Introduction
Radiation Dosimetry program
For anyone who wishes to join the program, the requisite qualifications include a full time working experience of not less than three years in a radiation oncology clinic as radiation therapist. One is required to be a recent graduate from the respective school of radiation therapy (Berger, Hajek, Bilski, Körner, Vanhavere, & Reitz, 2012). The dosimetry personnel training program is driven by four goals. The goals are designed to enable a radiation oncology professional to fulfill the mission statement that directs a dosimetrist to impart the requisite skills and necessary knowledge to any graduating student to develop competent skills and to gain the independence required to work as qualified dosimetrist.
According to Bevelacqua (2016), the first goal is to impact knowledge on the treatment of patients based on advanced as well as basic skills, comprehend the treatment protocol parameters, develop clear understanding of calculations based on emergency simulation-and-treatment cases, and have clear understanding of the record-and-verify systems. The second goal is about enabling graduating students to demonstrate evidence of problem solving and critical thinking skills in different situations (Mettler Jr, Huda, Yoshizumi, & Mahesh, 2008).
In addition, the student is required to develop enough skills to assess the treatment plan and make recommendations whether to use a specific treatment technique. Besides, the student should develop the right skills to determine the appropriate special treatment procedure and the necessary setup to achieve the objectives (Bevelacqua, 2016). This leads to the third goal, which outlines the need to inculcate effective communication and reporting skills on patients undergoing treatment among graduating students and radiation oncology team members. The fourth goal is to ensure that those students who graduate have the requisite knowledge and ability to maintain confidentiality of information about a patient who is undergoing treatment.
Film-screen combinations are used to achieve diagnostic radiology to ensure that patients are protected effectively when undergoing treatment. In this case, medical facilities are sealed and unsealed according to the prescribed procedures and standards for therapeutic purposes. The procedure is executed according to recommended radiation dose levels that place the patient and the user/ Radiation Safety Officers (RSOs) outside the risk of getting radiation induced damages. Often, small treatment procedures are directed by skilled RSO and knowledgeable physicist. According to Devic (2011), the radiation protection programs were initiated to fulfill certain objectives within the recommended doses.
The objectives include prevention of radiation induced deterministic and stochastic effects and accumulation of societal benefits that exceed the overall costs. According to Bevelacqua (2016), staff preparation is required to fulfill effective personal monitoring, establish detailed dose requirements, monitor the limits of exposure to the public and the patient’s family, and establish direct measurement of radioactivity (bioassays). Patient exposure to radiation is drastically reduced by pulsed progressive scanning of the image using a program that is integrated with a good quality camera as opposed to previous methods that make is difficulty to lower fluoroscopic radiation to acceptable doses.
Literature Review
Occupancy Dosimetry
Also known as ‘simply dosimetry’ or occupancy dosimetry, the phrase is defined as “the process of taking measurements that are either accurate or estimated values of radiation doses irradiated on individuals” (Berger et al., 2012). According to Devic (2011), the key word, occupancy dosimetry involves “determining by use of a dosimeter or though extrapolation the quantities that are imparted on a target organ, which have radiological relevance constituting of exposure, kerma, fluence, and dose equivalent measured on a dosimeter” (p.11), which cause the absorbed dose. The absorbed dose is the measurable quantity of dosimetrist radiation protection that provides measurements which yield numerically expressed data on the basis of previously defined relationships. This leads to another key definition known as the equivalent dose, which is attributed to the type of radiation and accompanying energy incident and detectable on the body.
Here, literature by Devic (2011) notes that equivalent dose is defined as “the absorbed dose averaged over a tissue or organ and weighted for the radiation quality that is of interest” (Hobbs, Song, Huso, Sundel, & Sgouros, 2012). The severity of radiation, which is also known as ‘radiation weighting factor’ can be determined by the biological effects it has on human tissues. On the other hand, effective dose is defined as “the weighted equivalent doses in all the tissues and organs of the body” (Berger et al., 2012). In the context of the definition, a dosimeter is used to make specific or average readings of the amount of dose absorbed from the ionizing radiation that is often linear or non-linear. Dosimeter measurements depend on the medium of interest that is often modeled in terms of the cavity theory.
