Introduction
Overview
Hand hygiene might simply be too common that people usually take it for granted. They have been washing their hands from childhood that the act becomes a routine without extra effort. However, there is a proper way to maintain hand hygiene. Several health benefits can be derived from the proper practice of hand hygiene. Numerous hospital-based research proved that non-compliance with hand hygiene practices (HPP) is linked to infections in the health care sector, escalation of multi-resistant microorganisms, and a critical cause in disease outbreaks (Hand Hygiene, 2009).
It has become an important issue among the healthcare provider, medical professionals, nursing profession, researchers, academicians, the government and private institutions that it has gained a specific advocacy. It can be found that improper hand hygiene is practiced not only among the poor and low income people but also the wealthy who have not properly informed on its necessity. Hand hygiene is essential in hospital setting, in perioperative environment, in the household and public places. Reduction in the healthcare acquired infections (HCAI) is accorded great attention in order to enhance the safety and quality of the health services (Hand Hygiene Project, 2009). As research revealed, health care-associated infections (HCAIs) is greatly reduced when there is a marked improvement in HPP implementation (Hand Hygiene, 2009)
This paper will discuss the importance of hand hygiene, the proper hand sanitation, institutional move to inculcate the proper practice, and the global outlook and development of this aspect of health maintenance.
Definition
According to the Centers for Disease Control and Prevention, hand hygiene refers to the “routine hand washing, antiseptic hand wash, antiseptic hand rub, or surgical hand antisepsis” (Hand Hygiene 2009).
Scope of the Problem
Infection can be transmitted through the hands. Thus, cleanliness of the hands is imperative everywhere especially in the hospital setting where infectious diseases can be transmitted from person to person easily. In the pediatric section, transmission of infection is imperative with repeated contact among patients, visitors, healthcare providers, environment, etc. (Improving Hand Hygiene, 2009). Despite such necessity for hand hygiene practice (HPP), there is a very low compliance as shown by existing literatures (Creedon, 2005, as cited in Improving Hand Hygiene, 2009). The review conducted by Pittet (2001, as cited in Improving Hand Hygiene, 2009) revealed that compliance with HPP has a rate of 16 to 60 percent in non-ICU units while ICU compliance settings has 28 to 81 percent compliance. The Children’s Hospital at Westmead (CHW) in Australia, audited in 2006, had a low 23 percent compliance as against the other institutions that prompted it to increase the awareness of the individuals concerned (Improving Hand Hygiene, 2009).
Chart I
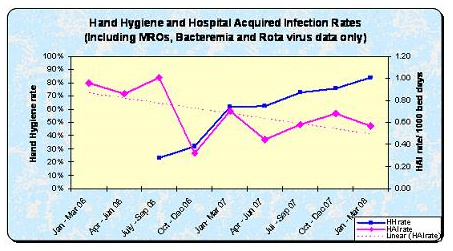
The above chart shows the result of regular monitoring of hospital-acquired infections (HAIs) concerning Rotavirus, MROs, and Bacteremia and the effectiveness of the HPP intervention (Improving Hand Hygiene, 2009). The data showing a marked decline in HAIs when the HPP increased is relevant for hospital staff in their awareness of keeping patients safe (Improving Hand Hygiene, 2009).
The internal audit conducted (in 2008) in some wards in McGill University Health Centre (MUHC) revealed that only one in every four physicians wash their hand’s in-between patients or before attending to the next patient (Gazette, 2009). The nurses had a higher HPP compliance of 40 to 50 percent (Gazette, 2009) but still low by established standards. Such compliance rate by the nurses is blamed for the proliferation of “germs and deadly infections in hospitals” (Gazette, 2009, para. 2). The 2008 audit is not far higher than the 2001 audit that had less than one in four physicians and below 40 percent for nurses that undertake HPP precautions (Gazette, 2009)
These figures are not quite satisfactory since those audited should be the advocates of hand hygiene. The low turnout would only indicate that on the rest of the rating, the germs and bacteria would be thriving and spread by health care providers and professionals.
