Introduction
Radiation comes from natural sources and man-made sources. Included in the natural sources are those that come from outer space (especially the sun), the rocks and soil, and the human body (Natural Radiation, par. 2). Man-made sources include medical equipment, consumer products, nuclear weapons and industrial infrastructures (pars. 7 -10). Radiation has a harmful effect upon the human body.
However, since it is useful in medicine and industry, its use must be controlled so that human exposure will be minimized. New modalities and uses are being introduced using radiation.
Radiations are classified as alpha, beta and gamma radiations. An alpha radiation emanates from “heavier elements” (with atomic number higher than 52) and becomes ionized easily that prevents penetrating a material (Types of Radiation, par. 4). It cannot penetrate and cannot harm the skin (4).
This emission can only travel for a short distance in the air (What Types, par. 2). The particle is a helium nucleus (2) with a positive charge (Types of Radiation, par. 4). The Beta radiation can have a positive charge (positron) or negative charge (negatron), lighter, moves fast, and has a higher penetrating capacity (5). Although it can penetrate water, inner layer of the skin, and other materials, an aluminum metal can stop it (5).
A gamma radiation is electromagnetic in nature just like the ultraviolet rays (6). It has a short wavelength, high penetration capacity (even into the tissue) and a danger to people (6). The X-ray is grouped together with gamma radiation (Radiation Protection, 6).
Figure I
Frequency and Wavelength Spectrum
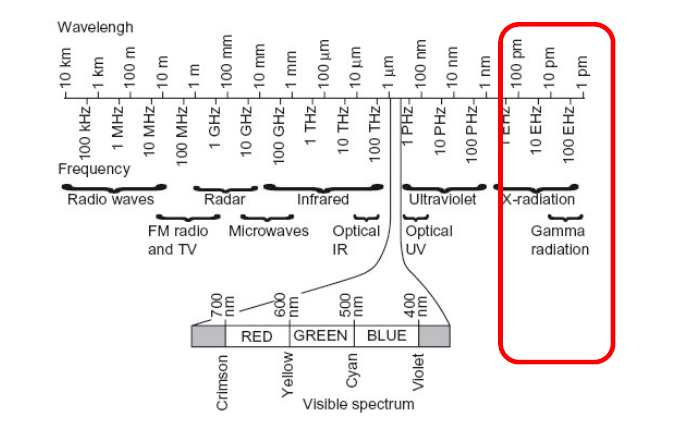
(Source: Radiation Protection, 6).
Although nuclear medicine has benefits to health, there are accompanying risks that may result to serious consequences or death (Occupational Radiation, xxii). Exposure to radiation is a risk to cancer. Therefore, people working with them should wear protective gears or at lesser time.
How is Radiation Measured
The international unit of measurement under the metric system uses the System Internationale (SI) (Radiation Measurement, 1). The SI unit for emitted radiation is “Bq” (becquerel) while the conventional unit (used in the US) is “Ci” (currie) (1). The radiation absorbed by the body and deposited in the tissue uses the conventional unit “rad” (radiation absorbed dose) and SI unit “gray” (Gy) (1).
The absorbed dose refers to the energy taken for every unit of weight of tissue (1). Gy is generally used at present than rad (1 Gy is equivalent to 100 rad) (1). However, when measuring the biological risk due to exposure, the conventional unit “rem” or SI unit “sievert” (Sv) is used (1).
The biological risk is calculated based on an assigned number (depends on capacity to transfer energy to cells) for the ionizing radiations (e.g. alpha, beta, gamma, x-ray); referred to as Quality Factor or “Q” (2). To get the risk in rem, the dose in rad is multiplied with Q (rad x Q) (2). One Sv is equivalent to 100 rem (2).
Measurements below “1” and those measured by thousands have been assigned prefixes.
Figure II
Prefixes for Measurements below 1
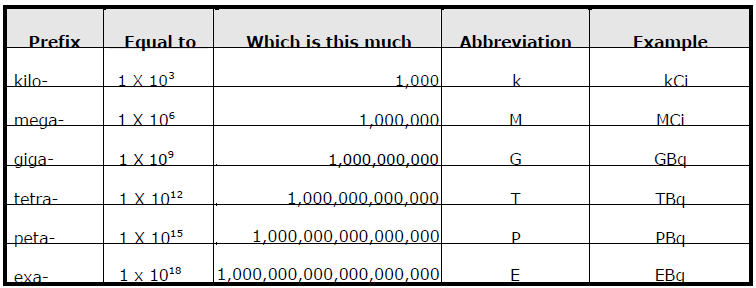
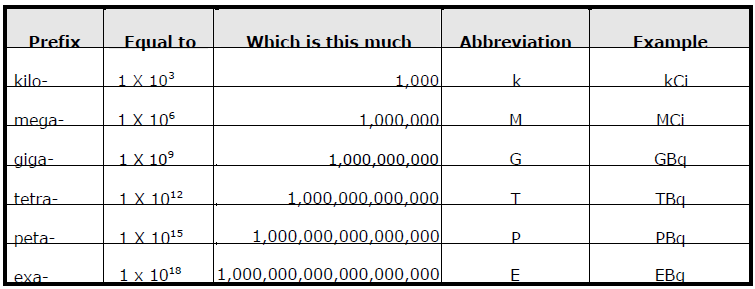
Figure II provides the prefixes for measurements below one while Figure III shows the measurements made in thousands.