Cavity is the sensitive volume of measurement that is calibrated with the indices used to evaluate the level of compliance to the recommended dose. The measurements can either be stochastic or non-stochastic and results certified as compliant must show an index of either equal or less than unity. Here, exposure to ionizing radiation has been proved to have adverse health effects on the irradiated person’s tissue cells. In all cases, the safety system should include safety standards as detailed in the “American National Standard Radiation Safety for Personnel Security Screening Systems Using X ray or Gamma Radiation” (Martin & Sutton, 2015). It is recommended that when working in a radiation emitting environment, personnel should wear a dosimeter at the collar as recommended in the regulations guiding the use of dosimeters.
Stochastic Characteristics
An evaluation of the behaviour of living cells irradiated with stochastic energy shows that such sources lack specific dose thresholds. Martin and Sutton (2015) note that the effects of the dose are directly proportional to the irradiating intensity, which leads to the manifestation of events that usually reveal themselves before the latent period elapses. Suzuki and Yamashita (2012) note that cell modifications in response to the level of intensity of incident radiation occur when the latent period has elapsed. According to Martin and Sutton (2015), the deterministic effects are evaluated on specific and measurable thresholds of definite levels of radiation doses.
However, a study of people that have been exposed to the ionizing radiation has revealed that effects of the dose are proportional to the received dose with a low probability of occurrence. Despite that, changes in the cells can lead to cancer due to radiation doses from gamma rays and neutrons. Stochastic hereditary disorders can be transmitted to the offspring increasing the probability of developing multifactorial diseases. Often, irradiated body cells are likely to lead to biological DNA damages with doses that are in the range of 100 mGy (Martin & Sutton, 2015). However, it is difficult to measure radiation doses that are as low as µGy and any treatment using radiation sources is based on linear extrapolation.
Induced Hereditary Effects
An analysis of the discourse by Bevelacqua (2016) concludes that induced hereditary effects often referred to as progeny are secondary and do not cause new types of mutations but are direct causes of increased levels of naturally occurring mutations. This new types of gene mutations include neural tube defects, Down’s syndrome. The preference rates are 0.2% per Sv (Sievert) for the general population and 0.1% Sv for the working population.
It is imperative to note that exposure levels that exceed one hundred mSv have proved to be fatal to the exposed person (Bevelacqua, 2016). However, different models have been used to estimate the risk levels, with one such model based on the shape of the dose-response curve. In this curve, a monotonic linear pattern emerges, which is the most preferred method that is used to make prudent choices on the patient dose exposure rates (Martin & Sutton, 2015). However, most countries in Europe recommend the use of the International Commission for Radiation Protection (ICRP) system of radiation protection that provides guidelines on the use of sources of radiation on human beings (Berger et al., 2012). ICRP operates on the principle of justification, where each radiation source is kept to the minimum. The other principles are based on dose limitation and optimization.
The major element of occupational dosimetry monitory
Dose quantities
Certain exposure situations are deemed to be exceptional. However, stringent conditions of dose limits apply for those who are exposed to different levels of incident radiation. Dose conversion factors can be calculated using the MIRD Phantom technique to determine the right dose for subjecting a patient to the frontal half-space exposure (Berger et al., 2012). Absorbed doses are determined on a gray scale equivalent to one unit of energy deposited per unit measure. The level of biological effectiveness is measured on the radiation weighting factor (wR) (Devic, 2011).
