Introduction
In this case study, the investigator focused on ischemic stroke, one of the most common types of stroke in the world. Ischemic stroke, as Bhatnagar et al. (2015) observe, is a medical condition where a blood clot blocks a vital vessel that transports nutrients into a given part of the brain. If it is not addressed urgently, the cell in that part of the brain, which is denied blood, starts dying. The author selected a patient with this condition because of the agony she was going through at the time she visited the hospital.
The patient had an intense headache at the time when she was admitted to the unit. She appeared confused and did not understand simple questions or instructions given to her by the medical team. This life-shortening illness is currently a major pandemic in the United Kingdom (Ciccone et al. 2013).
The relevant statistics provided by numerous healthcare units indicate that approximately 152,000 cases of stroke occur in the country every year (Ahn et al. 2013). It means that for every five minutes, the health problem emerges. More than 1.1 million people in the country are stroke survivors, some of whom are under close medical observation because of their delicate conditions. Lee (2017) argues that other than being a major cause of death, stroke is also a leading cause of disability among adults who are lucky enough to survive it. They have to rely on their family members to lead a normal life because some of them are paralysed in various ways (Fleisher 2013).
About 50% of cases of stroke reported in the country are caused by high blood pressure. A report by Doeppner and Hermann (2016) estimates that for every 100,000 people in the United Kingdom, 380 men and 299 women suffer from stroke. Through the efforts put in place by the government and private stakeholders, cases of stroke declined by over 24% in women and 18% in men from 1995 to 2004 (Lapchak & Zhang 2017).
Goyal et al. (2015) argue that the African-Caribbean people are the worst affected group. The condition is not unique in the United Kingdom (Williams, Perry & Watkins 2013). The World Health Organization estimates that about 15 million people across the globe suffer from a stroke (Bhalla & Birns 2015). In the given paper I will revolve around the state of a particular patients health and her current condition. I will introduce the confidentiality statement to ensure that her agreement is obtained.
The paper will also contain such sections as the patients presentation that describes her current state; pathophysiology that demonstrates peculiarity of the suggested health problem; physical, social and psychological changes in the patient under the impact of the stroke; medical/nursing care part that discusses the provided treatment and medications; integrated care; health promotion and patients empowerment and conclusion sections. These are the basic parts of the paper needed to investigate the case.
Confidentiality Statement
When conducting this case study, it was important to observe the code of conduct set by the Nursing and Midwifery Council (NMC) (2015) to ensure that the patient will not suffer from unethical actions or abuse of basic human rights. Additionally, basic human rights guarantee non-interference in a persons private life and protection of information he/she does not want to share (NMC 2015).
For this reason, all participants should demonstrate their desire to participate or provide data. Assuring patients of the commitment to protect their identity is one of the aspects that make their participation in the project more probable (NMC 2015). The author ensured that the name, exact location, and age of the patient remained anonymous; hence she is only referred to as Jane. In such a way, her informed consent was acquired. She did not participate in the study; however, she agreed to provide all information about her case to the researcher and said that it could be used for the investigation.
Patient Presentation
The patient was an adult female who was admitted to the hospital with a complaint of an intense headache, poor coordination of body parts, faecal incontinence, and general confusion. She was brought in by ambulance paramedics after she felt extremely bad and her close people noticed the first signs of the disease when she was at home.
At the time of admission, she demonstrated reduced communication and cognitive skills – sometimes she could answer simple questions correctly; however, in the majority of cases, she was not able to find an appropriate answer as it was difficult for her. However, the medical team was able to get past medical history of the patient. Jane reported that she has never been admitted to a hospital in her adult life. She stated that over the past three years, she had been experiencing discomfort in the chest and at the back of her head, but considered it a minor issue that did not warrant hospitalisation.
The patient is a single mother of three (a boy and two girls). Within that period, she has been the sole breadwinner for the family. She reported that she had two jobs. This middle-aged woman stated that her eldest child is aged 12 while her last-born is only 4 years. She has been able to meet all their basic needs, and all of them attend school. Her current partner plays a very limited role as a parent and a spouse in the family. He is always out of the house, and she noted that one could not predict when he would be back. She is worried that her current condition might have a pernicious impact on her children as there were no relatives to care for them, bring them back from school. Her partner is not responsible and could not be trusted. It evidently impacts her state.