Figure III
Prefixes for Measurements by the Thousands
Radiation and Radioisotopes in Medicine
Radiation has found usefulness in medicine. The branch of medicine that uses radiation either for diagnosis or treatment is nuclear medicine (Boyd, par. 1). Products from radioactive materials whether used for diagnosis or therapy are called radiopharmaceuticals (Radioisotopes, par. 14).
With the use of radiation, organs inside the body and the bones can be imaged quickly and accurately (1). In this manner, the physician can make a diagnosis of one’s illness by viewing the disorder or malfunctioning (1). Radiation is also utilized in the treatment of organs and abnormal cell growth (1). Radiation therapy is used in leukemia treatment (What is Ionizing, par. 8).
The three general categories of radiation use in nuclear medicine are: radiation therapy, diagnostic radiology and fluoroscopically guided interventional procedures (Jensen, pars. 5-7). In radiation therapy, the dosage of radiation given is very high but care is given so that danger to nearby healthy tissues is minimized (5).
Diagnostic radiology detects fractures and lung conditions (6). X-ray, the primary modality used in this approach, is carcinogenic (6). Fluoroscopically guided interventional procedures give higher doses than diagnostic modalities (7). The procedures angioplasty and stent replacement allow the doctor to see the movement of internal organs with the use of X-ray energy (7).
Radiation diagnosis is made possible with the use of radioisotope (2). Isotopes are two atoms of an element “with the same atomic number (same number or protons in the nucleus) and position in the periodic table and nearly identical chemical behavior but with different atomic masses and physical properties” (Radioisotopes, par. 1). Each element was found to have one or more isotopes (par. 1). An isotope can be stable or unstable, both are used in nuclear medicine (par. 6).
A stable isotope does not go through radioactive decay (par. 6). The protons and electrons in the nuclei of a stable isotope of two or more forms of a chemical element has the same number but different neutrons (par. 7). Carbon-13, nitrogen-15, oxygen-18, and the noble gas isotopes are the stable elements utilized in medicine (par. 9).
The number of protons is responsible for the attribution of atomic number while the atomic mass is the total of the neutrons and protons (Radioisotopes, par. 10). Thus, isotopes that have the same atomic number may have different masses due to the variation in the number of neutrons (par. 10).
A radioisotope (or radioactive isotope), which is unstable, is one produced artificially (Radioisotopes, par. 11). Of the two hundred radioisotopes being used, majority of them are artificially manufactured (par. 12). Radioisotopes are produced by increasing the number of neutrons in the nucleus through neutron activation inside the nuclear reactor or increasing the number of protons in the nucleus inside the cyclotron (par. 13).
A radioisotope may become stable when an alpha or beta particle is emitted and during such process, the electromagnetic radiation gamma rays are released (par. 14). Technetium-99 is the most commonly used radioisotope in the diagnosis of diseases in thousands of hospitals around the world (Boyd, par. 2).
Ionization and Ionizing Radiation
A non-ionizing radiation (e.g. sound wave, visible light, microwave) is one whose energy can make atoms vibrate but not enough to knock-off an electron (Radiation Protection, 6). On the contrary, an ionizing radiation is powerful to remove an electron from an atom, and such property makes it useful for diagnosis, imaging, destroying of abnormal cells and in manufacturing (6). Ionizing radiation can destroy DNA and healthy cells, amplify the risk to cancer, and can cause death at high doses (What is Ionizing, par. 8).
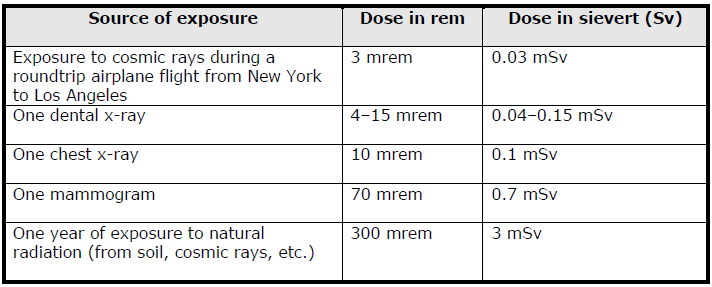
An example of ionizing radiation is X-ray (Radiation Protection, 7). Overexposure to X-ray is dangerous to humans. The usual dose for a chest X-ray is around 10 mrem (7). It can pass through a thick substance (8). An X-ray released by the X-ray machine is controlled by cone in order to concentrate its beam only to the targeted area (8). Ionizing radiation is used in X-ray imaging and CT (Computed X-ray tomography) scan (What is Ionizing, par. 8).