The cumulative effects of background radiation are direct causes of radiation that can be determined by radiological physics who deal with the study of the level of exposure, effects, and protection of individuals against the risk of exposure to different levels background radiation. Berger et al. (2012) note that certain enforceable safety standards apply. Conditional acceptance of the risk of exposure to distinct and varying sources of radiation limits the patient’s health benefits. Radiation exposures are characteristically modeled on stochastic or deterministic outcomes. Measurements using both approaches yields deep dose equivalents based on maximally exposed or occupational dosimetry data. This is in accordance with the requirement that radiation is an already proved excellent tool for therapeutic and diagnostic medicine. According to Berger et al. (2012), in each case, when exposed, both healthy and sick tissue cells morbidity relation reveals different responses and levels of sensitivity.
Protection of Staff
Different researchers including Bevelacqua (2009) agree that the level and nature of occupational hazard exposures provide appropriate indicators for guidelines in designing facilities and in putting in place appropriate equipment operating procedures using patient care personnel correctly trained in a medical environment. Appropriate facility design with the right technical details that assure the patient and occupational safety personnel of safe exposure at a reasonable cost must be guaranteed (Vano, Ubeda, Miranda, Leyton, Durán, & Nader, 2011). Typically, accurate and effective design parameters include the level of sophistication, centralized vs. decentralized equipment, level of medical care, size and sophistication of the facility, and the level of safety that is engineered into the facility. For effective occupational protection, appropriate local shielding should be used and incorporation of specific procedures for the protection of the vulnerable.
It is imperative to make visual checks of the area where the equipment is situated and evaluate the resulting safety against established standards. Frequent monitoring and assessment of nuclear or radiation sources is a prerequisite to effective monitoring. Besides, accurate inventory of radioactive isotopes is mandatory to comply with regulations and ensure that unanticipated or other types of losses do not happen. Besides, accidental disposal of needles and syringes is recommended for better protection and avoidance of accidental injuries.
Personnel monitoring
It is appropriate to conduct internal and external routine monitoring of staff to ensure that radiation levels are within the regulatory limits. According to Bevelacqua (2009), this ensures that the facility is secure so that any loopholes are detected and sealed rightly as well as establish those likely to get higher exposures to radiation. It is appropriate to conduct bioassay, which is a radiological analysis that is designed for the examination of the whole body in a radiation detection system. The rationale is to establish the level of radiation activity in the body. Exposure to bioassay depends on mode of entry, radiation emissions, and characteristic bio-distribution in vivo.
Nurses
The professionals trained in caring for patients subjected to therapeutic degrees of radionuclides are assigned to nurses or radiation oncology specialists. The nurses are taken through a training program to prepare them on how to effectively carry out therapeutic treatments on patients. Typically, Devic (2011) notes that the nurse serves the important aspect of ensuring that the patient’s mental status is evaluated and determined ahead of treatment. Besides, the nurse takes the responsibility of injecting the patient with diagnostic doses of radiopharmaceuticals as prescribed by the doctor.
Radiation safety committee
A standing radiation committee should be established in a medical-radiation facility, which should be constituted by a nurse, RSO, and a representative from the facility’s management. Bevelacqua (2009) and Devic (2011) among other authors clarify that the committee must have experienced members with background knowledge on the utilization of radioactive materials. It is imperative to include expertise in radiation oncology, nuclear medicine, and biological scientists. Regular meetings form an important component of the radiation safety committee.
Management committee
The radiation safety programs must be constituted to provide oversight on quality assurance (Devic, 2011). Resource allocations that adequately meet the needs and participation of members who are required to fulfill the requisite activities of the management committee should be included. Specific policies and procedures that comply with the dose-limiting standards envisaged in recommendations provided by requite bodies, codes of regulations, and laws that are defined as proactive policy for effective maintenance of personal exposures. According to Martin and Sutton (2015), additional requirements recommended for the transportation of brachytherapy and radiopharmaceuticals include the use of sealed containers. The ALARA principles provide the key guidelines to conform to in the transportation and handling of radioactive materials.
External and Internal Dosimetry
Operational quantities are used to measure both external and internal exposures to specific radiation doses (Bevelacqua, 2016). Operational, physical, and protection quantities can be measured. It is difficulty to accurately measure the effective dose, equivalent dose, and basic protection quantities.