Pathophysiology
Ischemic stroke is characterised by a sudden loss of circulation of blood to a given part of the brain. Lee (2017) states that depending on its cause, it may take different paths. Acute ischemic stroke, as Lohse, Lang, and Boyd (2014) observe, is caused by embolic or thrombotic occlusion. If the blockage affects a large area of the brain and it is not addressed within the shortest time possible, then one can lose his or her life. Sometimes it may end in paralysis even if one is lucky enough to get the right medication in time.
The Patient’s Case
The patient complained that she was having a sporadic severe headache that caused her lack of comfort. Therefore, the symptoms exhibited by the patient and the outcome of the medical examinations strongly suggested she was suffering from ischemic stroke. The emergence of the health problem was preconditioned by the thrombotic occlusion observed in her brain. The most probable causes for the appearance of the thrombotic occlusion are hypertension (the patients blood pressure is higher than the norm), and the high level of stress. Altogether, hypertension is of the central factors for stroke.
Thus, the circulation failure in the patients brain preconditioned the appearance of oxygen deficit and a decrease in specific functions. With time, it resulted in the deterioration of the patients speech, cognitive function, movements, and other symptoms peculiar to stroke. The inability of the patient to raise both hands in a coordinated manner must have been as a result of primary motor cortex being affected. At the same time, paralysis of some limbs, problematic movement, speech, language problems and a specific behavioural style demonstrate that the left brain is affected by the stroke and the thrombotic occlusion could be found there (Lee 2017).
The cells in this part of the brain that was denied blood started dying because of the lack of nutrients and oxygen. For this reason, the inability of the left brain to function in an appropriate way resulted in difficulties in walking. The patient may also have other physical or mental issues and problems with eyesight if the investigation discovers the corruption of optic nerves.
Physical, Social, and Psychological Changes
It was established that the condition of the patient had a significant impact on her life from various dimensions. Based on her accounts about the experiences she has had since the symptoms started getting serious and the physical observations and tests, the team established that a number of things have changed in her life and the people around her. She is going through challenging times, and it is unfortunate that it took her so long to know about her condition.
Psychological Impact of the Condition
Barrett and Meschia (2013) say that stroke may have a significant psychological impact on a patient. It was our responsibility to inform the patient about her condition and to explain how she could deal with it in the best way possible. When looking at the psychological impact, it is important to look at it before and after Jane received the information about her new condition. When working with the patient, I engaged the patient to understand the kind of experiences she has gone through and how the problems that she has been having impacted on her psychologically. Thus, at the moment she feels so lonely and rejected, especially considering the fact that her partner avoids communication with her.
When the patient was told that she had been diagnosed with ischemic stroke and she was lucky enough to receive the needed care, Jane demonstrated an apparent emotional response. It was evident that the patient was in a shock. The patient remained motionless for several seconds, lying face down in bed. The team wanted to help her through this challenging experience, so they gave her time to absorb the news.
However, when she turned to face us, she was dejected and somehow harsh. She was in denial, a common stage among patients diagnosed with life-shortening illnesses, especially if their condition is not stable, as was the case with her (Berkhemer et al. 2015). She was given time but maintained tight surveillance on her to ensure that she does not harm herself or others around her. When I finally offered to talk to her, she started sobbing.
She was constantly referring to her children and the extent to which they would be left to suffer if she succumbs to the disease. After giving her some time, she was able to accept the new condition, but it was evident that she had a sense of rejection even after several sessions with a psychotherapist. Her biggest worry, which was valid from a medical point of view, was that even after surviving this first attack, she might be permanently paralysed for the rest of her life and will not be able to look after her children.
Socioeconomic Impact of the Condition
According to the patient, the condition will have a serious impact on her social and economic life. As the sole breadwinner in her family, the patient has to work on a daily basis. To increase her income and improve her family’s standards of living, she has been working two shifts. However, that may not be possible because of the disease. The pain and fatigue have made it impossible for her to go to work on a regular basis.
