XYZ Health Center Overview
About XYZ Health Center
The XYZ Health Center is a private pediatric and family medicine center based in W City. The medical center has remained consistent in the provision of different medical services to a large client base. As a specialized center, this facility has a capacity to service up to 50 patients per day in different departments and sections. XYZ Health Center is a health care agency specializing in Medicaid center-based services and pediatric care.
Founded more than ten years ago, XYZ Health Center provides compassionate care to nearly 300 clients. The Pediatric and Family Medicine office employs 7 thoroughly screened and qualified care-giving staff, making XYZ Health Center one of the largest providers of health care in the W region with specialization in pediatric and family medicine. XYZ Health Center is currently contracted with multiple Pediatric Health authorities.
Objectives and Procedure for Promoting Quality Service Charter
The objectives of XYZ Health Center are:
- To develop and continuously improve services at the center.
- To provide modern, friendly, and effective treatment to the clients.
- To improve the service charter to meet the demand and needs of all stakeholders.
- Continuously review the service charter for relevance and effectiveness for optimal service delivery outcome.
- Review client feedback from environmental, treatment, and cultural perspectives.
The strategies for promoting quality service charter are;
- XYZ Health Center has an up-to-date policy on health and safety.
- The content of the policy is made available to all stakeholders.
- XYZ Health Center has a clear reporting, investigation, and resolution procedures.
- XYZ Health Center has an effective work standard that must be adhered to by all employees.
- The center periodically carries a comprehensive risk assessment and management.
- The plan spells out emergency actions (see figure 1).

Personnel Composition Within the Pediatric and Family Medicine office
The Pediatric and Family Medicine office has seven qualified personnel consisting of two pediatric providers, two family medicine providers, and three medical assistants. The office has adequate employees to handle all business processes. These employees are well trained and adequately experienced to deliver quality and effective services to customers within the stipulated business hours. As captured in Table 1, the employees have different roles.
Table 1: Pediatric and Family Medicine office personnel composition.
Quality in Service Delivery Approach
The services are aligned to quality and consistency for optimal results within a short timeline. As a pediatric and family medicine center, this organization provides services for a wide range of individuals from different cultures and diverse groups, each with their own unique requirements. The services are tailored into service options that respond to the specific needs of clients. Each customer is motivated by the service charter to be part of the comprehensive and individualized program.
The personnel policies and procedures are specific to ABA service provider credentialing, licensing and staff competency, training, orientation, recruitment and selection, performance evaluation monitoring safety, managing clinic risks, termination and follow up, corporate compliance program and plan, documentation guidelines, and health and safety. The center has a state of the art ultra modern training facility that equips personnel with the relevant training needs on risk assessment and response in a timely manner. The center has adequate resources to monitor and manage the needs of clients.
The hospital has a modern center equipped with the necessary resources to offer initial service appointment to a child/family within 14 days of referral data. The 7 dedicated staff and additional contracted practitioners ensure that appointments are honored within a maximum of two weeks.
XYZ Health Center has a manager tasked with connecting the stakeholders and following up on any communication with providers, program agencies, administrators, and other resources that are tailored to benefit clients. The manager also has the responsibility of monitoring all activities and delegating duties at a departmental level. Personnel are hired on a competitive manner with focus on experience in provision specialized services to clients.
The personnel are subjected to continuous training every three weeks in addition to daily assessment on work progress. The training model is designed to accommodate the cultural, professional, and environment needs of personnel and clients. The center’s policy framework is aligned to health safety standards stipulated in the Accreditation Commission for Health Care (ACHC). Management of the center functions on consistency, relevancy, and competency frameworks for optimal outcome. The management plans are reviewed semi-annually and adjustments made whenever appropriate.
The center has a continuous 360-degree performance tracking feedback system that monitors and assesses progress every two months from which adjustments are made. The feedback is subjected to a management review and current policies are adjusted based on the majority vote. In the event of extreme poor result, a new behavioral support plan is put in place. The center also has internal regulations monitoring compliance to compassion, respect, and understanding in the process of providing services to clients. XYZ Health Center has a comprehensive database that can keep and automatically update customer records once the treatment has commenced.
The structure has the capacity to bill insurance that is compatible to the local health system. The system is programmed to electronically capture data and collect ability to pay and excess assets amounts. Also, the system is capable of submitting Medicaid spend-down statements and bill primary insurance carriers.
Current Performance Improvement Activities
XYZ Health Center organization has plans to monitor, track, and report quality assessments, performance, and improvement through an integrated management system with a functional 360-degree feedback. This system can track and record performance against set goals besides given periodic alerts based on its programming module. The plans comply with MSA Bulletin Number MSA 15-59 through the integration of consistency, dependability, speed, and cost in the quality metrics. The center strives to manage these components to ensure that any unit of input generates optimal output at the least possible costs to make the service charter sustainable in the short and long-term.
Current Challenges
There is a need to improve the operational processes within the Pediatric and Family Medicine office. There are challenges in documentation in medical records, prolonged length of stay within the Pediatric and Family Medicine office, bed utilization, and inadequate space in the general building. For instance, there are a few inconsistent components as it pertains to vaccines in general which makes it difficult to check and balance the billing and inventory. When an order is not placed, it leaves the responsibility on the clinical staff to remind the providers to submit. Also, charges to the account would either be forgotten or entered late.
