Acute respiratory failure (ARF) refers to a condition where there is severe annihilation of gas transfer at the alveolar, and this condition becomes characterized by hypercapnia (>50 mmHg) and hypoxia (<50 mmHg) in a patient who had healthy lungs formerly (Weinberger, 2008). The typical value for pulse oximeter saturation (SpO2) is 94- 98%, while arterial partial pressure of oxygen (PaO2) is 9.3-13.3 or kPa (80-100 mmHg). Further, pH is 7.35- 7.45 and arterial carbon dioxide (PaCO2) is 4.7 and kPa (35-45 mmHg) (McCurdy, 2012). Common conditions triggered by failure of ventilation include acidosis and hypercapnia.
ARF does not have a standardized definition in critical care. However, the most prevalent criteria for clinical and epidemiologic examinations include diagnosis of Acute Lung Injury (ALI) as well as Acute Respiratory Distress Syndrome (ARDS). Other criteria include some level of oxygen malfunction, employment of variable intervals of ventilator support and the respiratory factor of the Sequential Organ Failure Assessment (SOFA) score (Weinberger, 2008). ALI is the early stage of ARDS. Other ailments related with ARF include pneumonia, acute exacerbation of COPD and status asthmaticus.
ARF occurs once the fibrotic and exudative regions of the lung overlap. Subsequent to the first acute endothelial and epithelial injury, deposition of fibrin, alveolar oedema and haemorrhage occur in the lung together with disseminate interstitial inflammatory cell infiltrate (Weinberger, 2008). While hyaline membranes line the alveolar spaces, increasingly, alveolar consolidation happens.
In ARDS, the compliance of the lung obtains first reduction through alveolar oedema and disintegration, and second, by pulmonary fibrosis. While a low compliance is not commonly incorporated as a diagnostic measure of ARDS, it is an even feature of the ailment and necessitates accurate assessment to optimize support through mechanical ventilation (McCurdy, 2012). The following equations demonstrate calculations for respiratory compliance and lung compliance, respectively.
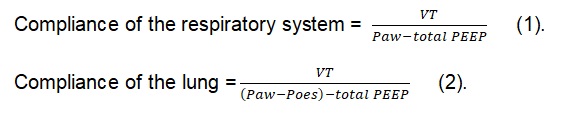
In the equation, Poes and Paw represent the pressures obtained in a 2- s inspiratory suspension at the esophagus and airway respectively. Besides, total PEEP is the summation of both intrinsic and applied positive end-expiratory pressure. VT represents tidal volume. Thus, aspects that must be incorporated into the evaluation of respiratory compliance, in patients with ARDS include assessment of auto-PEEP and intra-thoracic pressure together with measurement of plateau pressure at different lung volumes (Weinberger, 2008).
Management and Treatment
ARF can be managed through invasive, noninvasive and respiratory rescue therapy techniques. Invasive mechanical ventilation enhances gas circulation and protects the airway in severely ill patients. Initially, positive pressure ventilators, which pressured gas into endotracheal tubes, obtained common use in treating patients with acute respiratory failure. Ventilators became further refined to allow patients to prompt breaths so that they harmonized with the breathing patterns of individual patients, for comfort and efficiency. The last 15 years have experienced development of enhanced ventilators, which provides enhanced delivery of air to patients. Besides, development of methods to wean patients from invasive ventilation more safely and swiftly have helped eliminate avoidable complications and reduced expenses in intensive care units. Further, use of noninvasive ventilation has enhanced results.
Noninvasive ventilation is a significant evolution in the treatment of ARF. Noninvasive ventilation lessens injuries in the airway and the threat of pneumonia, which arises because bacteria may move into the lungs via the endotracheal tube (Bolton & Bleetman, 2008). However, noninvasive ventilation should only be used for patients with heart failure of chronic obstructive pulmonary disease. Heart failure causes inadequate pumping of blood, making fluid go back to the lungs and impede circulation of oxygenation. Usually, noninvasive ventilation has the potential of maintaining the client pending removal of the excess fluid.
Some respiratory rescue therapies include prone positioning and high frequency oscillatory ventilation. Prone positioning can enhance oxygenation in patients with ARF. Some techniques of prone positioning include enhancement of ventilation, perfusion circulation and recruitment of atelectasis. Prone positioning alleviates hydrostatic pressure of superimposing lung parenchyma and the constrictive effect of the heart on lungs.
Equally, high frequency oscillatory ventilation enhances gas exchange through an elevated mean airway pressure and reduced tidal volume compared to normal minute volume, thus allowing lung protective ventilation.
ARF treatment involves pharmacological adjuvant therapies, which include neuromuscular blocking agents and corticosteroid treatment. Managing high levels of intracerebral pressure, reducing oxygen consumption, allowing invasive MV, and treating muscle spasms are some of the roles of neuromuscular blocking agents (Bream-Rouwenhorst, Beltz, Ross, &Moores, 2008). This application is relevant when other methods fail.