Additionally, her current state will likely result in the appearance of new problems with finances. The situation may be worse in case she is paralysed by this condition. She laments that no other responsible adult is around who can ensure that the family has the basic needs, let alone caring for her as would be expected. She feels that the life of her and her family may be completely changed for the worst.
Over the past year, the patient has spent a lot of money on the over-the-counter medicine to deal with the pain. The cost of medication is an additional expense that she has to meet. The patient narrates that within the last two months, she and her children have been forced to change their lifestyle because of a reduced source of money and increased expenses. It means that today, due to the ischaemic stroke, the situation could become worse. The patient is depressed by this fact and is scared that she will not be able to take care of her children and social services will take them. In such a way, at the moment money and her children are the major concerns.
Physical Impact of the Condition
Currently, the main physical impact of her condition is her inability to coordinate her arms and legs. The team observed that she has a fallen face, which has slightly changed her physical appearance. However, the patient fears that she may have serious physical problems in case her condition leaves her physically paralysed. She looks weak and very pale. Although she demonstrates tendencies towards the improvement of the state, she is barely able to bathe herself.
She is yet to gain proper physical strength in her arms. She feels that her fallen face has negatively affected her beauty. The condition has resulted in excruciating pain, especially the constant headache. The patient noted that lack of physical strength had forced her to delegate some of the family chores to her eldest daughter, something that she had never considered doing before. However, the family had to adjust to the new lifestyle due to the patient’s condition.
Medical/Nursing Care
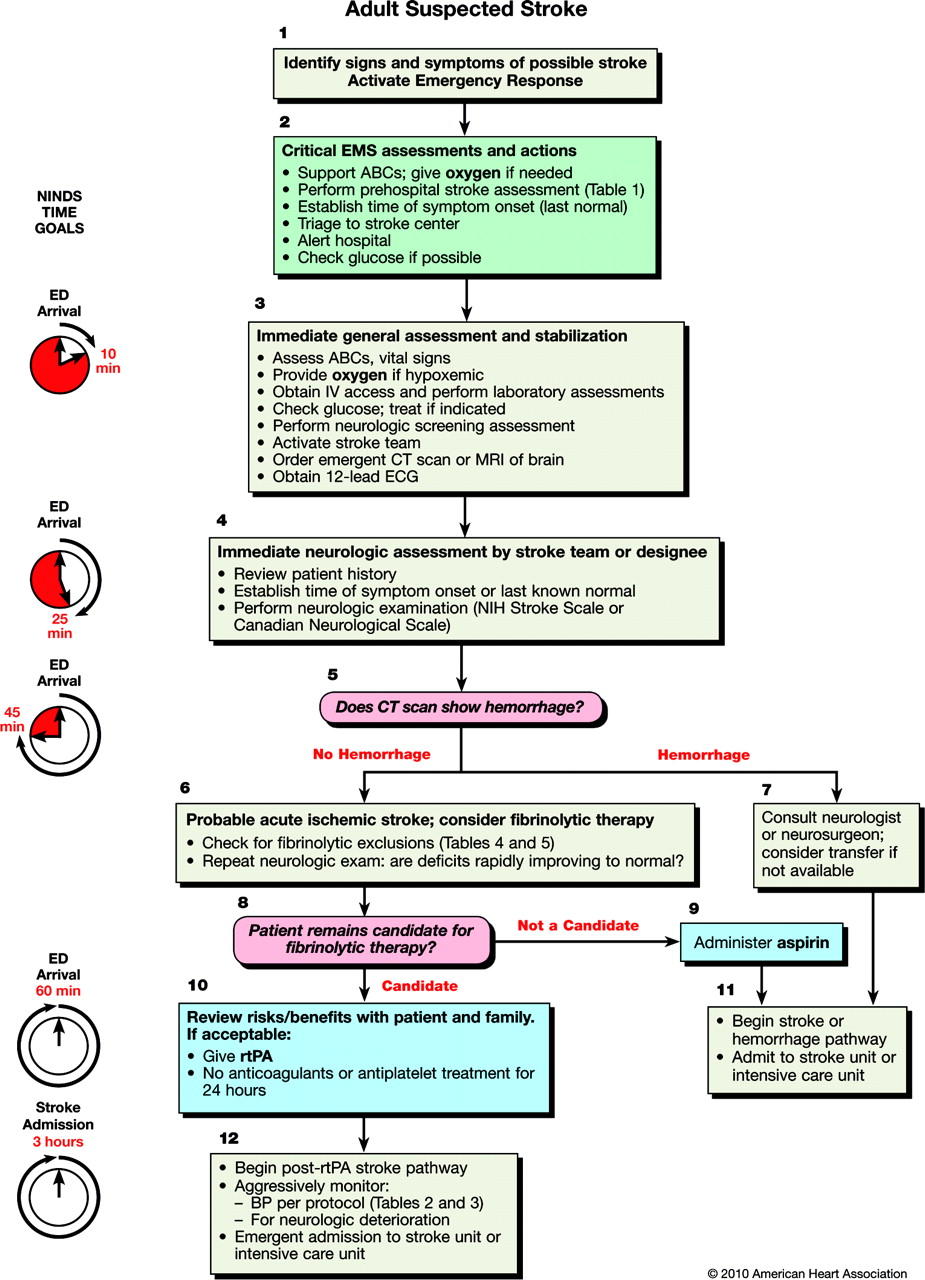
When the patient was admitted to the hospital, it was critical to attend to her as soon as possible because her condition was considered an emergency. A team of medical experts (physicians, cardiologists, neurologists, nurses) was quickly assembled to handle the patient and start treatment using specific guidelines (Figure 1). The medical team initiated diagnosing by physically examining the condition of the patient.
The doctor then asked about the historical record of the problem, when it started and the nature of the discomfort that the patient has had. The patient stated that she had a frequent headache, straining of the left eye or sometimes both eyes, and discomfort at the back of her head. The blood pressure test revealed that she had a higher than normal blood pressure level, at 148/95 (Campbell et al. 2015).