Another inconsistent task is of the staff forgetting to document the vaccines onto the paper log. If this is not done, then the inventory is out of balance. Also, if both situations occur, that is, the provider missing the order and the staff not documenting the vaccine, then the office could have totally missed a vaccine charge. Moreover, patients take longer than necessary in the office when seeking services and there is inconsistency in the flow within the service charter. As illustrated in Table 2, these challenges were prioritized on order to address the most pressing need at the moment.
Table 2: Prioritization of the current challenges within the Pediatric and Family Medicine office.
As illustrated in table 2, the most pressing challenges that should be handled immediately are the low workflow of services and prolonged stay in the Pediatric and Family Medicine office. Therefore, this business working project is focused on creating a process improvement plan for the Pediatric and Family Medicine office. Specifically, the process will identify quantifiable and effective improvements in the workflow and duration taken by patients during the service process. The plan is expected to improve quality and service delivery by optimizing the input-output function.
Rationale for the Proposed Process Improvement Plan
Based on the challenges identified, there is a need to improve the workflow and duration taken to receive services within the Pediatric and Family Medicine office. This is necessary to help the center achieve its vision of optimal functionality in operations and service delivery through introducing a Business Process Management whose strategy should have futuristic goals. The plan should have a timeline through which the organization operates.
In this case, the manager requires 6 months to provide a report to the stakeholders who are interested in efficient and effective organizational performance. The essential component of the proposed plan is leadership; people change management and BPM project management without which the entire BPM activity should build on. The BPM project indicates that accountability is crucial, but the whole management endeavor requires responsibility.
Summary of the Outcomes or Benefits of the Improvement Plan
The proposed workflow plan for providers and clinical staff is expected to help streamline the process of service delivery by improving the workflow and decreasing the time taken to receive services as follows:
- Decrease the length of stay per client from 7 hours to an average of 4 hours
- Improve the workflow per patient throughout the health center and the Pediatric and Family Medicine office.
- Reduce the financial cost within the Pediatric and Family Medicine office per bed.
Business Process Management as a Perquisite for Quality Improvement at XYZ Health Center
XYZ Health Center needs to come up with an appropriate environment and high-level guidelines on how to execute the strategy of the organization. Alignment is one of the critical structures that a manager needs for achievement from the topmost to the lowest of the body as they allow the business strategy to lead them. The approach of an organization first requires the management to set rules that will govern the organization, known as the Business Operating Model (BOM).
The executed BOM needs a further creation and development of business capabilities that drive the production of the components. The BOM however, contains the unspoken rules and codes of the organization; therefore, it is intrinsic to the way XYZ Health Center operates. The BOM operates under the power of the business capabilities and components such as Processes, People, and Technology.
The people component carries human resource policies, roles and responsibilities, organizational structure, and reward structures. The process component needs several capabilities, frameworks, and governance, including process groups and models, process asset, high-level value chains and architectural framework. The BOM operates and drives the component of technology. XYZ Health Center needs to implement a BPM project management system standing on the three elements mentioned above. Without people, technology, and processes, the BPM strategy shall fail. According to the 7FE approach, the BPM begins its operations after undergoing ten phases enveloped by three major essential components which include leadership, managing change by the people and BPM project management (Kiran, 2016).
The XYZ Health Center requires a significant shift in its operations to optimize service delivery. For a proposed BPM project to be a success, the business outcomes to be agreed upon from the stakeholders, who are required to ensure their dedication and allocate the time to initiate the BPM initiative, as well as to demonstrate their commitment process improvement. The proposed BPM will require a Target Operating Model to ensure an ideal methodology of process operations at XYZ Health Center.
To have an initial start with the proposed process improvement in workflow and duration of service, a workshop will be planned to gather further information and data from the stakeholders. Despite the clear instruction of this BPM requiring a dedication and time from stakeholders, many of them may not attend due to their busy schedule. This lack of dedication from the stakeholders might pose risk to the foundation phase of the proposed BPM project.
The Target Operating Model (TOM) for the proposed plan will set a high-level roadmap for XYZ Health Center’s future business operating model. Kiran (2016) has explained the core components of the TOM in a pyramid figure to ensure alignment and result achievement of the proposed process improvement strategy. The suggested TOM for this initiative is creating the desired operations to transform the Pediatric and Family Medicine office into an efficient and effective section.
It is vital to ensure this TOM is communicated, explained, and understood by the key stakeholders. The TOM explains how each of the Strategic Objective will be achieved through the existing value chain as illustrated in Table 3.
Table 3: TOM in relation to the Pediatric and Family Medicine office’s proposed improvements.
The TOM is necessitated by four fundamental reasons surrounding the BPM processes, purpose, value, and change management strategy. For instance, in relation to the proposed BPM, it would be prudent for the activity team members to capture sufficient knowledge of the present business processes at the Pediatric and Family Medicine office for proactively redesigned at the next step, which is the innovative phase.
The team should also be in a position to carry out a comprehensive comparative analysis of the metrics in relation to the new processes in the proposed. This will enable the activity team to deliver the business value while clarifying the project functionality. The understand phase is also significant in base lining the skills needed to effectively execute the proposed current processes against future modifications for training purposes. Lastly, it is prudent to master the understand phase to commence the personnel change management initiative aimed at unfreezing people for them to understand the need for the proposed change (Kiran, 2016).