External dosimetry
Bevelacqua (2016) notes that external dosimetry is due to the emission of radiation from external sources such as beta or neutrons and gamma rays that are made incident on the body, eye lens, and the skin. It worth noting that beta particles do not make deep penetrations into dead skin, but alpha particles have lethal effects on the living skin and other organs of the body when radioactive sources are made incident on the living organs. Empirical evidence by Bevelacqua (2016) among other researchers, suggest that beta particles provide deeper penetrations of up to 0.3 cm into the body and make a penetration of 1 cm in some cases of the body tissues. Photons and neutrons are the predominant primary sources of radiation. Devic (2011) clarifies that external dose measurements should be made by subjecting every part of the body to radiation except extremities such as the elbow, legs below knees, and arms below the elbows as illustrated in figure 1.
The specific parts where the measurements are taken are shown in figure 2.
Typically, Bevelacqua (2016) notes that measurements of the dose and the eye are taken at a depth of 0.3 cm while the shallow skin measurements are made at a depth of 0.007 cm. Deep dose measurements of the body are taken at a depth of 1 cm as illustrated in figure 2.
On the other hand, because the exposure of the entire body to the source of radiation is not uniform, it is appropriate to determine the Effective Dose Equivalent (EDE) using a dosimeter that is placed at the back and in front of the body by applying the (EPRI Method). The results are weighted using the formula: EDE = ¾ Hi + ¼ Lo (Mettler Jr. et al., 2008).
Internal dosimetry
This is a two phased approach consisting of estimating the level and potency of nuclear radiation inside the body and calculating the resulting internal radiation doses (Devic, 2011). In-vivo bioassay involves making internal measurements using external instruments that depend on gamma radiation, which has sufficient energy to move within the detectable range outside the body. The three types of detectors used to measure the level of radiation include the whole-body counters, lung counters, and the thyroid counters. Both direct and indirect measurements have been applied to determine the amount of radiation in wounds and body organs.
The measurements yield monitoring data that is analyzed to show the intensity of internal and internal doses which results from the chemical characteristics of the radioactive substance in use (Mettler Jr. et al., 2008). Data from the measurements taken by exposing intakes and the excreted radioactive substance are specified using appropriate quantities of radionuclides and the quantity of materials used. Here, it is also “important to use computational models that show how biokinetics of radioactive materials work in the body” (Hobb et al., 2012). The effective dose with specific radionuclides should be determined as well as the effects on organs of the body measured appropriately.
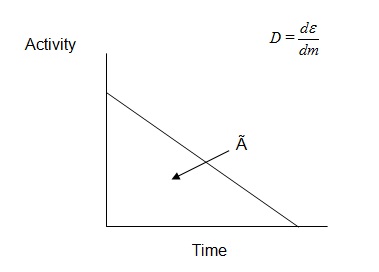
Activity Internal dose calculations can be obtained by defining the dose equivalent or absorbed dose (D), which is expressed as:
In the expression, dm is the mass that is ionized with incident radiation, which is expressed in gray (Gy) units.
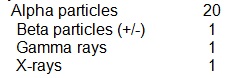
The ICRU Reports of 39 and 43 describe the quantity or dose equivalents that are expressed as H in a mathematical relation, which shows that H=Q.D exposures. In the mathematical relation, D is the quantity factor while Q is the dose that has been absorbed, which occurs in the form of linear energy transfer. The International Commission on Radiological Protection has recommended qualifying factors about the effectiveness of incident radiation as shown in table 2.
Table 2. Quality Factors Recommended in ICRP 30.