The doctor recommended a computerised tomography (CT) scan to determine the cause of her lack of proper coordination. The scan revealed a minor blockage in one of the vessels that supply blood to the left side of the brain. The brain cells in that part of the brain were not adversely damaged, but the continued blockade of the vessel that transport blood into that part of the brain was putting the patient in danger. It was at this point that the medical team confirmed that the patient was suffering from ischemic stroke.
When the diagnosis had been determined, the medical team ensured that policies set by the National Institute for Health and Care Excellence regarding the specialist care, pharmacology, nutrition, and care delivery were followed strictly. These also include administration of appropriate medications, procedures, and interventions to avoid the further deterioration of the state of an individual.
For this reason, the first urgent care that was given to the patient was the administration of medicine to improve blood flow (National Collaborating Centre for Chronic Conditions 2008). Recombinant tissue plasminogen activator (rtPA) was administered immediately by the physician, as recommended by Food and Drug Administration (FDA) (Wardlaw et al. 2012). As Campbell et al. (2015) observe, rtPA helps in dissolving the clot. It also improves the flow of blood to parts of the brain affected by stroke. In accordance with the existing guidelines, the recommended dose is 0,9 mg/kg with the 10% of the total dose that should be administered as an initial intravenous bolus over 1 minute and then infused during 60 minutes (Peschillo 2016).
For this reason, the patient was provided with 50 mg Activase (generic name Alteplase) (Acton 2012). The monitoring for bleeding was also introduced. Continuous hemodynamic monitoring to scan blood pressure an avoid its increase was implemented. These measures helped to stop the further deterioration of the patients state and serious brain damage. After the administration, the patient should continue taking warfarin to prevent the development of thrombosis (Ovbiagele & Turan 2016).
As for the nursing care, it should be focused on the rehabilitation and minimisation of the negative impact ischemic stroke might have had on the patient (Chang 2014). Nurses assessed the patients memory, cognitive function, orientation, speech, movement, etc. (Roedde 2012). Regarding the nature of the disease, the nursing care also included the focus on impairment of function in diverse daily activities.
There was a particular nurse who worked with a patient constantly to monitor alterations in her state and report them to therapists with the primary aim to introduce new interventions if they are needed or alter the existing ones to guarantee enhanced results. The patient was educated about the rehabilitation practices needed to restore her damaged skills and improve the quality of her life. In the majority of cases, all important portions of information were followed by the detailed explanation provided by the nurse.
