Introduction
Tuberculosis (TB) is considered one of the oldest contagious diseases. As of 2010, World Health Organization estimated that there were 8.8 million of people infected (McCance & Hueter, 2014). The disease has definite clinical manifestations such as “productive cough with or without hemoptysis, fevers, night sweats, and weight loss” (Grosset & Chaisson, 2017, p. 17). The patient from the case study experienced most of the symptoms and was taken to the hospital after one week of observing these symptoms. Complex examination proved the diagnosis of “infiltrative TB of left lung without MBT shedding” (Kozlov, 2016, para. 2).
Case Study
- a 30-year-old male;
- looks older than he is;
- history of intravenous drug abuse;
- history of hepatitis B (Kozlov, 2016).
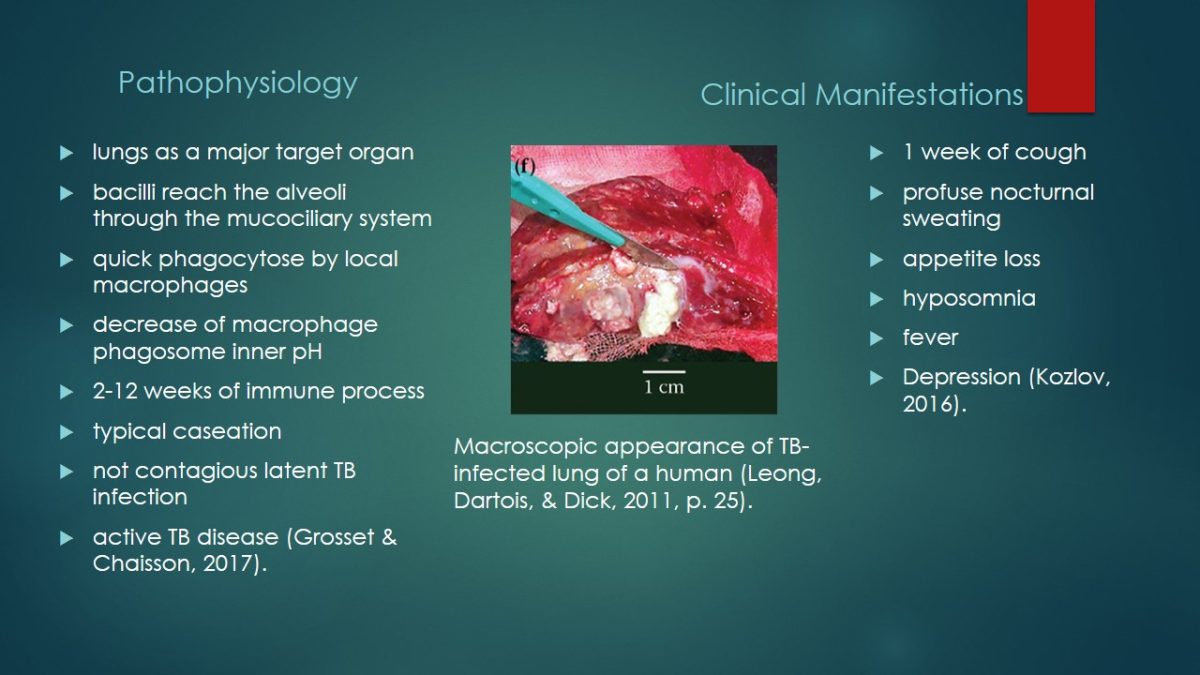
Pathophysiology
- lungs as a major target organ;
- bacilli reach the alveoli through the mucociliary system;
- quick phagocytose by local macrophages;
- decrease of macrophage phagosome inner pH;
- 2-12 weeks of immune process;
- typical caseation;
- not contagious latent TB infection;
- active TB disease (Grosset & Chaisson, 2017).
Clinical Manifestations
- 1 week of cough;
- profuse nocturnal sweating;
- appetite loss;
- hyposomnia;
- fever;
- Depression (Kozlov, 2016).
The patient was admitted to the hospital where he was examined by a physician in an emergency room. Vital signs such as blood pressure and respiratory rate were within the normal limits. However, the temperature and heart rate were higher, 38.0°C and 110 breaths per minute (Kozlov, 2016). The patient looked depressed. Check of the respiratory system revealed unilateral (left side) crepitation. The clinical manifestations suggested high probability of TB.
Diagnostic Studies
- examination;
- radiology (chest x-ray);
- sputum smear gram stain;
- blood test.
Clinical Management and Treatment Modalities
- for 8 weeks, every day:
- isoniazid;
- rifampin;
- pyrazinamide;
- ethambutol;
- 24 weeks, every day:
- Isoniazid;
- rifampin.
The laboratory studies revealed 1.8 creatinine, WBC: 9.48 x 109/L, and Hgb: 11.4 g/dL (114 g/L). HIV test is negative. Radiological investigation revealed infiltrate in the middle of left lung. It was 1.7 cm in diameter and showed signs of cavitation (Kozlov, 2016). Microbiological investigation did not show growth of blood culture. Mycobacteria growth indicator tube is also negative. Sputum smear showed 4+ squamous epithelial cells, 1+ segmented neutrophils, but no organisms (Kozlov, 2016).
The initial treatment consisted of two stages, the first one lasted for 8 weeks with 8 prescribed antibiotics, and the second one was supposed to last 24 weeks with two prescribed medications.

Evaluation of Treatments
- repeated visit to hospital after two months of therapy;
- worsened symptoms;
- repeat chest radiograph.
Patient Education and Safety
- patient-centered care;
- development of prevention strategies;
- Introduction of evidence-based practice;
- work with risk groups;
- spread of information on symptoms.
The treatment was not efficient and the patient returned to the hospital after two months complaining about coughing up blood. Also, he had been still experiencing malaise, night sweating, and weight loss. Another chest x-ray discovered “progressive bilateral fibronodular disease with a “miliary” pattern” (Kozlov, 2016). The medications for the following 20 months included levofloxacin, cycloserine, kanamycin, pyrazinamide and prothionamide.
Patient education and safety interventions are based on the objectives of Quality and Safety Education for Nurses and include patient-centered care, preventive strategies aimed first of all at the representatives of risk groups, etc. Apart from smoking, drug and alcohol abuse, risk factors for TB are HIV and AIDS. Also, malnourishment, diabetes, some types of cancer, and kidney disease contribute to getting TB. In addition, prevention of TB includes limiting contacts with infected people.
References
Grosset, J., & Chaisson, R. (2017). Handbook of tuberculosis. Cham, Switzerland: Springer International Publishing.
Kozlov, R. (2016). Case studies: Tuberculosis. Web.
Leong, F., Dartois, V., & Dick, T. (2011). A color atlas of comparative pathology of pulmonary tuberculosis. Boca Raton, FL: CRC Press.
McCance, K.L., & Hueter, S.E. (2014). Pathophysiology: The biologic basis for disease in adults and children (7th ed.). St. Louis, MO: Elsevier.