Introduction
NPs are licensed and certified registered nurses with specialized training. They have different educational backgrounds and obligations from doctors (MDs).
NPs perform diagnostic and inspections, administer drugs, and generally care for patients, in contrast to MDs, who focus primarily on disease diagnosis and prescription of tests and treatments. However, the scope of work for NPs differs from that of registered nurses (RNs). Unlike RNs, NPs are permitted to identify patients, prescribe tests, and administer medication, which brings their duties closer to those of a doctor. NPs are essential to the medical system because of their broad range of operations and the superior patient care provided by their greater education levels. NPs carry out their duties as autonomous professionals and work in critical, outpatient, acute, and long-term care facilities. In the wake of the COVID-19 epidemic, when contagion management and prevention have become a worldwide concern, this subject is highly crucial (Shahrin et al., 2022).
Need for Nurse Practitioners in Healthcare
To ensure that all patients are entitled to thorough, efficient, and inclusive care, hospital administration must consider fresh and creative approaches due to the aging population, scarce funds, and cumulative sophistication and intensity of patients. As highly technical ICU nurses, one way to speak out for the patients is by speaking up for all nurses. The innovative education of ICU nurses to become acute care nurse practitioners (ACNPs) will push the limits of current nursing techniques and healthcare provision in several ways. Nursing has acknowledged that the requirements of patients who are critically ill are not being addressed. NPs have a field of expertise that, when used to its full potential, can satisfy the demands of patients, the healthcare system, and nursing staff (Shahrin et al., 2022).
Nurses in Acute and Intensive Care
The fact that NPs frequently treat patients with central venous catheters despite not typically inserting them is an instance from exercise that relates to the problem of sophisticated abilities. As a result, NPs are knowledgeable about these technologies and may instruct other physicians on properly implanting catheters to avoid bloodstream infections brought by central lines (Snyder et al., 2021). Nurses and allied health experts like physiotherapists are examples of positions ACCPs hold in the health industry. Giving care to individuals who are seriously ill is the focus of ICU management. The ACCP job calls for an extensive understanding of acute care medicine and a variety of specialized abilities, such as enhanced health monitoring, developed organ maintenance, and rescue.
Role of Nurses in Acute and Intensive Care
The ACNP duty evolved in retort to resident status scarcities in the critical care entity, comparable to the transformation of the perinatal NP responsibility in the late 1970s (Snyder et al., 2021). Acute care centers sought alternative approaches to publicize and ensure appropriate patient care as medicinal schooling developed more susceptible to the extended durations needed by apprentices and inhabitants. Nurses with primary care experience were well-matched to gain the extra skills and knowledge required to satisfy the additional wants of these service users.
The transformation started in 1993, with existing nursing bodies such as the American Nurses Association, American Association of Colleges of Nursing, American Association of Critical Care Nurses, and National Board of Nursing attempting to address particular diagnostic practice issues (Snyder et al., 2021). In 1995, the ACNP extent and guidelines were published, as was the first national certification. ACNP’s high-quality skills and knowledge were developed in 2004, including research preconceptions and journal articles to highlight the position’s growth and expansion (Snyder et al., 2021). This progress authenticated the ACNP as a separate domain of progressive nursing exercise.
The function of an ACNP is to deliver advanced nursing services throughout the spectrum of hospital facilities to fulfill the unique physiologic and psychological requirements of persons with complicated acute, severe, and long-term medical illnesses. Patients who are critically ill, acutely unwell, or having a chronic illness flare-up or terminal illness make up the population of acute care practices (Snyder et al., 2021). Any scenario where patients need complicated surveillance and therapy, high-intensity nursing treatment, or effective nursing monitoring within the scope of high-acuity care is where the ACNP practices.
The ACNP responsibilities transformed from the requirement for a specialist to care for patients suffering from vital, critical infections and individuals suffering from a crucial, chronic condition (Snyder et al., 2021). An upsurge in the degree of sickness among hospitalized persons, a decrease in healthcare duration of stay, and adjustments in residency training reportage in the healthcare setting were driving factors in the transformation of the ACNP role.
Role of NPs in Infection and Prevention Control
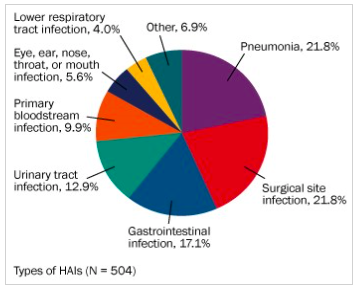
Controlling infections to preserve the general populace and people’s wellness, nurse practitioners collaborate with government organizations, researchers, healthcare professionals, and patients in addition to doctors and medical professionals (Zhang et al., 2020). Infections connected to healthcare happen in the US every year at around 2 million, with a correspondingly high mortality rate of almost 100,000 (Shahrin et al., 2022). The most incredible typical organisms responsible for infections contracted in hospitals are Klebsiella, Staphylococcus aureus (staph), Clostridioides difficile (C. diff), and Escherichia coli (E. coli).