Additionally, all rehabilitation procedures starting from those aimed at the restoration of the patients cognitive function and ending with her motor function were introduced by a team consisting of a nurse, therapist, and other specialists responsible for the provision of this sort of intervention. Moreover, Jane had consultations with a psychologist to decrease her panic regarding the diagnosis and cope with the problem. In general, the appropriate delivery of nursing care becomes crucial in cases of Ischemic stroke as it is a central element of the recovery process.
Integrated Care
Integrated care, also known as comprehensive care, or holistic care is a new trend in care system where an emphasis is placed on a coordinated form of care provision (Palmer, Brown & Hobson 2013). The approach is gaining popularity because it integrated primary care, management of mental illnesses among adults, and management of common physical conditions. Davies (2012) says that is important to note that the state of the patient needed attention in all the three areas mentioned above (primary care, management of mental illnesses, and management of common physical conditions).
When handling this patient, the inter-professional team involving doctors, nurses, and even social workers was focused on the restoration of the patients health statues and guaranteeing her complete recovery (Saver et al. 2016).
Incorporating this holistic approach will not only help in managing the patient’s medical condition but also mental problems that she is currently battling. Therefore, it is encouraging that this hospital has developed its integrated care pathways that enable doctors and nurses to work closely and in a coordinated manner when managing patients (Siotto et al. 2017). The same we could observe in Janes case as the efficient cooperation of specialists helped to improve her health.
The difference in approaches is mainly caused by laxity of the management to implement the policies strictly. As explained in the pharmacology section above, management of the patient’s condition required multidrug therapy (MDT) to ensure that entire process was holistic. The United Kingdom’s government has come up with various strategies to help promote integrated care, such as the NHS Five Year Forward View, House of Care Model, and Wanless Report (Kernan et al. 2016).
Thus, the central idea of this report is the provision of the combination of services to ensure that a patient will rehabilitate and improvements in all aspects of his/her life would be admitted. In such a way, in accordance with this report, Jane was provided with comprehensive and integrated care. First, as it has already been stated, her children are the main concern as the patient is the only close person who cares for them. In such a way, health workers of the hospital informed social workers about the complexity of the case and a problem that appears due to Janes health issues. Social workers suggested communication with the father to guarantee that children will be protected.
However, this idea failed as the man did not have any desire to help his former partner and look after adolescents. It is apparent that this fact had a pernicious impact on the patient and her recovery as she was worried about her childrens destiny. That is why social workers suggested a specific pattern that presupposed their assistance and provision of the needed care for Janes family. In other words, a person was appointed to live with children, feed and protect them. The patient accepted this very approach as it was the only possible solution to the problem. At the same time, being a social program designed for people who suffer from particular diseases and experience financial or other needs, the provision of this assistance was voluntary.
All social workers were volunteers who wanted to help Jane to recover and ensure that her children would be fine. This program perfectly demonstrates the efficiency of the integrated care and the high need for policies of this sort that will be focused on the provision of specific and complex care to patients who need it because of diverse limits or barriers. Although these policies have helped in promoting integrated care, there are issues that were ignored because not all stakeholders were involved (Jabbour 2012). For instance, there is still a lack of the coordination between diverse healthcare providers based on actual forces in a healthcare setting (Blythe & Buchan 2016).
When caring for the patient, it was important to incorporate 6C’s of care to deliver excellent service (Jovin et al. 2015). Care, commitment and compassion were critical in ensuring that the patient’s needs were met by the medical staff and effective communication helped in understanding the condition of the patient and progress made during the process of medication. Thus, regarding Janes case, 6Cs of care were incorporated to improve her critical state.
Health Promotion and Patient Empowerment
Nevertheless, numerous research works demonstrate that the efficiency of health promotions and patient empowerment strategies applied to patients who have experienced an ischemic stroke precondition the overall success of the treatment (Bhalla & Birns 2015). For this reason, Jane was offered a specific plan of actions designed to ensure elimination of the negative impact of stroke on her body.