This means that the understand phase is vital towards validating the current process reality within the proposed plan in order to define the priorities for improvement as guided by the project scope. The understand face ends at the point where all the stakeholders are made aware of the process involved in the BPM after which these activities are appropriately documented. However, for each process model, it is important to build consensus in the documentation for optimal project acceptance.
Modeling the Proposed Process Improvement Plan
The process modeling within the proposed process improvement plan is significant in gaining consensus, demonstrating any shortcoming, supporting acceptance, allowing evaluation, and creating a baseline for managing inter- and intrapersonal relationships among the team. In order to effectively implement the proposed BPM plan to improve billing, inventory, and general procedures at the Pediatric and Family Medicine office, the steps to be completed include communications, scope revalidation, understanding workshops, complete metrics analysis, root-cause analysis, complete people capability matrix, identification of available information, process worth matrix, highlighting innovative priorities, focus on quick wins, and understanding phase report.
The communication activities will involve providing information to all stakeholders within the Pediatric and Family Medicine office about the proposed BPM plan, its objectives and their involvement. This will be achieved through creating a consultative, warm, and holistic atmosphere for ease of building consensus. At this point, the communication initiatives will be fully integrated in the BPM activity by balancing consistency and efficiency in passing information (Kiran, 2016).
The second step will involve the revalidating of scope of the BPM activity on a continuous and systematic basis by leveraging the primary documents on process worth matrix and process selection matrix. The modeling will capture the interests of the various stakeholder groups.
This step will enable the Pediatric and Family Medicine office to understand the end-to-end processes for effective innovative outcome. The third step is ‘understand workshops’ in order to grasp the necessity of this phase. In relation to the proposed improvement activity at the Pediatric and Family Medicine office, this step will create an inclusive environment for learning the current processes from the perspectives of success, stakeholder participation, and metrics guiding potential priorities and quantifiable benefits. The workshops will be scheduled conveniently and in time followed by framing of the participants against set expectations.
The workshops will be conducted in controlled and structured manner to streamline attendees and agenda for effective end-to-end processes. The fourth step will involve complete the metrics analyzing from the perspective of the targeted customers.
These metrics form the standard for measuring the performance in any given process. Moreover, it facilitates the production of an analytical reflection of the proposed plan by allowing for benchmarking of any available process data such as volumes, task times and cost implications against other similar campuses. The process selection matrix will also be used to estimate benefit and cost implications after which a specific process level will determine the measures for each processing time. For instance, the KIP and SLA would authenticate the measures against any bottleneck (Kiran, 2016). These metrics will be measured at organizational and management levels from the workshops and periodic surveys.
The proposed improvement plan will also involve a comprehensive root-cause analysis for potentially non-performing processes. This approach is critical in understanding errors and their sources, accuracy of information being received, and capacity of the Pediatric and Family Medicine office to meet the desired standards. Through the use of the Failure Mode Effect Analysis (FMEA), it will be possible to establish the process reference, failure mode, root cause, failure effect, residual risk, and severity on total score. This will be used to gain useful information on future and current environment.
In performing the FMEA, it will be essential to examine the current capability as a function of future needs at organizational level in order to identify the high levels for reviewing competency enhancement requirements. During the plan creation, a process selection matrix will be developed for the Pediatric and Family Medicine office as part of the BPM activity. Information identification will be done via the workshops, human resource archives, and interaction with different stakeholders.
Discussion of the Challenges from Capacity Strength
Length of Stay Within the Pediatric and Family Medicine Office
As illustrated in Figure 2, the current process of customer service within the Pediatric and Family Medicine office is complex and multifaceted. The network encompasses policies, process, environment, and people in order to compete the service cycle. Although the system has sustainable the service delivery charter, it has some bottlenecks associated with inefficiencies and inability to balance the competing needs in the utilization of resources. The sections in this process are run concurrently and assumed to be effectively functional. However, they have not been optimized to ensure timely service delivery module.