A nurse practitioner’s role as a contagion control nurse involves recognizing and averting the transmission of contagious illnesses, comprising bacterial and viral infections, in a therapeutic set. ICNs are hardworking and aspect-concerned individuals who can successfully share paramount procedures with their coworkers to ensure the well-being of victims being taken care of by an organization (Snyder et al., 2021). When handling both organized contagions and more significant outbursts, their indulgence in the hazards of diverse contagious proxies is crucial. These nurses are constantly on the frontier of cutting-edge medical treatments since they are naturally innovative problem solvers.
The hazard assessments used by nurse practitioners in infection control practices are based on their understanding of the bacteria involved, transmission channels, and the work process in the specialty. The recommendations may change depending on the circumstances and the degree of danger the clinic is ready to accept as a business (Nelson et al., 2019). For instance, in the scenario of an eruption, it may be conceivable to suspend all scheduled surgeries, diagnostics, and examinations, restrict visitation, and completely shut a unit or unit to new patients. A lockdown, however, also has specific unfavorable effects, such as delaying patient assessment and care (Zhang et al.,2020). People who suffer from mental illnesses may experience harmful effects from isolation, which need to be considered.
The nurse practitioner may operate alone based on the size and form of the service; in this instance, they would be required to be sufficiently knowledgeable about and trained in contamination prevention and management to function independently. Clinical advocates, such as physicians or nurses interested in deterring and controlling infections, can also assist by serving as role replicas by exhibiting best practices (Nelson et al., 2019). Additionally, these medical advocates can educate others, offer input on new and established programs, and communicate any issues with the nurse practitioner that may pertain to their line of duty.
Overview of Infection Prevention and Control
Figure 1 shows the percentages of healthcare infections as of 2014 (ECRI, 2015).
Infections in Healthcare
Contaminations related to medical care pose a significant problem for the industry. These infestations are frequently brought on by multidrug-resistant organisms (MDROs), like carbapenem-resistant Enterobacteriaceae (CRE), vancomycin-resistant Enterococci (VRE), and methicillin-resistant Staphylococcus aureus (MRSA) (Ingebretson, 2022). There are two types of infection management techniques, vertical and lateral, intended to stop the transmission of these illnesses. While lateral methods seek to regulate the proliferation of numerous species concurrently, vertical techniques concentrate on one entity.
Risk Factors of Infection in Healthcare
Patients may come into contact with a wide range of exogenous germs from staff members, guests, or other patients while receiving medical care. The clinical setting, the medical staff, the patients themselves, infected drugs, tainted food, and polluted care delivery tools are the most frequent contributors of pathogens that result in HAI (Mudd et al.,2022). The likelihood that a patient may become infected after coming into contact with a hazardous organism varies.
Since they are immune to certain pathogenic virulence factors or can withstand the increased growth of microorganisms, some persons have inherent defense functions and are unlikely to experience signs of illness. Patients are predisposed to HAIs by innate risk variables (Tan et al., 2021). Individuals who are immunosuppressed due to age, fundamental disorders, the intensity of their illnesses, immunosuppressants, or operative or medical procedures have an increased risk of infection. External risk factors involve human interactions, treatment or diagnostic measures, and surgical or other invasive devices. At least 90% of illnesses, based on one study paper, were brought on by intrusive equipment (Mudd et al., 2022).
Four primary methods of conveyance are used to transfer bacteria among patients and medical staff: interface, respiratory secretions, airborne dissemination, and primary vehicle (Phan et al., 2019). Vector-borne transmissions are an unusual route in American hospitals; however, they are other forms of conveyance.
Strategies for Infection Control
An accurate, proof-grounded approach for preventing avoidable pathogens from impairing patients and medical specialists is infection prevention and control (IPC). Efficient IPC obliges continuing deeds from choice makers, facility administration, health workers, as well as patients at all stages of healthcare. There are several strategies for infection control, as shown in figure 2.
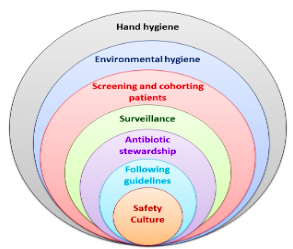
The drawbacks of AST typically outweigh its advantages in non-epidemic conditions. Both opportunity costs and direct costs are included in this. AST could be beneficial in preventing the transmission of pathogens like MRSA and CRE in epidemic conditions (Broussard & Kahwaji, 2022).
The most crucial method of preventing infection is good hand cleanliness. The World Health Organization advises completing hand washing at five different times: before interacting with patients, before undertaking aseptic operations, after coming into touch with bodily excretions, after interacting with patients, and after interacting with their environment (Broussard & Kahwaji, 2022).