First of all, she was educated about the importance of lifestyle modification and its role in reducing vascular risk (Bhalla & Birns 2015). Regarding the patients hypertension, antihypertensive drug therapy to decrease the average level of her blood pressure was prescribed (Aslani et al. 2016). Additionally, Jane was provided with the diet rich in vegetables and fruits to minimise the risk of thrombosis and improve her dietary habits (Sit et al. 2016). Moreover, she was engaged in regular aerobic physical activity focused on the improvement of her cardiovascular system and overall rehabilitation. This set of measures contributed to the enhancement of treatment outcomes and Janes ability to continue working and communicating with her close friends and family.
Conclusion
Ischemic stroke is currently one of the leading causes of death and disability in the United Kingdom. It is estimated that 152,000 cases strokes are reported in the country every year. The problem is more common among African-Caribbean people than it is among the whites. However, it does not mean that the rest of the population is safe. The condition can affect anybody, especially those with poor lifestyle and those in abusive relationships or highly stressing careers.
Studies suggest that ischemic stroke is currently one of the leading causes of disabilities among senior adults in the country. It is also one of the top causes of deaths in the country, especially among the elderly in the United Kingdom and around the world. In the case study, it was evident that the patient did not know that she had an ischemic stroke. It means that the level of awareness of the disease among the people of the country, especially the elderly, is low. For those who are already with the condition, they should be helped to overcome their state. The following are the recommendations made based on this case study:
- Nursing and Midwifery Council should work with various government agencies and non-governmental organisation to sensitive the public about ischemic stroke. They need to be informed or reminded about the causes of the condition, the need to lead a responsible lifestyle, and importance of early diagnosis in case one suspects that he or she has first symptoms of the health problem.
- It is important to equip nurses when it comes to handling ischemic stroke patients, especially those who are emotionally unstable. Although the team was able to help the patient, it was not easy managing her emotional instability. For this reason, it might be helpful to invite psychotherapists to consult patients with the disease.
- When handling patients who are having this condition, nurses should always be considerate and able to understand that some of their abnormal behaviours are because of the intense pain and mental impairment caused by the issue.
Reference List
Acton, Q 2012, Nucleoside reverse transcriptase inhibitors: advances in research and application, Springer, London.
Ahn, S, Kim, J, Kim, D, Choo, S, Lee, H & Kim, H 2013, ‘Interaction between sleep-disordered breathing and acute ischemic stroke’, Journal of Clinical Neurology, vol. 9, no. 1, pp. 9-13.
Aslani, Z, Alimohammadi, N, Taleghani, F & Khorasani, P 2016, ‘Nurses’ empowerment in self-care education to stroke patients: an action research study’, International Journal of Commonly Based Nursing Midwifery, vol. 4, no.4, pp. 329-338.
Barrett, K & Meschia, J 2013, Stroke, John Wiley & Sons, New York, NY.
Berkhemer, O, Fransen, P, Beumer, D, Berg, L, Lingsma, H, Yoo, A & Schonewille, W 2015, ‘A randomized trial of intra-arterial treatment for acute ischemic stroke’, The New England Journal of Medicine, vol. 372, no. 1, pp. 11-20.
Bhalla, A & Birns, J 2015, Management of post-stroke complications, Springer, Cham.
Bhatnagar, P, Wickramasinghe, K, Williams, J Rayner, M & Townsend, N 2015, ‘The epidemiology of cardiovascular disease in the UK 2014’, British Journal of Sports Medicine, vol. 10, no. 2, pp. 34-49.
Blythe, A & Buchan, J 2016, Essential primary care, Wiley Blackwell, Hoboken, NJ.
Campbell, B, Mitchell, P, Kleinig, T, Dewey, H, Churilov, L, Yassi, N & Yan, B 2015, ‘Endovascular therapy for ischemic stroke with perfusion-imaging selection’, The New England Journal of Medicine, vol. 372, no. 1, pp. 1019-1030.
Chang, C 2014, Neurocritical care, Elsevier, Philadelphia, PA.
Ciccone, A, Valvassori, L, Nichelatti, M, Sgoifo, A, Ponzio, M, Sterzi, R & Boccardi, E 2013, ‘Endovascular treatment for acute ischemic stroke’, The New England Journal of Medicine, vol. 368, no. 1, pp. 904-913.