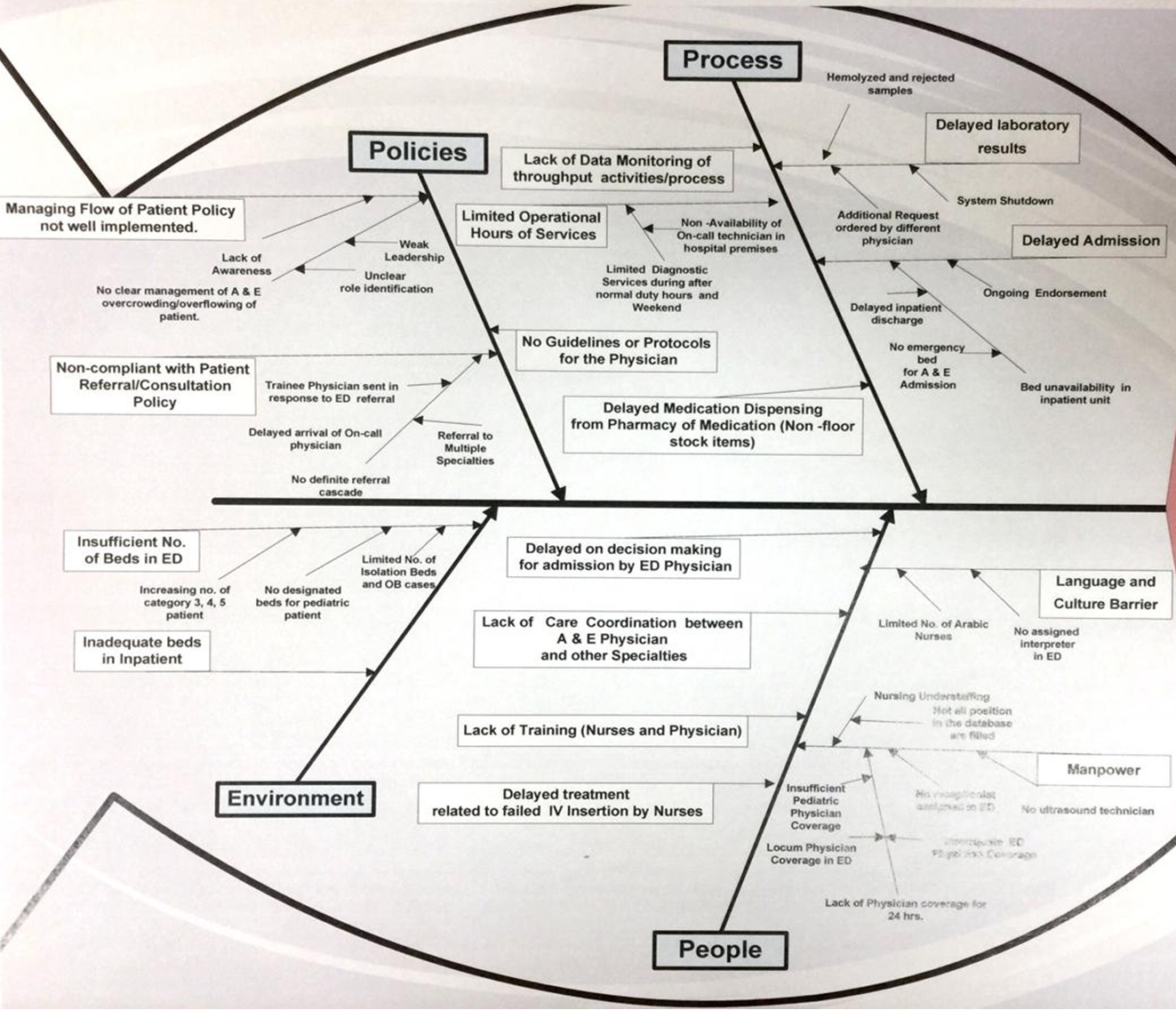
From the available data within the center, the length of stay was averaged for a period of a year, that is, from October 2017 to March 2018. The results were tabulated as illustrated in Table 4 to monitor the trend.
Against an ideal time of 4 hours, the Pediatric and Family Medicine office has experienced consistent reduction in the average length of stay per patient from 12 hours in October 2017 to 7 hours in March 2018. However, the reducing length of stay is still way above the ideal 4 hours. Therefore, there is a need to come up with plans to reduce the length of stay in the line of service from the current 7 hours to 4 hours.
Based on the current length of stay hours against the ideal 4 hours, a financial impact computation was carried out to compare the cost per patient in the Pediatric and Family Medicine office against the cost per inpatient clients admitted in the health center. The current average cost per patient per day at the Pediatric and Family Medicine office per hour is $20 while inpatients are charged 200$ per 24 hours. As illustrated in Table 6, the findings indicated that the Pediatric and Family Medicine office might be able to save more than $100 per client per day if the length of stay is reduced from 7 hours to 4 hours.
Table 6: Comparative cost implication of reducing the length of stay from 7 hours to 4 hours.
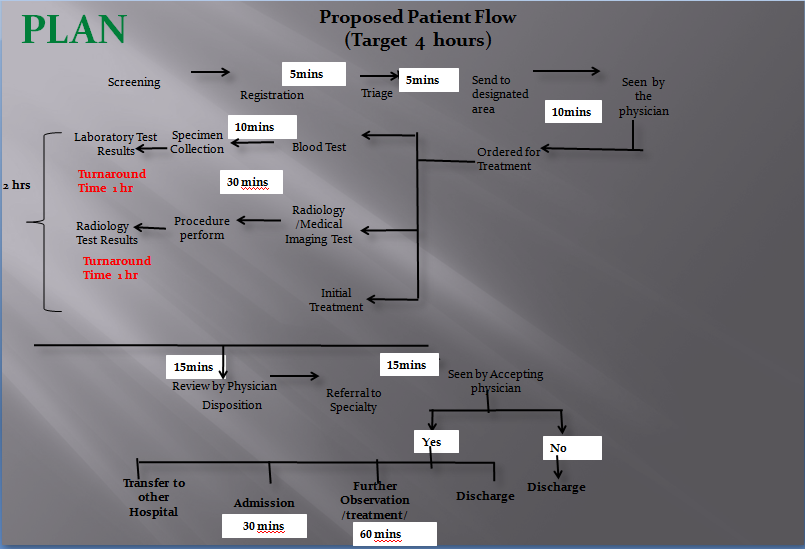
Proposed Plan to Reduce the Length of Stay
The proposed plan to reduce the length of stay was organized into a ten-item project that targets to create a holistic and sustainable service improvement in the Pediatric and Family Medicine office. The process was focused on reducing the flow of services from the current 7 hours to 4 hours over a period of 6 weeks. The propose plan encompassed systematic collaboration and intentional improvement of the current process inefficiencies as illustrated in Table 7.