The most popular decontamination inhibitor is CHG. CHG baths may only be used in elevated-acuity sections like ICUs, or they could be used throughout the entire hospital (Mudd et al., 2022). Recommendations and washing practices should be developed by institutions and made accessible to healthcare workers.
Antibiotic stewardship programs (ASPs) can assist in lowering drug consumption, Clostridium difficile degrees of infection, and medical expenditures. Through the practical application of operative prophylactic antibiotics, they can assist in avoiding surgical-site contagions.
The risk of cross-pollution must be minimized by assigning ecological maintenance personnel to distinct elements (Tan et al., 2021). Units need to be checked periodically to ensure ambient cleanup procedures are followed.
Standard Practices to Avoid Healthcare-Associated Infections
HAIs place a significant financial strain on the US healthcare system. According to the Centers for Disease Control and Prevention, at least one in 25 medical center patients in the US is battling an HAI (Broussard & Kahwaji, 2022). HAIs can lead to fatalities, permanent physical impairment, an increased charge of healthcare, and more than only additional expenses. However, by taking the actions outlined by the World Health Organization, one can contribute to reducing the spread of contamination in healthcare facilities (Phan et al., 2019).
Challenges in Implementing ACNPs in Healthcare
The stakeholders frequently stem from a misperception of the ACNP’s responsibility. The community, hospital management, and other interdisciplinary team participants must embrace and encourage this novel role. Physician reluctance is one of the most complex challenges since they frequently view ACNPs as competitors instead of collaborative team players.
Although the original cost of setting up an ICU NP program will be high, the total cost is minimal compared to a doctor-only strategy. Increased duration of stay, lower postoperative complications, and lower readmission rates can save costs.
Conclusion
Despite obstacles, it is evident that adding an ACNP to the interdisciplinary team had overwhelmingly favorable results. In the specialist field of emergency care, ACNPs can offer high-quality patient safety. Intensive care certified ACNPs would provide a novel method of caring for critically sick patients in an age of limited funds, rising severity, and increased demand for care.
References
7 strategies to prevent healthcare-associated infections. Global Alliance for Infections in Surgery. (2019). Web.
Broussard, I., & Kahwaji, C. (2022). Universal precautions. National Library of Medicine. Web.
Frieda Paton, M. C. (2021). Becoming a nurse practitioner: Everything you need to know. Nurseslabs. Web.
Ingebretson, E. (2022). Prevention and infection control. In A. Bergeron et al. (Eds.), Principles in nursing practice in the era of COVID-19 (pp. 17-53). Springer, Cham.
Mudd, S., Slater, T., & Curless, M. (2022). Central line-associated bloodstream infections and advanced practice providers: Identifying opportunities for prevention efforts. The Journal for Nurse Practitioners, 18(3), 328-330. Web.
Nelson, L., McMahon, J., Leblanc, N., Braksmajer, A., Crean, H., Smith, K., & Xue, Y. (2019). Advancing the case for nurse practitioner‐based models to accelerate scale‐up of HIV pre‐exposure prophylaxis. Journal of Clinical Nursing, 28(1-2), 351-361. Web.
Overview of infection prevention and control. ECRI. (2015). Web.
Phan, L., Maita, D., Mortiz, D., Bleasdale, S., & Jones, R. (2019). Healthcare workers’ environmental contact and self-contact patterns: Implications for infection prevention and control. Clinical Infectious Diseases, 69(Supplement 3), S178-S184. Web.
Shahrin, L., Parvin, I., Sarmin, M., Abbassi, N., Ackhter, M., Alam, T., Mamun, G., Rahman, A., Shaima, S. N., Shikha, S., Jeorge, D., Nahar, A., Sharifuzzaman, Saha, H., Rahman, A., Shahid, A., Faruque, A., Ahmed, T., & Chisti, M. (2022). In-person training on COVID-19 case management and infection prevention and control: Evaluation of healthcare professionals in Bangladesh. PloS One, 17(10), e0273809. Web.
Snyder, R., White, K., Glowicz, J., Novosad, S., Soda, E., Hsu, S., Kuhar, D., & Cochran, R. (2021). Gaps in infection prevention practices for catheter-associated urinary tract infections and central line-associated bloodstream infections as identified by the Targeted Assessment for Prevention Strategy. American Journal of Infection Control, 49(7), 874-878. Web.
Tan, D., Wiseman, T., Betihavas, V., & Rolls, K. (2021). Patient, provider, and system factors that contribute to healthcare-associated infection and sepsis development in patients after a traumatic injury: An integrative review. Australian Critical Care, 34(3), 269-277.
Zhang, S., Diao, M., Duan, L., Lin, Z., & Chen, D. (2020). The novel coronavirus (SARS-CoV-2) infections in China: Prevention, control and challenges. Intensive Care Medicine, 46(4), 591-593.