On the other hand, corticosteroids obtain use in several physiological mechanisms. Insufficiency of corticosteroid can result in severe illness although critical illness can as well trigger relative insufficiency (Bream-Rouwenhorst et al., 2008). Corticosteroids obtain most use in conditions that cause ARFs such as severe asthma and acute chronic obstructive pulmonary diseases, due to their anti-inflammatory effect.
Prolonged use of corticosteroids causes risks associated with an increased vulnerability to infection. Similarly, extended use of NMBAs can cause severe polyneuropathy, weakness and myopathy in mechanically ventilated patients and those with septic illness. Prolonged use of both corticosteroids and NMBAs causes the risk of muscle weakness.
New treatments of ARFT include use of surfactants, extracorporeal techniques of gas exchange and new mechanical ventilation. Lung surfactants can be used for replacement therapy in treatment of ALI, especially when the alleged cause is aspiration pneumonia (Weinberger, 2008). However, this method is still under investigation.
There are also new ways of mechanical ventilation. The traditional way of ventilating ALI patients’ provides hefty tidal volumes, reduces the fraction of inspired oxygen and maintains standard amounts of arterial oxygen as well as carbon dioxide. Considerable changes to this custom have obtained consideration based on the traumatic impacts of mechanical ventilation on lungs.
Lastly, extracorporeal techniques of gas exchange are new to clinical practice. The idea underlying the utilization of this technique in patients with ARF is to offer an interim alternative for transpulmonary respiration as the damaged lungs recuperate.
Planning for Care
Care for ARF can be obtained from home or hospital. Chronic alveolar hypoventilation can be enhanced by long-term mechanical ventilation in the course of impulsive breathing. Long-term mechanical ventilation reduces hospitalization need, enhances quality of life, besides survival (Bream-Rouwenhorst et al., 2008.
At the same time, acute and severe respiratory failure requires medical intervention. Levels of oxygen require swift normalization through providing additional oxygen. Patients experiencing high levels of carbon dioxide l require breathing support. Such patients obtain pressurized gas from gadgets that augment pressure when prompted by a timer or the patient’s breathing efforts. This gas may be supplied through invasive ventilation, whereby a plastic tube gets slotted into the trachea, or through noninvasive ventilation, whereby a mask gets fastened over the mouth and nose. Certain patients may require noninvasive ventilation just at nighttime. Noninvasive ventilation allows an enhanced quality of sleep because the patient’s fatigue becomes alleviated. Hence, the plan to take care of a patient from home or hospital should be based on the needs of the patient. If a patient’s situation calls for hospitalization, that is what should follow.
Assessment and Evaluation
Most patients with ARF end up in the Intensive Care Unit (ICU). Since ICU may have an impact on quality of life, an assessment on long-term quality of life (QOL) is vital. The Euro-QOL-5D (EQ-5D) and the Short Form 36-item questionnaire (SF-36) can be used to access QOL for patients with ARF (Fitzgerald, 2010). SF-36 evaluates 8 aspects including physical pain, task limitations because of physical difficulties, social functioning, bodily functioning, task restrictions owing to emotional issues, mental wellbeing, health views as well as fatigue. Conversely, EQ-5D evaluated 5 aspects including self-care, mobility, normal activities, depression, physical pain and vision.
Prevention and Interventions
Common principles of clinical practice are essential for the deterrence of ALI. Some of these principles include quick fixation of fissures, sufficient volume recovery of hypovolaemic states, timely drainage of abscesses, grafting of burnt marks and proper use of antibiotics.
Education should be offered to clients who seem to be at risk of acquiring ailments related to ARF. For instance, clients who are smokers should be enlightened on the dangers of smoking. Patients who exhibit symptoms of ARF should be taught how to manage the disease. Patients also require education upon receiving treatment and medications, in order to know how to manage the disease.
References
Bolton, R. & Bleetman, A.(2008). Non-invasive ventilation and continuous positive pressure ventilation in emergency departments: Where are we now? Emergency Medical Journal, 25(4), 190-1944.
Bream-Rouwenhorst, H.R., Beltz, E.A., Ross, M.B., Moores, K.G.(2008). Recent developments in the management of acute respiratory distress syndrome in adults. American Journal of Health System Pharmacy, 65 (1), 29-36.
Fitzgerald, R.C. (2010). Pre-invasive disease pathogenesis and clinical management. New York, NY: Springer.
McCurdy, B. (2012). Noninvasive positive pressure ventilation for acute respiratory failure patients with chronic obstructive pulmonary disease (COPD): An evidence-based analysis. Ontario Health Technology Assessment Series, 12 (8), 1–102.
Weinberger, S. (2008). Principles of pulmonary medicine. London, England: Sage.