Davies, M 2012, Antenatal consults: a guide for neonatologists and paediatricians, Elsevier, London.
Doeppner, T & Hermann, M 2016, Stem cells and progenitor cells in ischemic stroke – fashion or future, Frontiers Media, Cape Town.
Fleisher, L 2013, Evidence-based practice of anesthesiology, Elsevier, Philadelphia, PA.
Goyal, M, Demchuk, A, Menon, B, Eesa, M, Rempel, J, Thornton, J & Roy, D 2015, ‘Randomized assessment of rapid endovascular treatment of ischemic stroke’, The New England Journal of Medicine, vol. 372, no. 1, pp. 1019-1030.
Jabbour, M 2012, Neurovascular surgical techniques, Jaypee Medical, New Delhi.
Jauch, E, Cucchiara, B, Adeoye, O, Meurer, W, Brice, J, Chan, Y, Gentile, N & Hazinski, M 2010, Part 11: adult stroke 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Web.
Jovin, T, Chamorro, A, Cobo, E, Miquel, M, Molina, C, Rovira, A & Román, L 2015, ‘Thrombectomy within 8 hours after symptom onset in ischemic stroke’, The New England Journal of Medicine, vol. 372, no. 1, pp. 1019-1030.
Kernan, W, Viscoli, C, Furie, K, Young, L, Inzucchi, S, Gorman, M & Guarino, P 2016, ‘Pioglitazone after ischemic stroke or transient ischemic attack’, The New England Journal of Medicine, vol. 374, no. 2, pp. 1321-1331.
Lapchak, A & Zhang, J 2017, Neuroprotective therapy for stroke and ischemic disease, Springer, Cham.
Lee, S 2017, Stroke revisited: diagnosis and treatment of ischemic stroke, Springer, Singapore.
Lohse, K, Lang, C & Boyd, L 2014, ‘Is better? Using metadata to explore dose–response relationships in stroke rehabilitation’, American Stroke Association, vol. 45, no. 1, pp. 2053-2058.
National Collaborating Centre for Chronic Conditions 2008, National clinical guideline for diagnosis and initial management of acute stroke and transient ischaemic attack (TIA), Royal College for Chronic Conditions, London.
NMC 2015, The code. Professional standards of practice and behaviour for nurses and midwives. Web.
Ovbiagele, B & Turan, N 2016, Ischemic stroke therapeutics: a comprehensive guide, Springer, Cham.
Palmer, K, Brown, I & Hobson, J 2013, Fitness for work: the medical aspects, Cengage, New York, NY.
Peschillo, S 2016, Brain ischemic stroke – from diagnosis to treatment, Bentham Science Publishers, Sharjah.
Roedde, G 2012, A doctor’s quest: the struggle for mother and child health around the globe, Dundurn Press, Toronto.
Saver, J, Goyal, M, Lugt, A, Menon, B, Majoie, C, Dippel, D & Campbell, B 2016, ‘Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis’, The JAMA. Journals, vol. 316, no. 12, pp. 1279-1289.
Sit, J, Chair, S, Choi,K, Chan, C, Lee, D, Chan, A, Cheung, J, Tang, S, Chan, P & Piliae, R 2016, ‘Do empowered stroke patients perform better at self-management and functional recovery after a stroke? A randomized controlled trial’, Clinical Interventions in Aging, vol. 11, pp. 1441-1450.
Siotto, M, Aprile, I, Simonelli, I, Pazzaglia, C, Ventriglia, M, Santoro, M, Imbimbo, I, Squitti, R & Padua, L 2017, ‘An exploratory study of BDNF and oxidative stress marker alterations in subacute and chronic stroke patients affected by neuropathic pain’, Journal of Neural Transmission, vol. 124, no. 12, pp. 1557–1566.
Wardlaw, J, Murray, V, Berge, E, del Zoppoe, G, Sandercock, P, Lindley, R & Cohen, G 2012, ‘Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis’, Lancet, vol. 379, no. 9834, pp. 2364-2372.
Williams, J, Perry, L & Watkins, C 2013, Acute stroke nursing, John Wiley & Sons, New York, NY.