Table 7: Proposed plan for reducing the length of stay.
The content in Table 7 was illustrated in graphs to explain the relationship among the suggested improvements. As captured in Figures 3 and 4, the proposed plan involved distribution of activities with estimated timelines to ensure that a complete service per client does not supersede four hours running concurrently.
Actions Taken
The Pediatric and Family Medicine office was modified to by adding 3 stations to avoid overflowing or overcrowding situation in this section. The new sections are the records desk, data entry desk, and record automation desk. The revised and reviewed policies involve managing patient flow, patient consultation/referral, and laboratory activities. The revised policy was focused on addressing the currently high census situation in the office and monitor or cascade the aspect of compliance. The laboratory activities were automated to ensure that the aspects of sample collection, requesting, identification, dispensing and storage processes indicated downtime or failure.
In order to address the challenge of insufficient manpower, a new physician consultant and three desk clerks were added in the triage area. In addition, an arrangement was organized for technical coverage of the lab processes within the official working hours and over the weekend. In order to minimize potential language barrier that would slow down the service process, an interpreter specialist and an automated interpretation machine was introduced in the office.
Moreover, the current workforce was arranged in such a manner to foster quick and accessible communication with the clients. Data on language proficiency was collected and stored for backup to assist, depending on the language of a client. As a strategy for reducing the delay in admission, the office introduced an effective records section through the new three desks to ensure that the records of clients are captured within 5 minutes.
In terms of training and education, a systematic program was introduced in the office to ensure that the personnel are periodically sent for training. Specifically, two physicians were enrolled in training after which they were expected to train the rest of the staff in this office. Moreover, a system was put in place to carry out continuous education and semiannual competency.
Projected Results of the Improvement Plan
Since the proposed improvement plan will reduce the patient service duration to 4 hours, from the current 7 hours, projections were made on the basis of past trend while introducing the proposed improvements. The projections were benchmarked against the ideal service duration of 4 to 4 to 5 hours, averaged at 5 hours in the worst case scenario. In project management, the use of maximum of the minimum is ideal for guarding against overestimation.
The results of the improvements were compared to the results before the improvements. For instance, in the triage area, benchmarking for the waiting time were compared before and after the implementation of the proposed reduction of the length of stay per patient per complete service cycle. As captured in Figure 4, there were improvements in the waiting time from 11.5 minutes in January to 7.25 minutes in October. Equilibrium waiting time was reached between June and August at an average of 5 minutes.
The increasing waiting time thereafter could be attributed to increased efficiency, thus, ability to serve more clients, which automatically increases the waiting duration. The increasing waiting time from August 2018 could also be associated with existing inefficiencies that are common with a new system as the personnel face the challenge of adjusting appropriately. Interestingly, the addition of an extra physician ensured that the queue at the triage moved relatively faster as compared to the previous situation before the improvement plan.
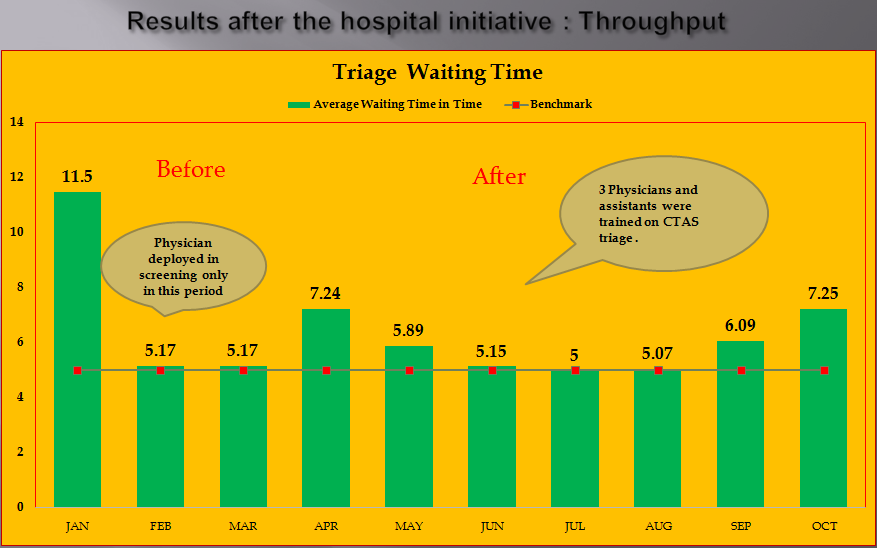
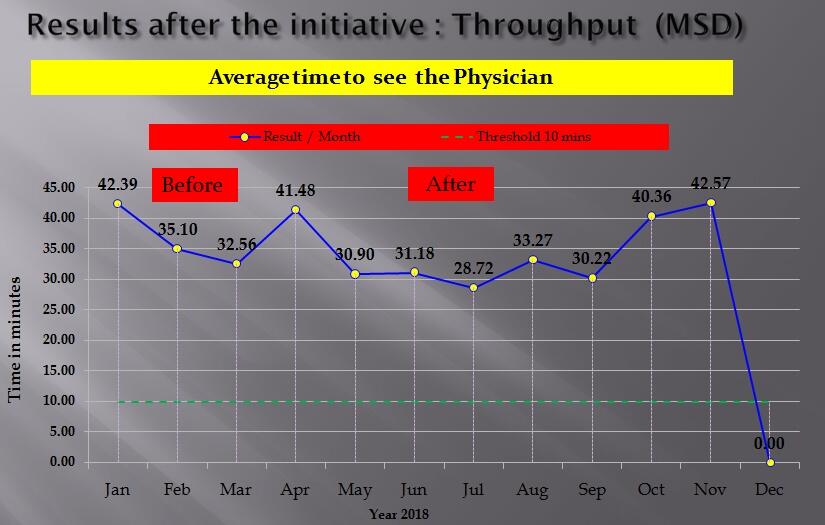
In order to confirm the changes in waiting time apply to all other processes within the Pediatric and Family Medicine office, same data was used to establish average time it takes to see a physician before and after implementation of the plan. Since the plan was implemented from April, there was consistent reduction in the time it takes to see a physician at the Pediatric and Family Medicine office as illustrated in Figure 5. After 7 months of implementing the proposed improvement plan, the average time it takes to see a physician reached an equilibrium used to benchmark at 10 minutes. Setting of the benchmark for improvement was done after every ten minutes.