Empirical evidence has shown the importance of determining the quantity of energy absorbed per unit mass by each tissue when body organs are exposed to beta particles and electrons. The “particles are either penetrating or non-penetrating radiations” (Mettler Jr. et al., 2008). Typically, the resulting equation for the absorbed dose is expressed as:
In the above case, n=number of radiations having energy E, A =activity, D=absorbed
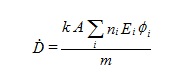
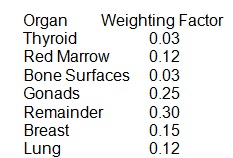
D=absorbed, E-energy per radiation, m=mass of target region, and k=constant of proportionality. A critical review of how to determine certain quantities of radiation shows that the area under the activity curve can be determined by the use of the quantity cumulated activity (Ã) (Bevelacqua, 2009). Certain organs of the body subjected to radiation doses, which is also known as the effective dose equivalent have different body organs assigned different weighting factors as shown in table 3.
Table 3.
Regulations that Control the Occupational Dose
Occupational dose is defined as the dose received by an individual working in a licensed environment, but excludes individuals who receive medically administered doses. Berger et al. (2012) note that several regulations have been developed to ensure that those exposed to incident radiation or those working in irradiated environments are subjected to limited and acceptable levels of doses. For instance, different authors including Bevelacqua (2016) recommend that those in the public are subjected to dose equivalents of 0.1 rem per year or (1 mSv) in a year as envisaged in section under section “35.75 of the regulations guiding voluntary participation in medical research” (McParland, 2010). Here, doses that exceed 0.1 rem of exposure per year are classified as lethal. Bevelacqua (2016) notes further that as per section 35.75, the 0.002 rem (0.02) millisievert dose limits are recommended for dose exposures to unrestricted areas that come from external sources.
According to Devic (2011), the regulations that define dose exposures, section A.1.9 deals with the units of exposure and dose measurements from external and internal sources of radiation as shown on table 1.
Table 1.
The regulation, A.2.1 on the implementation of various requirements on the protection of individuals exposed to radiation, each facility must be registered in accordance with provisions of part A, which details the protection factors and allowable radiation doses (Bevelacqua, 2009). Typically, this covers combination respirators, breathing Apparatus (SCBA), and air-line respirators. In each category, there are sub-categories which provide details of the assigned protection factors to comply with.
According to Berger et al. (2012), section A.1.10 deals with the Units of Activity while section A.1.11 deals with Deliberate Misconduct. The section details how certificate holders of registration and licensed employees as well as contractors and subcontractors could be dealt with in law when identified to engage in deliberate misconduct (Bevelacqua, 2009). Typically, a “person who violates A.1.11 (a) (1) or (a) (2) may be subject to enforcement action in accordance with the procedures in A.7”. Violations occur in terms of procedures and breach of requirements. A.2.2 radiation protection programs discuss about appropriate protection and enforcement of regulations that guide the application and level and appropriate implementation of section A.2.2 (b) that constitute the ALARA requirements. That is in addition to section A.2.11, which regulates the emission of radioactive materials to the environment.
Pursuant to section A 2.3 of the occupational dose limits for adults, prescribed limits are defined to enable the parties (adults) under external exposure to radiation to control the dose limits allowable per year. The effective dose limits that have been suggested by Stabin and Flux (2007) based on empirically tested evidence include 0.05 Sv as pertains to external body organs. However, Bevelacqua (2009) affirms that a dose equivalent of 0.5 Sv for the eye and ear exposed to external radiation have been recommended according to sub-section A.2.8 of section A.2.3 of the occupational dose limits for adults.
On the other hand, Devic (2011) asserts that the recommended dose in extreme circumstances is 0.15 Sv, which is described as the lens-dose equivalent. Bevelacqua (2016) presents empirical evidence which shows that the recommended dose for shallow-dose equivalent is 0.5 Sv as “pertains to the level of exposure of the whole body and skin in extreme irradiation situations” (McParland, 2010). Section A.2.3 (b) of section A 2.3 of occupational dose limits for adults define excesses of recommended dose limits in the event of the occurrence of accidents, emergencies, and special exposures (Bevelacqua, 2009). Part c of section A.2.3 (b) of part 1 recommends that the deep dose equivalents, shallow, and lens dose equivalents have to be established to determine occupational dose limits for situations where individual monitoring is not possible.