Exposure to Radiation and Protection
The patients who undergo diagnosis and treatment utilizing nuclear medicine are exposed to radiation. However, in the hospital setting, radiation is released under a controlled environment. Radiation exposure in the US from CT scan and nuclear medicine, embodied in the 2009 report of the US National Council on Radiation Protection & Measurements, is 36 percent as against exposure from medical sources and 75 percent as against overall radiation exposure (Boyd, par. 5).
The annual exposure from medical sources, said the report, has increased from 3.6 mSv to 6.2 mSv yearly starting 1980, while that from industrial sources (nuclear plants included) falls below 0.1 percent of the total public exposure (par. 5).
Figure IV
Source of Exposure and Dose in Rem/SV
Since X-ray influences around 30 to 50 percent of medical decisions, the Physics of Radiation and Radiobiology (2000 edition) mentioned that doctors subject 300 million of their patients to such procedure in one year (Jensen, par. 1). As reported in Radiology (1993), in fluoroscopically guided interventional procedures, the hands of physicians receive chronic irradiation for administering high-dose radiation (par. 17). Some workers that stay in the room to guide the X-ray also receive some exposure (par. 18).
The average exposure of workers to radiation in industrial and research institutions is tolerable (Occupational Radiation, v). However, certain occupations require continued exposure to radiation, and the workers were not monitored (Occupational Radiation, v). Exposure reduction from man-made sources entails enhanced control, where workers are monitored closely (xi).
The ALARA (that stands for As Low As Reasonably Achievable) is a set of guidelines used to regulate radiation exposure (Jensen, par. 8). The guidelines provide operating exposure to be below than the allowable exposure so that a greater margin for safety can be had in case of failure or accident (par. 9).
The dose exposure should subscribe to the limits set by the International Commission on Radiological Protection (Occupational Radiation, xi). A development of risk management program will give more protection to workers, and this includes public education which should begin at the school level (xi).
A “safety culture” must be developed by the organization and the individual worker (xiv). Protection can be implemented through continued tracking and recording of exposures, as well as the methodologies used in dose monitoring (xix). Electronic readout dosimeters are being used in a number of countries to track radiation in an organization.
There is also the chromosome aberration analysis tool, available in few countries, that estimates the dose in case of accidental exposure (xx). Measurement of radiation is also offered by business entities that offer dosimetry services to institutions wherein the workers are exposed to radiation (xxi). These specialized companies are able to offer cost effective services and standardized highly-developed systems and equipment (xxi).
The workers who are engaged in diagnostic and therapeutic functions are the most exposed to ionizing radiations (Occupational Radiation, xxi). In fact, such exposure is an inevitable risk for this group (xxi). However, the trend in developed countries is the declining annual level of doses (xxi). Doses that exceed the 10 mSv to 15 mSv levels seldom occur, and can approximate the ideal objective for maximum protection (xxi).
The three principles that would allow for maximum protection for workers in the health care sector are time, distance and shielding (Jensen, par. 11). When the time the worker is exposed to the source of radiation is lessened and the distance from the same is increased (with proper adjustment of proximity), radiation exposure of the worker is decreased (par. 11).
The shielding material and thickness will depend on the kind of radiation and the dosage applied (par. 11). The legislature has yet to pass laws that mandate the use of shielding materials in diagnostic and therapeutic services (12). But the fluoroscopic setting has already standardized the procedure of using shielding materials even for an annual exposure below 50 mSv (par. 13).
Drapes and aprons fortified with lead-impregnated vinyl protect the worker from off-target radiation (Jensen, par. 14). The worker may also leave the room during the procedure for fixed equipment (par. 14). Protective clothing should be used when operating a mobile C-arm fluoroscopy or portable radiography (par. 14).
A wraparound lead apron should be used to protect the worker’s back when the latter used a longer time with the back towards the patient (par. 15). Leg shields are particularly useful when the legs are positioned adjacent to the X-ray tube (par. 15). Thyroid shield, often ignored, can prevent the onset of cancer (par. 16). In some procedures, particular health workers (e.g. interventional radiologists, pain service physicians, gastro-intestinal physicians) may be absorbing huge radiation dose compared to other health workers (par. 16).