However, instances of non compliance were reduced significantly as compared to the period before the improvement initiative. The trend further indicated that the average time reduced further below 10 minutes. This is an indication that it took several months to implement the improvement plan and create capacity for its functionality. Apparently, it is in order to confirm that the improvement plan had positive results and met the expectation within 6 months of implementation.
Summary of Findings before and after the Improvement Plan
Apparently the Pediatric and Family Medicine office overcrowding is contributed by inefficiency in service flow and increased number of patient orders. The increasing number of clients translated to prolonged waiting time, thus, overcrowding. Moreover, the service flow is inconsistent due to imbalance in the processes within the health center. As a result, the service duration at the health center takes an average of 7 hours, which is almost double the benchmark time of 4 hours. Fortunately, the proposed improvement plan has successfully achieved its aim and objective of reducing the waiting time to about 4 hours.
Prior to implementation of the proposed plan, the length of stay ranged from 12 to 7 hours. Moreover, the plan has resulted in a decreased number of patients who over stay in the center. Interestingly, there was a general improvement in the throughput activities or patient flow after the implementation of the improvement plan. For instance, there was an improvement in the triage process. The start to end time of triage declined from an average of 11.5 minutes to 7.25 minutes per client after the implementation of the improvement plan. This was achieved through competency and triage re-training of the involved personnel.
Despite these successes, there is a need for continuous process for monitoring progress to sustain compliance. Apparently, the output, input and throughput in the Pediatric and Family Medicine office should be organized in a systematic manner to minimize any reoccurring bottlenecks associated with increased costs. For instance, through a systematic and focused time management, it will be possible to sustain the observed improvements and reduce the patient stay while increasing the number of clients served in any single day. The proposed benchmark ensured that the ideal timing is met to overcome incidences of increasing length of stay per client seeking services.
Although the improvements only focused on the procedures at the office, there is a need to also integrate other structural improvements in the spacing to accommodate the demand of the growing number of client seeking services at the Pediatric and Family Medicine office. For instance, an extra physician at the triage will improve effectiveness and efficiency. As a result, positive beneficial effects such as reduced departmental cost and increase patient flow for sustainable service delivery charter. Moreover, there is a need to improve the patient referral approach through focused and systematic compliance monitory and training programs.
The currently standardized communication system should also be adjusted to guarantee smooth flow of information. In addition, the data collection methodology in line with the required metrics should be improved to balance the aspects of inputs, throughputs, and outputs in the entire service process. In the long term, there will be a need to expand and renovate the Pediatric and Family Medicine office to sustain the projected increase in patient flow due to improved efficiency.
Metrics for Tracking Improvement in Flowchart: Cost and Efficiency
The metric used to measure the soundness of the flow chart is the time taken to receive and process the patient service per client. The entire process should not go for more than four hours. Another metric is the accuracy and efficiency in the balancing of the service process. This is measured by the number of clients served within the stipulated timeline. In order to foster further improvements, patient records should be merged into one function to avoid duplication of duty. At present, the verification process is repeated in two stages, which is a waste of time and hospital resources.
Through merger into a single step, the Pediatric and Family Medicine office might avoid wastage of the labor resource that could be channeled to other important areas. For instance, the office clerks could do the matching and verification at once followed by the assistant clearance. This will shorten the time taken between documentation and seeing a physician. Apparently, the awareness of a workflow of different activities is important in tracking and understanding the processes involved to complete a service cycle. The entire process could be subjected to feedback metrics for improvements or complete change.
Implementing Improvement Plan
After the development of the improvement plan, it is time to produce the solution prepared, which place the development phase in parallel with the people phase. New system development requires care and sufficient flexibility that can adopt any near future change by meeting business change. There are two possible proposed ways to develop BPM solution, which are the traditional way of software development life cycle (SDLC) also known as waterfall, or the Rapid Application Development (RAD) also known as iterative and agile.
As for the modeling of the improvement plan for the Pediatric and Family Medicine office, the team proposed that it is an agile way of development due to a short timeline for implementation, that is, 6 months. The quick wins will then be identified via workshops to validate any feasibility of the proposed improvement sustainability. After validating the implementation, considerations will be given to creating a sub-project team tasked with the duty of implementing the quick wins. Project modeling will end with reviewing the process report in terms of findings for the current processes, metrics, identified quick wins, and potential risks against mitigation strategies.
