Implementation Plan
In the past three years, scientists have shown a high interest in preventing pressure ulcers among patients with limited mobility. (1) Most researchers share the opinion that an organized approach to risk assessment and the use of the Braden scale significantly improves patient health indicators and reduces the risk of developing pressure ulcers. (2) The Braden scale was chosen because it meets the project objectives and is the most widely used, convenient, and effective tool for assessing the risks of developing pressure ulcers. In particular, using the Braden scale for patient assessment and nursing education is in line with the research goal to raise awareness among nurses about risk assessment.
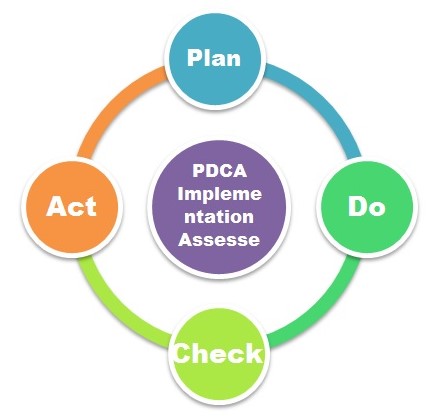
PDCS Quality Improvement Method
For an ongoing evaluation of the implementation plan, the project team will use the PDCS tool:
Establishing the Braden Scale Implementation Task Force Committee
Establishing the Braden scale implementation Task Force Committee will occur after the first collective meeting with the nurses, who decided to participate in the project in the middle of April 2021. The Committee will consist of Nurses Managers, ICU, Medical and Surgical Units, Chronic Care Units, IT, and the Quality assurance department. Each member will have their role and responsibilities, and the project team observers will evaluate their efficiency. Based on these observations, Unit Pressure Ulcer champions will be chosen who will have extended duties determined by the role of the unit they represent.
The project team will hold a meeting for health workers who have agreed to participate in the project, during which the researchers will talk about the need and objectives of the project and present an action plan. During the meeting, the project team members will express their views on the following issues:
- Start date of the project start.
- Outreach to participants, including nurses, patients, and researchers.
- Place of storage of documents related to the project, including educational materials and test results at the end of training; storage space for other related materials, including color-coding.
- The procedure for coordinating the implementation of the use of color-coding with the hospital management.
- Start date of educational training.
- Duration of pieces of training, including the duration of one lesson and the entire session.
The members of the project team proposed to hold a meeting in mid-April 2021. All patients with reduced mobility who are being treated in the hospital will participate in the project. After training and the introduction of color marking, nurses will be able to improve the effectiveness of preventing pressure ulcers. The members of the project team will create a check-list of the project participants. Other related documents will be made available to nursing staff during and after the end of the project. A green educational information booklet on the use of the Braden scale will be made available to all healthcare providers and will be electronically stored.
Stakeholders, including the participating nurses and hospital management, can subsequently discuss additional educational training sessions and decide whether to maintain the color-coding procedure. The study results will be assessed according to the effectiveness of risk mitigation. Nursing knowledge will be assessed according to testing. Project team members plan to achieve a higher average nursing awareness score on working with the Braden scale.
The project team will oversee the nurses during testing and carry out a risk assessment in the early stages. The educational materials will provide a roadmap for the effective use of the Braden scale. Combining the implementation of the color-coding process and educational training with final testing will improve the effectiveness of preventing pressure ulcers among patients with limited mobility. The project sustainability will be ensured by the subsequent decision to introduce the practice of color marking and repeated training sessions. At the stage of developing the project implementation plan, a work schedule was drawn up.
Action Plan
The action plan will include a list of steps, presented in Table 1, in the form of a check-list. Notably, it will feature creating the implementation plan, reviewing it with the staff and supervisors in clinical areas, revising the plan according to the feedback, and explaining how the measurable outcomes will be evaluated.
Table 1
Interventions: Implementing the Braden scale
The implementation of the project will feature several interventions. First, the project members will ensure the Braden scale implementation by integrating it into Electronic Medical Record EMR. It will be done after the discussion with the Committee and its approval. Notably, the Braden scale will feature an alert icon on the main screen of medical equipment in patient rooms with reduced mobility. The color-coding will reflect the severity of the risk of pressure ulcer development. Red will stand for severe or high risk, orange – for moderate risk, yellow – for mild risk, and green for no risk. The nurses will put the color-code stickers on patients’ doors as a reminder. Then, the Guideline will be developed named Using Braden Scale for Predicting Pressure Ulcer Risk in Adults. The project team will also create a Braden Scale Interventions Algorithm (BSIA) and hold the staff education and training campaigns promoting the Braden scale assessment tool.
