Introduction: Pathophysiology of Osteoarthritis (OA)
- OA: joint disease, chronic, inflammatory.
- The main cause: unknown (Ashkavand, Malekinejad, & Vishwanath, 2013).
- The most widespread form of arthritis in the USA.
- There is no cure.
- Treatment can relieve the symptoms (Woo, 2016).
The main cause of OA is not known, but patients demonstrate such morphological changes as inflammation and cartilage erosion (Ashkavand et al., 2013). The most common signs and symptoms of OA are the stiffness in joints, the weakness in muscles, pain, and the enlargement or swelling of bones. Risk factors for the disease include age, gender, diet, and genetic hormones (Ashkavand et al., 2013). Typically, joint pain gets worse with activity and weight-bearing, whereas the improvement occurs when a patient has enough rest (Woo, 2016). While there is no cure for OA, the appropriately selected treatment can relieve the patient’s condition by minimizing the functional impairment.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Pharmacodynamics
- The most common over-the-counter drug for OA.
- NSAIDs constitute one of the most common types of treatment of OA.
- NSAIDs help to preserve activity in pain, inflammation, and fever.
- The need for opioid analgesics is reduced.
- NSAIDs help to avoid addiction and chemical dependency (Woo, 2016).
Irrespective of the injury, the inflammatory response is similar. When cell membranes are destroyed, chemical mediators are released, such as prostaglandins, histamine, cytokines, leukotrienes, enzymes, and oxygen radicals (Woo, 2016). Two main enzymes, cyclo-oxygenase and lipo-oxygenase are needed to produce the mentioned mediators. The main mechanism of NSAIDs is considered to be the inhibition of cyclo-oxygenase activity and prostaglandin synthesis (Woo, 2016). Other factors that may be observed include the inhibition of lipo-oxygenase, lysosomal enzyme release, neutrophil aggregation, leukotriene synthesis, and different cell membrane functions (Woo, 2016).
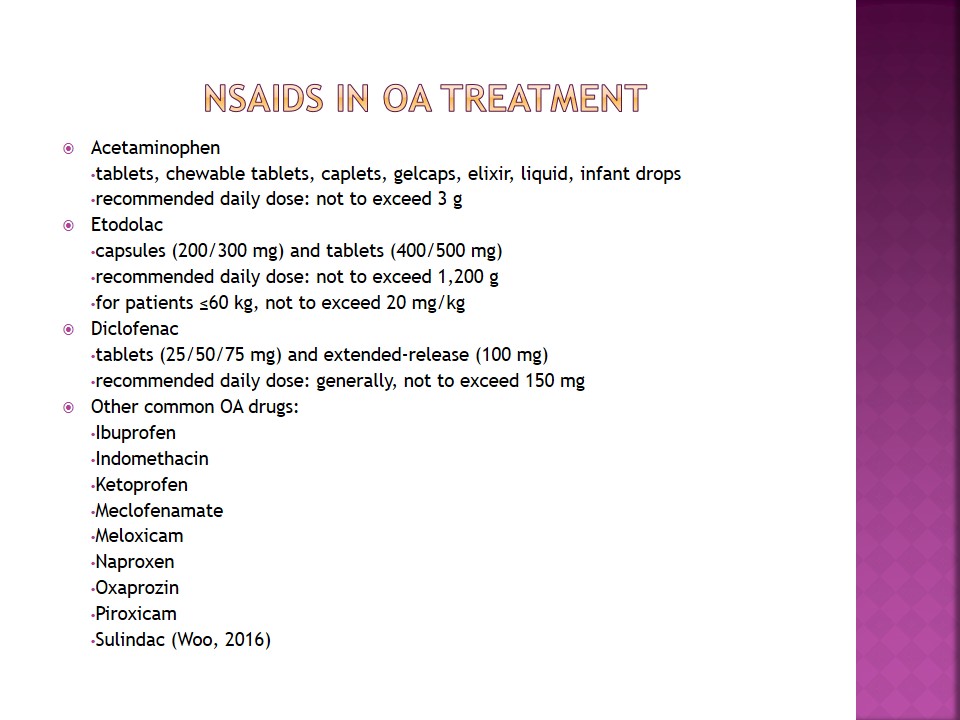
NSAIDs in OA Treatment
- Acetaminophen:
- tablets, chewable tablets, caplets, gelcaps, elixir, liquid, infant drops;
- recommended daily dose: not to exceed 3 g;
- Etodolac:
- capsules (200/300 mg) and tablets (400/500 mg);
- recommended daily dose: not to exceed 1,200 g;
- for patients ≤60 kg, not to exceed 20 mg/kg;
- Diclofenac:
- tablets (25/50/75 mg) and extended-release (100 mg);
- recommended daily dose: generally, not to exceed 150 mg;
- Other common OA drugs:
- Ibuprofen;
- Indomethacin;
- Ketoprofen;
- Meclofenamate;
- Meloxicam;
- Naproxen;
- Oxaprozin;
- Piroxicam;
- Sulindac (Woo, 2016).
