Introduction
This educational project paper aims to reduce cases of rehospitalization at the facility after discharge. The project focuses on a for-profit nursing facility where rehospitalization is common. The project is useful because rehospitalization has raised many concerns to government agencies and is a part of healthcare reforms.
The literature review shows that there are avoidable and unavoidable cases of rehospitalization. However, there are also various factors, which influence available literature, such as different methodologies, purposes, geography, and interpretation of results. Therefore, policymakers find it difficult to harmonize such data for formulating policies.
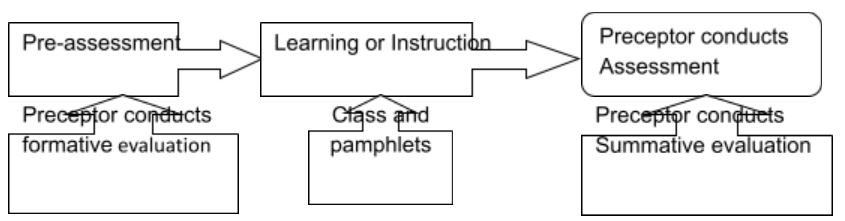
The project used pretest and posttest to conduct the project among the target group (nurses). The preceptor implemented the project in four stages. He used test scores to evaluate the effectiveness of the project.
Description of the setting
The nursing and rehab center is a for-profit agency located in Roswell, Georgia. The agency is a part of other nursing homes in different states. The agency has 220 beds with 33 bed ventilators. The occupancy rate at the facility is 68 percent with 181 residents.
It is a skilled nursing facility (SNF) but not a special focus facility. It provides most of its services on-site to residents. However, the agency offers few services offsite. It has both short-term and long-term care services to residents. It participates in both Medicare and Medicaid programs. The role of the preceptor includes providing services on-site and offsite to patients.
Purpose of the educational project
There are several cases of rehospitalization of patients after discharge from nearby hospitals and nursing homes. Rehospitalization takes place because of many different factors, such as Medicare and Medicaid services provided, availability of post-acute care provided by SNF and on-site and offsite rehabilitation services offered.
Rehospitalization has effects on patients. For instance, Medicare policymakers expressed their interests to change the system by not paying for preventable cases of readmissions. Among the elderly, rehospitalisations can results into decline in functional abilities and cause disabilities. This implies that senior patients must seek long-term care after rehospitalization (Berkowitz et al., 2011).
The purpose of this project is to design education project plan that can enhance patients’ care and assist caregivers to realize effective transitions of patients as a fundamental part of their roles.
Design of the educational project
- The topic of the educational project is reducing rehospitalization in the agency from other nearby facilities.
- Presentation of the project shall be through pamphlets. The pamphlet shall have the following:
- What is rehospitalization or hospital readmission?
- Causes of hospital readmission
- Effects of hospital readmission
- How to reduce rehospitalization
- Evaluation of effectiveness of interventions
There shall also be class lectures to facilitate understanding of pamphlet contents.
- The target group for the educational project consists of nurses. However, the project focuses on nurses who are responsible for patients’ discharge processes.
- The student shall ensure effective planning and implementation of the project by ensuring active participation in all stages. The preceptor must ensure that nurses or students attend classes and get copies of pamphlets.
Method for evaluating effectiveness of the project: pre-test and post-test
The method of pretest and posttest is often the most suitable method of assessing the effectiveness or the extent to which an educational intervention has influenced students. The test provides details of how the intervention shall achieve its results. However, we have to consider what we call ‘improved outcomes’ from interventions.
The preceptor shall administer the tests at the entry and exit points of the education project.
The tests shall reflect the situation at the facility and causes of rehospitalization from other nearby nursing homes. Therefore, we can determine positive changes at the facility. The pretest shall enable the preceptor to understand current knowledge on rehospitalization at the agency and offer basis for comparison on posttest outcomes. The preceptor shall also be able to evaluate whether the rehospitalization prerequisites are achievable.