It was reported that more than 1.4 million people around the world suffer from infections obtained in hospitals (Tikhomirov, 1987; Vincent 2003, as cited in Improved Hand Hygiene, 2007). The World Health Organization mentioned that HAI affects not only developing but also developed countries (Improved Hand Hygiene, 2007). Developed countries have 5 to 10 percent of patients who acquire infections not only once while in the critical care setting, 15 to 40 percent of patients are affected (Lazzari, 2004, as cited in Improved Hand Hygiene, 2007). It is believed that the infection can reach more than 20 percent in settings with poor resources (Pittet, 2005, as cited in Improved Hand Hygiene, 2007).
The United States of America has one hospital infection for every 136 patients that becomes critically ill (Starfield, 2000, as cited in Improved Hand Hygiene, 2007) that is commensurate to 2 million persons in a year with equivalent spending of US$ 4.5 to 5.7 billion and around 90,000 deaths (Improved Hand Hygiene, 2007). The United Kingdom, on the other hand, has 100,000 HAI cases with an equivalent cost of £1 billion and 5,000 deaths in a year (Mayor, 2000, as cited in Improved Hand Hygiene, 2007). Mexico has around 450,000 infections that resulted in 35 deaths for every 100,000 neonatal cases and fatality of 4 to 56 percent (Zaidi, 2005, as cited in Improved Hand Hygiene, 2007). Australia has around 150,000 HCAI cases with around 7,000 resulting in death in a year (Hand Hygiene Project, 2009).
Thesis Statement
The government and health institutions should devise programs and allocate resources to increase hand hygiene practice compliance and reduce the risk of infections and contagion among patients, health care providers, personnel, and visitors of patients.
Discussion
Infectious Diseases
Infection refers to the process wherein germs penetrate a vulnerable part of the body and thereafter reproduce themselves causing a disease (Infection, 2005). It is also said to be a reaction of the body to the existence of microorganisms or the invasion of the tissue by microorganisms (Neligan, n.d.). The existence of bacteria in circulating blood is referred to as Bacteremia (Neligan, n.d.). Sepsis, on the other hand, is the “systemic inflammatory response to infection” accompanied by the following conditions: a) dysfunction, hypoperfusion, or hypotension (Sepsis [SIRS] associated with organ dysfunction), b) induced hypotension with perfusion abnormalities (Refractory [Septic] Shock/SIRS Shock), and c) altered organ function that intervention is necessary for homeostasis (Multiple Organ Dysfunction Syndrome [MODS]) (Neligan, n.d.).
Based on the brief description of infection, its effects upon the body cannot be simply ignored. Without delving into the technicalities of the definitions, germs, bacteria, and microorganisms can enter the body through person-to-person contact. While transference can happen airborne, physical contact is the primary cause of infection.
WHO Policies
As a global organization representing the health interest of the member-states and other countries, the World Health Organization (WHO) is one of the primary institutions that give prime importance to hand hygiene practice to avoid infection and death-causing diseases.
WHO provided these approaches to be followed by the member-states:
- promotion of hand hygiene by facility be given priority; this entails strong leadership, administrative support, and financial allocation,
- adoption from the regional level, country to the facility of the WHO Guidelines on Hand Hygiene in Health Care nine recommendations with emphasis on the multidisciplinary and multimodal approaches that include readily available alcohol-based hand sanitizers for patients, provision of continuous water supply, awareness training on hand hygiene for health workers, posting hand hygiene reminders in the area, measuring HHP compliance and providing feedback, and
- use WHO Recommended Hand Antisepsis Formulation: Guide to Local Production when alcohol-based sanitizers are unavailable or expensive (Improved Hand Hygiene, 2007).
WHO likewise exhorts concerned member-states to involve the patient and the family in the effort to avoid infection by
- increasing the awareness of patients, their families, and visitors to the risks posed by improper hand hygiene practices,
- formulating informative materials for patients and families,
- motivate staff to clean their hands in front of patients before touching them and invite the latter to do the same if culturally permissible, and d) inform the patients on the proper hand hygiene technique (Improved Hand Hygiene, 2007).