The hand is particularly vulnerable for physicians performing interventional modalities, according to Radiology (September 1999 issue) (par. 21). Although needle holders are used to lessen hand exposure of doctors, complicated procedures cause them to put the hands in the path of the beam (par. 19). Astray radiations are also prevalent in interventional modalities resulting to increased exposure, as reported on a community website for radiologists in 2001 (par. 20).
The Journal of Vascular Surgery (October 2000) mentioned that interventional radiologists more often do not use protective shields for the hands (par. 22). It was suggested that radiation attenuation gloves be used to weaken the effect of radiation when operating fluoroscopic machines (par. 23). Doctors are convinced that these sterile and disposable gloves can protect the worker against stray radiation (pars. 24 – 25).
However, when the glove is placed in front of the beam, it attenuates radiation but increases the quantity of stray radiation that affects the hand (par. 27). When the doctor’s hand is placed in front of the beam, the average dose the hand gets is 120 mSv in a single procedure (par. 29). Basing on the International Commission on Radiological Protection (ICRP) recommendation for allowable yearly dose of 500 mSv for the hand, the doctor operating the guided CT fluoroscopy machine can only perform four procedures in a year (par. 29).
However, if the hand is placed four centimeters from the beam, the exposure drops to 1.5 mSv, Radiology (1996 edition) reported (par. 29). This increases the number of procedures one can perform to 330 in a year (par. 29). The materials used for the gloves are lead and bismuth oxide (which is less toxic) (pars. 31, 35).
Health workers operating X-ray machines should also wear protective clothing (Jensen, par. 42). They should also be sufficiently informed on how to wear them properly for optimum protection (par. 42). They should also receive regular updates through an educational program provided by the institution (par. 42). This program must include the biological dangers using them would bring (par. 43).
Industrial Radiation
Industrial radiation may come from nuclear power plants, facilities that use and handle radioactive materials and industrial radiography. Industrial radiography refers to the use of scanners to view objects. The scanners, installed in airport terminals, emit radiation that penetrates materials and clothing. The viewing machines use a “‘Backscatter’ X-ray that penetrate the clothes, creating an image of a person without clothes (Reynolds, par. 3).
There are nearly 400 scanners installed around the airports in the US (and will increase to a thousand by 2011) which continually subject passengers to this type of X-ray (par. 3). The Food and Drug Administration (FDA) vouch for the safeness of the scanners (par. 1). The FDA claimed that the risk is negligible, wherein 1000 scans in a year are needed to reach the maximum allowable dose (par. 7).
Arizona State University physics professor Peter Rez conducted a study on the machine and reported that dying from cancer caused by the scanners has 1 to 30 million ratio (par. 7). But the University of California-San Francisco scientists claim it as “potentially dangerous because the new, and largely untested, technology concentrates the dose on the skin, increasing cancer risk” (par. 3).
Two pilots’ unions boycotted during the middle part of the last quarter of 2010 the scanning system saying that the Transport Security Administration (TSA) assessed the machine’s safeness of up to 5 percent to 20 percent than what was reported in two independent studies (par. 4).
The pilots express concern over the long-term cumulative effect of passing through body scanning (par. 5). The children are the most vulnerable to this type of X-ray; they are more susceptible to radiations (par. 6). Data has yet to prove the safeness of these scanners (par. 5).
Works Cited
Boyd, Rex. Radioisotopes in Medicine. World Nuclear Association. Australasian Science Magazine. 1999. Web.
Jensen, Lori. Protect Health Care Workers from Excessive Radiation: Know what Type of Shielding Equipment Works Best. 2009. Web.
Natural Radiation: Human Sources. Radiation Sources. Jefferson Lab. Web.
Occupational Radiation Protection: Protecting Workers Against Exposure To Ionizing Radiation. Proceedings of an International Conference, Geneva. International Atomic Energy Agency. 2002. Web.
Radiation Measurement. Radiation Emergencies. Centers for Disease Control and Prevention. Department of Health and Human Services. 2003. Web.
Radiation Protection Guidance For Hospital Staff. Prepared for Stanford Hospital and Clinics, Lucile Packard Children’s Hospital and Veterans Affairs Palo Alto Health Care System. 2010. Web.
Radioisotopes. Nuclear Medicine. Radiochemistry Society. 2003. Web.
Reynolds, Denise. Frequent Fliers: What are the Radiation Risks? Emax Health. 2010. Web.
Types of Radiation. Buzzle. 2010. Web.
What is Ionizing Radiation? Uniformed Services University of the Health Sciences. Armed Forces Radiobiology Research Institute. 2009. Web.
What Types of Radiation Are There? Health Physics Society. 2009. Web.