On the other hand, regulation A.2.4 defines the extent and level of exposure of radiation of an individual to external and internal doses of radiation. According to Bevelacqua (2016), the dose equivalents for the skin and the eye lens are subject to different limits. Within the limits are prescribed the amount of radiation limits for intake by inhalation of the radionuclides for each irradiated organ or tissue. Besides, section A. 2.4 constitutes the intake by oral ingestion radionuclides that are greater than 10 percent. On the other hand, A.2.4 (d) stipulates the dose requirements irradiated on wounds or absorbed through the skin. On the other hand, A.2.5 defines the external dose limits for external exposure (McParland, 2010). On the other hand, A.2.6 defines the limits for internal exposure. Here, Suzuki and Yamashita (2012) note that compliance levels can be determined pursuant to A.3.3 that makes suitable measurements of the level of concentration of radioactive materials from the air. It is worth noting that adherence to the regulations that guide the handling of radioactive materials for medicinal purposes provide significant benefits to the patient.
How to keep dose records
Record keeping is an important requirement that is detailed in the National Dose Registry (NDR) for doses that qualify to be known as ‘dose of record’ as detailed in section 10 CFR 835 of specific records maintenance requirements for different conditions of exposure (Martin & Sutton, 2015). Record keeping is usually undertaken through a radiological recording program. The key characteristics of the program include keeping records that are audible as well taking the recording process through the stages of “stages of creation, distribution, use, arrangement, storage, retrieval, media conversion (if applicable), and disposition” (Suzuki & Yamashita, 2012). In each case, specific radiological policies and procedures should be adhered to. Besides, various elements of the radiological recordkeeping components have been pointed out that make part of the record keeping procedures and policies.
According to McParland (2010), the policies and procedures cover both external and internal dosimetry exposures besides including documents saved in databases. In addition, the records should indicate personnel training as well as ‘As Low As Reasonably Achievable’ records (Martin & Sutton, 2015). Different dose levels and requirement are provided as guidelines on the amount of dose to record. For instance, if the incident dose on the skin that is in direct contamination with the skin is 2% or less than the specified value by the Radiation Control Department (RCD), there is no need to record such a dose. Suzuki and Yamashita (2012) recommend that the reports and records with private information as well as magnetic records should be kept under key and lock. Privacy and confidentiality are kept according to section 712-05 on information storage and retrieval act.
As per the legal requirements, it is appropriate to ensure that record keeping standards are observed. In this case, legibility and accuracy define the desirable attributes of the records. Suzuki and Yamashita (2012) note that record attributes are defined by the name of the facility, function, process, specific location, identification code, date, time, and supervisory signatures. In addition, it is important to ensure all items related to radiological records such as opaque substances and non-standardized items.
Personnel Radiological Records define the recording and storage of planned and special exposures and other forms of exposures as detailed in 10 CFR 835.402 legal requirements (Martin & Sutton, 2015). The dose records should be written in such a way that the person or interested party is accurately identified for whom the record is kept. It is imperative to keep records on the effective dose from external sources, dose limits for the eye, nose, and other body parts such as embryo/fetus, equivalent dose for the skin, and records for anomalous dose results. It is imperative to include individual records for the whole year for external and internal exposures (Martin & Sutton, 2015). It is also “important to ensure complete recording of radiological incidents involving the public and personnel” (Martin & Sutton, 2015). That is besides keeping records of radiological safety of employees and pregnancy information. The other records that should be kept include computerization of records using optical disks among other components.
Personal information on dose levels is detailed in the Radiation Protection Regulations, Canada. Besides, those records generated and maintained fall into the categories of workplace monitoring and control, administrative, and individual monitoring. Besides, paragraph 27(a) of the NSC Act requires those responsible for using radiation emitting equipment for the purpose of treatment or in circumstances that allow a person to pay a visit to an irradiated background to keep records as pertains to the level of exposure. According to McParland (2010), the Radiation Protection Regulations as defined in section 2 of the NSC Act under Section 24 which belongs to the category of the regulations that protect employees and outsiders from different doses of exposure to radiation, requires that records should be kept in compliance with the regulations.