Pretest (true or false)
- It is possible to reduce cases of rehospitalization after 30 days of patients’ discharge
- Rehospitalization is preventable
- Rehospitalization has negative impacts on patients and healthcare providers
- We should observe discharge disposition and reassess patients’ data before discharge
Posttest (true or false)
- Rehospitalization is preventable
- There are many risk factors correlating to future hospital readmission
- Care providers have ultimate roles in minimizing cases of hospital readmission
Evidence Based Literature Review for Project
Hospital readmission has become a part of the healthcare national reforms. According to Mor and fellow researchers (2010), the cost rehospitalization was $4.34 billion in 2006. The study indicated that most of the patients discharged from other healthcare facilities got readmission into SNF within 30 days after their discharge. Most of these patients were Medicare beneficiaries. As a result, the Medicare policymakers decided to withdraw payments for preventable cases of rehospitalization, which involve pneumonia and heart failure. This change took place in October 2012. The team also promised to review other medical conditions within two years.
This point may explain why the agency, which has both Medicare and Medicaid programs receive many cases of rehospitalization from nearby nursing homes. However, rehospitalization is not uniform in the country, but varies from state to state.
Berkowitz and other researchers observed that patients who got rehospitalization to skilled nursing facilities (SNF) had high rates of “early and unplanned rehospitalization” (Berkowitz et al., 2011). However, they also pointed out that hospital readmission had several risk factors, such as “recent hospitalization, specific diagnoses (such as congestive heart failure), acute medical illnesses, depression, and other factors” (Berkowitz et al., 2011). At the same time, senior patients also experienced adverse effects due to rehospitalization. For instance, such patients experienced steady reduction in their functional abilities. These situations ended in disabilities. Consequently, such patients become give up their independence for long-term care at healthcare facilities.
Some researchers have classified rehospitalization into two categories, which include avoidable and unavoidable cases (Sedehi, 2011). The timing of rehospitalization is usually readmission within 30 days after discharge. Readmission may occur due to a lack of follow-up care after discharge. Cases of avoidable rehospitalization usually result from medical errors, severe events, or because of appropriate social support. We also have avoidable cases in terms of “clinical, demographics, and operational factors” (Sedehi, 2011).
Operational factors are avoidable. They include consequences that result from discharging patients during the weekend and wrong places of admission. Such patients had long lengths of hospital stays and were likely to be under emergency rehospitalization.
Kudtarkar identified general trends observed in rehospitalization of patients to both SNF and other rehabilitation centers.
Table 1: Source: (Kudtarkar, 2009)
Kudtarkar noted that most cases of rehospitalization were mainly from patients. In addition, the author noted that there were also other illnesses associated with rehospitalization.
Past studies have also reviewed challenges to effective understanding rehospitalization processes (Kudtarkar, 2009). Such studies have cited lack of sufficient data as an impediment to understanding rehospitalization. At the same time, there were also cases of poor coordination among various healthcare providers in their efforts to reduce cases of rehospitalization.
Vest and other researchers noted that the existing studies on preventable cases of rehospitalization in the US contained evidence from “a variety of patient populations, geographical locations, healthcare settings, study designs, clinical and theoretical perspectives, and conditions” (Vest, et al., 2010). However, policymakers find it difficult to use this literature because of the definition differences, gaps, and different methodological and study designs. Therefore, it is only appropriate for healthcare providers to conduct multiple and thorough studies across different healthcare facilities in order to identify causes of such variations.
Based on negative consequences of rehospitalization, scholars have proposed various interventions in order to reduce such cases of rehospitalization (Berkowitz et al., 2011). They argue that healthcare providers should have proper documentation systems and effective discharge planning. Patients also expressed their concerns with the inadequacy of discharge processes. However, documentation processes are not effective in reducing cases of rehospitalization. Consequently, some researchers have developed a comprehensive intervention plan to address cases of rehospitalization (Berkowitz et al., 2011). Such a plan addresses admission issues, care provisions, the aim of care, provisions of social services, medication reconciliation, and frequencies of the patient’s rehospitalization within six months after discharge. The intervention also assesses whether the patient would prefer rehospitalization while in SNF.
Other researchers have proposed a two-tier model to address cases of rehospitalization (Sedehi, 2011). In this case, the care provider identifies a high-risk patient and refers the patient to an educator in order to enhance discharge processes and ensure adherence after the discharge. Still, some researchers have also shown that effective follow-ups after discharge resulted into few cases of rehospitalization. On this note, others have proposed the use of volunteers in order to “enhance the quality of healthcare provisions, satisfaction, and develop effective health-social partnership for transitional care” (Sedehi, 2011).
