancreatic tumor/ carcinoma Insulinoma. Neuroendocrinology, 84, 183-188. Web.
Ebady, S. E., Arami, M. A., & Kucheki, E. (2005). A case of Insulinoma with Neuropsychiatric Symptoms and celebral infarction. Internet Journal of Neurology, 4(2).
Guettier, J. M., et al. (2009). localisation of insulinomas to rwegions of the PAncrease by interarterial calcium stimulation: the NIH experience. Journal of Endocrinology Metabolism, 94(4), 1074-1080. Web.
Moses, S. K. (n.d.). Insulinoma: a review and an update. Web.
Sapountzi, P., Charnogursky, G., Emanuele, A., Murphy, D., nabhan, F., & Emanuele, N. V. (2010). case study: diagnosis of insulinoma using continuous monitoring systemin a with diabetes. Diabetes Journal, 28(3). Web.
Shah, S. V., Patel, A. M., Prajapati, J. A., Modi< A., Arora, R., & Sharma, P. (2010). Insulinoma: a commonly misdiagnosed pancreatic tumo., Journal of Gastroenterology, 9(1).