At the individual monitoring and dose records level, 10 CFR 835.702(a) and (b) on monitoring and maintenance of records submitted by individuals as per section 10 CFR of 835.402 details persons exposed to excessive doses that are above the acceptable dose limits, doses that are irradiated on individuals because of special circumstances such as emergency exposures and planned special exposures as well as those individuals whose exposures are planned but not within the jurisdiction of the 10 CFR 835.402 regulation (Devic, 2011). Here, it is imperative to note that records should be kept under the requirements to ensure individual monitoring to for compliance purposes. This is to ensure that occupational dose limits are not exceeded, but are kept within the limits in compliance with section 10 CFR 835.702(c) (2).
Each individual record is defined by appropriate details, which consists of the full name of the individual exposed to irradiation doses incident on the body from internal or external sources, details such as the social security number of the person whose record is being kept, date of birth, and gender. The employment status of the person should be added to the record, occupation code, and the type of building where the person works constitutes the details appended to the records.
Summary
The discourse on ‘Radiation Dosimetry Program’ reveals a number of facts such as the requirements or one needs to meet to join the dosimetry program and become a radiotherapist. Among the requirements is that one needs and experience of more than two years of work at a radiation oncology clinic with an undergraduate level of education to become a radiotherapist. It is also appropriate to have extensive knowledge and skills that enable one to make appropriate assessments of the treatment requirements for a patient besides being able to make the correct treatment procedures and protocol parameters. The key areas of understanding include the ability to determine the level and intensity of radiation one should be subjected to either from direct or background sources of radiation. It has been revealed in the study that exposure to ionizing radiation is adverse to the living cells of the body. However, the level of exposure is limited to 0.1% Sv for the general population, but exposures up to one hundred mSv are fatal for the body organs. The program provides details of appropriate doses, program components such as Nurses and radiation safety committee among others. Both external and internal dosimetry has been discussed and appropriate quantities and the regulations that provide guidelines to adhere to detailed.
References
Berger, T., Hajek, M., Bilski, P., Körner, C., Vanhavere, F., & Reitz, G. (2012). Cosmic radiation exposure of biological test systems during the EXPOSE-E mission. Astrobiology, 12(5), 387-392.
Bevelacqua, J. J. (2016). Health Physics: Radiation-Generating Devices, Characteristics, and Hazards. New York: John Wiley & Sons.
Bevelacqua, J. J. (2009). Contemporary Health Physics: Problems and Solutions. New York: John Wiley & Sons.
Devic, S. (2011). Radiochromic film dosimetry: past, present, and future. Physica medica, 27(3), 122-134.
Hobbs, R. F., Song, H., Huso, D. L., Sundel, M. H., & Sgouros, G. (2012). A nephron-based model of the kidneys for macro-to-micro α-particle dosimetry. Physics in medicine and biology, 57(13), 4403.
Martin, C. J., & Sutton, D. G. (Eds.). (2015). Practical radiation protection in healthcare. Oxford: Oxford University Press, USA.
McParland, B. J. (2010). Nuclear medicine radiation dosimetry: advanced theoretical principles. New York: Springer Science & Business Media.
Mettler Jr, F. A., Huda, W., Yoshizumi, T. T., & Mahesh, M. (2008). Effective doses in radiology and diagnostic nuclear medicine: a catalog 1. Radiology, 248(1), 254-263.
Suzuki, K., & Yamashita, S. (2012). Low-dose radiation exposure and carcinogenesis. Japanese journal of clinical oncology, 42(7), 563-568.
Vano, E., Ubeda, C., Miranda, P., Leyton, F., Durán, A., & Nader, A. (2011). Radiation protection in pediatric interventional cardiology: An IAEA PILOT program in Latin America. Health physics, 101(3), 233-237.