Staff Education and Training Campaigns
The project team will run the Train the Trainer Program after selecting one nurse from each unit as a pressure ulcer champion. The champions will be trained on how to link the subscale to the practice. The Nursing Orientation Program will be held during the first joint meeting of the Committee. The program will inform the research participants about the policies, procedures, and documentation standards associated with integrating the Braden scale tool in everyday nursing practice. The program will encourage creative use of existing resources to ensure effective risk reduction of pressure ulcers and create an environment that meets the ever-changing demands of quality healthcare.
The unit staff will present the information about their roles, responsibilities, and activity areas within the Nursing Orientation Program. In the training sessions, an interactive workshop on using the Braden scale in the clinical area will be conducted. The project team will develop the scenario and teach the nurses to apply the Braden scale, calculate the score, and identify the risk category. The team will use effective teaching strategies, such as lectures, high-fidelity simulation, concept mapping, case studies, debating, and problem-based learning.
The project implementation will be based on training the medical staff to correct the level of risk to patients under the Guidelines on the Braden scale application. A team of nurses will be involved in implementing the plan, who will sign an agreement to participate in the study and attend educational training sessions. Patients who will be attended by nurses will be aware that they are research participants. This approach to project implementation will ensure that ethical considerations are met. The study will involve patients with limited mobility and different risk levels of developing pressure ulcers – from low to high levels of risk. A broad sample of patients will provide an appropriate stratification level and ensure the originality of the study.
During the training sessions, nurses will become familiar with educational materials on risk assessment and the Braden scale application. Upon completing the training, they will answer a series of questions from the test, based on which researchers can evaluate the training effectiveness. The educational materials will be refined so that the material is easy to remember and as simple as possible, but at the same time does not lose sight of important details. Some important information will be taken from the Braden scale Guidelines.
The study will produce an educational Green Booklet that nurses can carry with them to check whether patients have symptoms and health indicators that indicate a higher risk. One of the project’s main goals is to increase the personal attention of nurses to patient health indicators. According to research, the Braden scale is effective only when nurses conduct an in-depth and detailed assessment of the patient’s condition and is significantly reduced with a formalized approach. (3) However, to make it easier for nurses, researchers are proposing color-coded labels to signal the risk level.
A Nursing tip will be sent through the hospital announcement from the education department to all nurses. There will be several tips revealing the topics selected from the Guideline on the Braden scale, such as the Braden scale subscale, when to complete the initial Braden scale assessment, and when to perform the reassessment. A presentation with the title “Braden Scale from Theory to Practice, Bridging the Gaps” will be developed. The Braden scale ID cards will then be created to guide the nurses in assessing the patients for pressure ulcer risk. The cards will be printed and distributed to all nurses, who will carry them along with their staff ID Card. A competency list for the nurses performing the Braden scale assessments will be developed to determine the key related competencies. A Pressure Ulcer Awareness Day will be established, the information disseminated will promote the early prediction of high-risk patients using the Braden scale.
Evaluation
The evaluation will be performed using pre- and post-training test questionnaires. Another evaluation aspect will be the documentation audit on EMR; the documentation audit tool will be developed. Field audit will be performed through evaluation of the color-code stickers’ compliance with the patients’ condition. The passing of competency will be evaluated after the completion of the training. The research will probably face some obstacles, including proactive barriers like refusal by nurses or hospital management to cooperate, nurses’ inattention to teaching materials, or technical problems. The team will establish a TFC to engage the participants, develop bright and handy teaching materials, and work in cooperation with the IT unit to overcome any technical problems.
References
Al Mutairi, K. B., & Hendrie, D. (2018). Global incidence and prevalence of pressure injuries in public hospitals: a systematic review. Wound Medicine, 22, 23-31.
Charalambous, C., Koulori, A., Vasilopoulos, A., & Roupa, Z. (2018). Evaluation of the validity and reliability of the Waterlow pressure ulcer risk assessment scale. Medical Archives, 72(2), 141.
Moore, Z. E., & Patton, D. (2019). Risk assessment tools for the prevention of pressure ulcers. Cochrane Database of Systematic Reviews, (1).