In order to effectively maneuver the dynamics within this phase, a series of documentations will be generated and integrated to foster creativity and complete commitment. These documents are aimed at redesigning the process models, clarifying any high-business need, and simulation of activity-based details of costs. Moreover, this phase will address the capacity planning, review of alternatives against stakeholder expectations, and capturing the process gap report. Since this phase integrates the people value in implementation, the plan will schedule the personnel development needs and present a detailed cost-benefit analysis for the improvement project activity.
The plan will be updated frequently on a need basis to quantify the costs and benefits from the assessment of the project’s impacts, in terms of intangible and tangible gains. In addition, this phase will outline the steps to be taken, alternatives considered, comprehensive analysis, results, and recommendations. Since the improvement plan is a complex project, this phase will be accompanied by a presentation to the management on the proposals and direction to be taken to turn the Pediatric and Family Medicine office around. This will be achieved through creation of an improved communication plan targeting all the stakeholders.
As a strategy for countering the common misconceptions about the proposed change plan, this phase will be developed through the integration of workshops in each process. Each workshop will be structured differently through upfront planning. Specifically, each training session will internalize the process being adjusted until it is completed using the end-to-end meter. Since the XYZ Health Center has many departments, the workshops will be organized by crossing the departmental boundaries for an effective integration. Moreover, the workshops will be created in a way that they are not limited by the current organizational structure. The process will be flexible, expansive, and inclusive to guarantee stakeholder support.
As part of the critical thinking strategies, the proposed implementation modeling for the improvement plan will involve aligning the perceptions of the stakeholders into the right thinking frame for effective involvement, implementing the innovative or creativity activities through engagement of the current employees, and determining and preparing the course of action against solutions proposed. These suggestions will be executed through a streamlined approach and subdivided into other phases for ease of control.
For instance, in order to make the modeling strategies relevant to the improvement project activity, the process will include a redesign matrix for tracking potential opportunities tied to different innovative alternatives. The opportunity redesign matrix will be laden with a stable innovation process that balances the way services are processed and conventional structure of the entire service charter. Therefore, the improvement modeling approach will involve introduction of the end-to-end process modeling to provide expansive opportunities for process improvement.
Prior to implementing the training workshops, it will be necessary to understand the required innovation and the best strategy for internalizing the needs of stakeholders. As a result, the innovative processes will achieve high effective service and satisfaction levels. Therefore, an ideal process management should be controlled using the end-to-end perspective to interface areas of the activity that are deemed to have significant improvement opportunities. The proposed improvement project will attempt to balance the impacts of different levels of customer satisfaction through improved service excellence.
For instance, through optimizing the zone of margin effect, it will be possible to avoid the irritation level by creating a line of absolute indifference that transition towards timely and optimal services. Actually, it is the process that will matter in executing the project modeling and actualization through understanding the variations between customer satisfaction and excellent service. For instance, a wow factor could be easily eroded by consistent poor service charter. Thus, the hygiene factors will be adequately taken care of before integrating the wow factors in the effectiveness charter. For example, this phase will be modeled around elimination of irrational factors to improve on customer satisfaction and higher service levels.
Communicating the Proposed Changes to Stakeholders
The communication stage will involve informing stakeholders about the scope, options, and status of the improvement project activity. This stage will integrate input of the stakeholders in order to gain understanding of the choices and objectives of the activity. The executive kick-off workshop stage will be integral towards knowing the goals associated with the proposed improvement activity for the Pediatric and Family Medicine office in terms of timeframes, strategy, planning, constraints, successes, and process optimization among others. The third step will involve updating the innovation approach by reviewing the present plan against standards for correct personnel in the workshops.
The updates are necessary for tracking different scenarios associated with implementing a complex project such as the proposed plan. The next step will be gathering and establishing consensus among the external stakeholder focus groups in order to capture their insights in the workshops. The fifth step will be internal mobilization of innovative ideas by focusing on quality instead of quantity of the suggestions. This process will be implemented through a competitive approach in collecting surveys, outcomes, and previous activities.
Information and communication supports will be incorporated through the use of consistent repetitive rules, unambiguous roles, and strategic decision-making to make the information discharge more effective. As a result, the communication phase will be characterized by reduced cost, improved quality, and consistence with the compliance needs of the center. Preparing the innovate workshops and their implementation will be performed on the basis of expected outcome.
Since the plan intend to improve on quality of service and other processes within the Pediatric and Family Medicine office, future process metrics projections will be used to understand the operations costs, and additional opportunities or benefits of the project. Moreover, continuous simulation will be performed to determine the efficiency and feasibility of the proposed adjusted process options. Through a detailed metrics analysis, it will be possible to quantify the potential benefits. Among the workshop proposed solutions will include an update of the people capability matrix, process gap analysis, and demonstration of the proposed solutions’ feasibility.
The benefits will then be identified and reported to the stakeholders and their approvals will transform the proposal into a viable project. The business requirements such as realized value and output will provide the matrix for measuring success or any need for further adjustments.