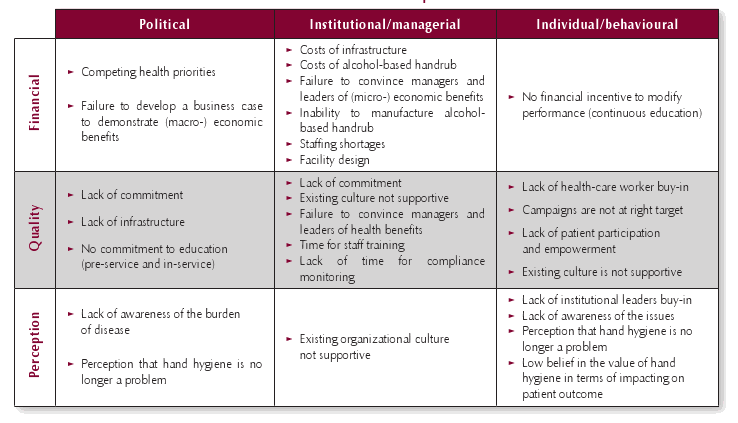
The table below provides the list of identified barriers to the implementation of hand hygiene practices. Successful implementation would involve not only the healthcare providers but also the policymakers of the organization, its leaders, and managers (Improved Hand Hygiene, 2007).
Hand Hygiene Techniques and Approaches
Hand hygiene is an effective practice that remarkably lessens the presence of pathogens on the hands and is regarded as the principal approach in risk reduction associated with microorganisms transmission between patients and healthcare workers (Hand Hygiene, 2009). It does not concern only the patients and their families but also the healthcare providers that they interact with every day. Health care-acquired infection (HCAI) affects the healthcare worker and the capability of the system to provide care to the patients (Hand Hygiene Project, 2009). Thus, the Hand Hygiene Project is launched by the Victorian Quality Council (VQC) to provide training and resources to hospitals, as well as promotion of sustained appropriate culture and attitude towards hand hygiene (Hand Hygiene Project, 2009). The systems in place and the linking of infection control teams and managers with the programs will ensure the sustainability of the project (Hand Hygiene Project, 2009). The strategy of the project includes a proposal to use alcohol-chlorhexidine hand hygiene product, inculcate HPP among the healthcare providers, continuous promotion of HPP through varied communication and advertising devices, effective participation and feedback mechanism for individuals and organization, engagement of institutional leaders, and accumulation and feedback for outcome indicators (e.g. product usage in liters/1000 bed days/month, rates of nosocomial infection, and rates of compliance) (Hand Hygiene Project, 2009).
Conclusion
This paper seeks to explore the status of hand hygiene practices and the programs and strategies implemented by institutions to reduce the risk of infection in the healthcare sector. Data gathered from several studies and internal audits showed that HPP compliance even among the healthcare professionals and carers is remarkably low that has been associated with an outbreak of diseases. Hand hygiene is a highly recommended primary approach in reducing the risk of contagion. Thus, hospitals, health institutions, and the WHO recommend strategies and approaches that would effectively lessen the transference of germs and bacteria from person to person.
Despite efforts in one institution, an internal audit revealed no marked increase in HPP compliance in physicians and nurses (2001 audit as against the 2008 audit). The wisdom manifested by this study is the difficulty of sustaining the practice or even improving it despite the seeming simplicity of this approach. It can be surmised that the difficulty in compliance is due to the tasks a doctor has to undertake from patient to patient that in-between hand washing is not remembered. But it is this in-between routine that is aimed by HPP leaders and advocates so that disease outbreaks can be averted.
In conclusion, HPP compliance still needs improvement. Institutional culture must be transformed so that the healthcare providers will be able to imbibe the proper hand hygiene practices. Constant implementation and performance of HPP will make it a routine task that becomes part of the activities of the healthcare providers that needs no more conscious effort in order to implement.
References
Gazette (Montreal). (2009). 3 out of 4 doctors skip hand washing. canada.com. CanWest MediaWorks Publications Inc. Web.
Hand Hygiene. (2009). Centers for Disease Control and Prevention. Department of Health and Human Services. Web.
Hand Hygiene Project. (2009). The Victorian Quality Council. Safety and Quality in Health. Victorian Government Health Information. Web.
Infection. (2005). Chemocare.com. The Cleveland Clinic Foundation. Cleveland Clinic Cancer Center. Web.
Improved Hand Hygiene to Prevent Health Care-Associated Infections. (2007) Patient Safety Solutions, 1(9). World Health Organization. Google docs. Web.
Improving Hand Hygiene – Difficult, but not Impossible. (2009). Australian Resource Centre for Healthcare Innovations (ARCHI). Web.
Neligan, P. (n.d.). What is Sepsis? SIRS, Septic Shock… Critical Care Medicine Tutorials. Web.