Rehospitalization has become common and a major source of healthcare concern. The concerns mainly occur due to preventable cases, costs, and increasing rates of avoidable rehospitalization. From the cost perspective, many healthcare facilities shall experience challenges due to increased cases of avoidable rehospitalization and the government’s action to alter such payments (Hansen et al., 2011). The program is under the quality improvement initiatives. In order to challenges from rehospitalization, healthcare providers must formulate potential strategies of reducing rehospitalization. This implies that it is necessary to identify best practices and policies, which can facilitate reduction of avoidable cases of rehospitalization. This shall “improve quality, reduce unnecessary health care utilization and costs, promote patient-centered care, and increase overall value in the system” (Sedehi, 2011).
It is important to note that effective reduction of risks associated with rehospitalization needs identification of risk factors and patient populations associated with rehospitalization. Further, we can identify risk factors, which we can reduce by educating patients or by involving them in the intervention. On this regard, care providers should engage patients in pre-discharge education and counseling. Moreover, healthcare facilities should address the issue of potential cases of rehospitalization and avoidable cases of readmission. It is also necessary to have effective home-based support services, constant follow-ups, and targeted post-discharge follow-ups. Healthcare providers should aim at preventable cases of rehospitalization during discharge processes and ensure effective transition.
Implementation and Evaluation of Effectiveness
Specific details of project implementation
Stage one
The preceptor reviewed goals of the education project and determined whether they were realistic and measurable. The implementation involved class lectures accompanied with pamphlets. The aim of the project was to evaluate education outcome on reducing rehospitalization in the facility.
Stage two
The preceptor determined the progress of the education based on the goals of the project. This process ensured strict adherence to project requirements.
Stage three
The preceptor used goals and measures in the second stage in order to identify effective interventions.
Stage four
The preceptor must reinforce interventions with positive outcomes. In addition, he must revise or eliminate interventions without impacts on learners.
Results of the participants on short-term expected outcomes
- Students showed increased awareness about rehospitalization
- Students identified various causes and circumstances leading rehospitalization
- Learners noted the importance of care providers in reducing cases of rehospitalization
The preceptor used test scores to evaluate educational project outcomes. The tests were effective in gauging progress the students achieved in reducing rehospitalization education.
Effectives of the project based on short-term outcomes
- Majorities of the target audience showed increased awareness on rehospitalization
- The project was successful because the target audience showed positive results
Determining long-term effectiveness of the project
- The preceptor shall ensure active participation by the target group
- There shall be adequate class lectures and pamphlets on the subjects
- Students shall collect data on the project
- The preceptor shall analyze the collected data
- The project shall commence after the intervention education and completed in assessment stage
- The preceptor and the target group shall initiate any needed changes based on the results
Conclusion
There are several concerns about rehospitalization. As a result, government agencies and policymakers have expressed the need to address rehospitalization. In addition, there are also various factors, which are responsible for rehospitalization. Therefore, the desire is to reduce cases of rehospitalization due to its adverse effects on patients and healthcare systems.
This research shows that initiatives on rehospitalization at schools or learning centers have positive outcomes. Therefore, the project shows that we can explore different strategies in order to enhance awareness about rehospitalization. These may include both discharge and post-discharge processes.
References
Berkowitz, R., Jones, R., Rieder, R., Bryan, M., Schreiber, R., Verney, S., and Paasche- Orlow M. (2011). Improving Disposition Outcomes for Patients in a Geriatric Skilled Nursing Facility. Journal of the American Geriatrics Society, 59(6), 1130- 6.
Hansen, L., Strater, A., Smith, L., Lee, J., Press, R., Ward, N.,…Williams, M. (2011). Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011, 1-7.
Kudtarkar, D. (2009). Discharge planning: Exploring strategies to increase social involvement. Healthcare Environments of the Future, COA 8823-DZ, 1-4.
Mor, V., Intrator, O., Feng, Z., and Grabowski, D. (2010). The Revolving Door of Rehospitalization From Skilled Nursing Facilities. Health Aff (Millwood), 29(1), 57–64.
Sedehi, A. (2011). Addressing the Problem of Hospital Readmissions. Web.
Vest, J., Gamm, L., Oxford, B., Gonzalez, M., and Slawson, K. (2010). Determinants of preventable readmissions in the United States: a systematic review. Implement Sci., 5, 88.