Key to Effective Change Communication and Acceptance
As a building block for social cohesion, an integration of social capital is a prerequisite for development of sustainable inter- and intrapersonal relations to encourage teamwork. This means that the success of any initiative can only be quantified by the nature of established collaboration, especially where there were no such relationships. An effective socially-based and action-oriented strategy is integrated into a learning system when the stakeholders institutionalize professional communities in places where there were none.
For instance, in relation to this project, there is a need to take a proactive position in establishing an action-based plan aimed at empowering the social and technical skills of the staff. The primary intention of this plan is to encourage progressive learning by reducing any staff-patient interaction challenges. The initiative will excel because of its comprehensive nature in balancing actions and socialization strategies into a well-decorated and practical manual. As a result, the Pediatric and Family Medicine office will be able to proactively track performance of the service charter environment and during execution of other duties. Moreover, the center will be able to foster strong relationships among the personnel through an interactive but flexible cooperation manual.
This strategy has the merit of removing the bottlenecks that impeded professional interaction among staff members. At present, the center’s performance tracker through the 360-degree feedback has recorded positive results for the last three years. The trend is predicted to persist in the foreseeable future due to its positive outcomes in the performance and interpersonal relationship building, especially when integrated in the proposed improvement plan.
An effective action-oriented intervention strategy should institutionalize capacity building. Lack of capacity is characterized by the inability of an individual or a group to perform optimally or within the expectation due to limited skills for self-improvement. As a result, such an individual or a group would embrace an indifference attitude towards performance improvement. In relation to the same performance improvement plan discussed previously, the initial stage of its implementation was met with resistance from the expected beneficiaries. This is because many stakeholders throughout the process would interfere with their daily activities and disrupt their comfort zones in the Pediatric and Family Medicine office.
This means that the personnel felt little motivated to embrace the idea since its benefits were not clearly explained. In order to overcome this stumbling block, change implementers will have to initiate a proactive capacity building process that is inclusive and accommodative to all the stakeholders. Specifically, the capacity building process will begin by exploring the need for the proposed change plan, benefits, and potential impacts on the general performance of Pediatric and Family Medicine Office’s improvement project. Moreover, the capacity building meetings will be organized in an interactive manner to capture the inputs of all stakeholders.
As a result, all stakeholders are expected to unanimously agree to integrate and internalize the improvement project into a service model for effective execution and general performance. Reflectively, the integration effort is expected to be successful since the service charter will improve as the workforce is empowered to be more participatory and in control of the patient service delivery charter.
The process of change planning and management is dynamic and multifaceted. Therefore, in order to proactively and effectively foster and manage change, there is a need to create a manual with the primary functioning conditions to transformed the undesired performance level to expected improvement standards. In the case of the Pediatric and Family Medicine office improvement plan, it will be necessary to institutionalize a collaborative culture between the stakeholders to build a positive pressure. The resulting effect of this pressure is direct motivation of the stakeholders to execute their duties without conflict. Moreover, the positive pressure improved the level of accountability among the stakeholders to catalyze the desired change.
During the collaboration, the stakeholders will be empowered to eliminate motivators of poor performance to promote positive feedback. In order to accomplish the positive attitude, the Pediatric and Family Medicine office will introduce a series of periodic meetings at the beginning, mid and end of each month for all the stakeholders. These meeting will be used to encourage positive bonding among stakeholders and create a platform for discussion of current and expected performance. Through collaborative change implementation approach, it is in order to state that the strategy will succeed in creating a holistic performance guided service environment within the Pediatric and Family Medicine office.
Conclusion
Every project under the BPM strategy should have futuristic goals. The plan should have a timeline through which the organization operates. In this case, the Pediatric and Family Medicine office required improvements in the patient waiting time and workflow to reduce the service duration from 7 hours to 4 hours. The essential components of the plan depend on the ability of the center to integrate transformational leadership strategies; people change management and BPM project management without which the entire project activity should build on. The BPM project does not indicate that accountability is crucial, but the whole management endeavor requires responsibility.
Every leader needs to account for their contributions to the achievement of the set priorities and goals. This means that the success of the proposed project plan depends on the ability to pull together an effective implementation team, which is focused on realizing the project deliverables against a series of benchmark measures. Every person in the implementation team should have excellent plans which require continued support from the top leadership and accountability. The findings and evaluation of the proposed improvement plan indicates that it is possible to reduce the service duration from 7 hours to 4 hours over a period of four to six months of implementing this project. Specifically, the plan has confirmed that the delay in service charter is attributed to imbalances in the inputs, throughputs, and outputs in serving patients.
For instance, the prolonged time in registration and seeing a physician was associated with mismatch in manpower and information management. The project plan has also confirmed that adjustments within the Pediatric and Family Medicine office, in terms of structuring the service points might increase the office’s ability to serve more clients. As estimated in the project plan, an effective implementation strategy might reduce the cost implications incurred at the Pediatric and Family Medicine office by up to 45%.
Fortunately, the Maximin Costing approach used in estimating the cost will ensure that more benefits might be achieved over a prolonged period of time. However, the success of the entire project is angled on the ability of the implementation team to create an effective communication and stakeholder engagement program. This is necessary for project acceptance. In general, the proposed plan has achieved its goals of reducing the length of stay per customer and increasing the workflow to ensure more clients are served.
Reference
Kiran, D. (2016). Total quality management: Key concepts and case studies. New York, NY: Elsevier Science.