The initial pharmacological treatment of OA includes 650 mg of acetaminophen four times a day or 1 g three times a day (Woo, 2016). Such an approach allows managing joint pain and relieving other symptoms. However, if this drug cannot produce positive results, NSAIDs are prescribed for the patient. Individuals with poor response to acetaminophen are recommended systemic NSAIDs or intra-articular corticosteroid injections (Woo, 2016). The selection of NSAIDs depends on patient preference, duration and cost f treatment, and adverse reactions.
Aspirin and Nonacetylated Salicylates: Pharmacodynamics
- Actions:
- oanti-inflammatory;
- oanalgesic;
- oantiplatelet;
- oantipyretic;
- Pharmacological effects: similar to NSAIDs.
- Body temperature is lowered through:
- othe impact on the hypothalamic thermostat;
- operipheral vessels vasolidation (Woo, 2016).
Due to their ability to lower patients’ body temperature, salicylates increase the heat dissipation. Analgesic and anti-inflammatory activities are resolved though the prostaglandin synthesis inhibition in the way similar to NSAIDs (Woo, 2016). It is necessary to note that aspirin has more potency in inhibiting prostaglandin synthesis than NSAIDS. Also, the anti-inflammatory activity of aspirin in higher than that of NSAIDs. The main reason for such a disparity is thought to be the acetyl group of the aspirin molecule (Woo, 2016). Another effect of aspirin is the irreversible inhibition of platelet aggregation. Bleeding times are prolonged through the use of single analgesic-level doses.
Aspirin and Nonacetylated Salicylates in OA Treatment
- Acetylsalicylic acid (aspirin):
- tablets, chewable tablets, enteric-coated tablets, timed-release tablets, caplets, suppository;
- cautious use in children is recommended;
- toxicity risk is increased at high doses;
- the combination with extended-release dipyridamole is more favorable than aspirin alone;
- Diflunisal:
- tablets (250/500 mg);
- recommended dose: 1 g initially, and then 500 mg every 8-12 hours for adults (Woo, 2016).
OA patients may experience acute or subacute painful episodes the major cause of which is inflammation. Whereas there is no effective drug that could change the course of OA, salicylates can be used to treat the pain (Woo, 2016). Aspirin is recommended due to its analgesic effect and anti-inflammatory action. In divided doses (1.2 to 2.4 g daily), this drug is well tolerated. Compared to NSAIDs, aspirin is reported to have fewer side effects (Woo, 2016). Acetaminophen does not have any anti-inflammatory action, but it is helpful for analgesia.
Nursing Implications
- Control over pain.
- Correct intake of drugs.
- No overdose issues.
- Ability to manage one’s condition.
- Avoidance of side effects.
The main nurse-related consequence of OA treatment is the patient’s ability to control his or her life due to the selection of correct drugs and dosage (Woo, 2016). It is necessary to explain the possibility of adverse effects and perform patient education to reach the best outcomes of treatment. Also, the nurse should make sure that the patient is capable of addressing the healthcare facility when he or she notes the deterioration of pain or other uncommon indications. Overall, the nurse’s role in the pharmacological management of OA is to promote patients’ well-being and help them to avoid complications.
References
Ashkavand, Z., Malekinejad, H., & Vishwanath, B. S. (2013). The pathophysiology of osteoarthritis. Journal of Pharmacy Research, 7(1), 132-138.
Woo, T. M. (2016). Drugs used in treating inflammatory processes. In T. M. Woo & M. V. Robinson (Eds.), Pharmacotherapeutics for advanced practice nurse prescribers (4th ed.) (pp. 801-836). Philadelphia, PA: F. A. Davis Company.