Background
This scientific paper explores the respiratory disease asthma. In the modern world, many people face this disease, which is why it is necessary to study this ailment. Therefore, this work focuses on such aspects of the disease as description, symptoms, people at risk, and treatment. Moreover, this study examines preventive measures that can contribute to reducing the dynamics of the occurrence of the disease among the population.
Description of the Disease
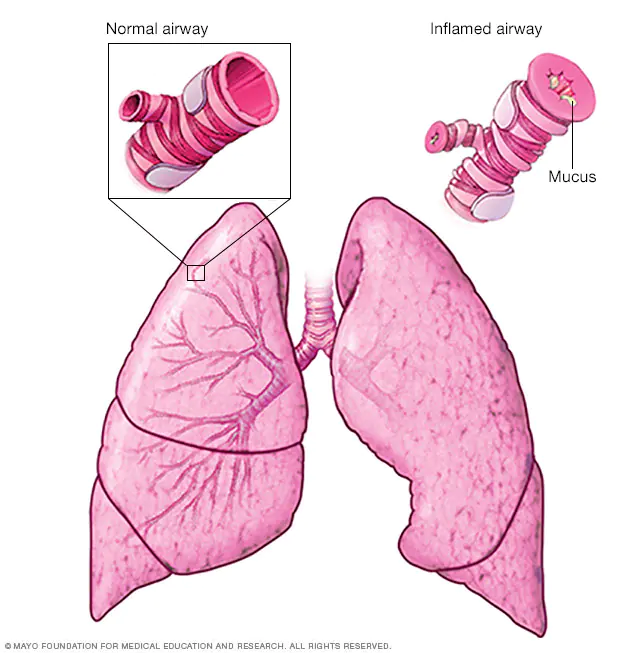
First of all, before discussing measures to prevent an increase in the case of the disease, it is necessary to understand the nature of the disease. Research shows that “asthma is a serious disease that affects about 25 million Americans and causes nearly 1.6 million emergency room visits every year” (Ratini, 2021, para. 2). As indicated in the sources, “chronic inflammatory disorder of the airways with bronchial hyper-responsiveness to a variety of stimuli and variable airflow obstruction that is often reversible either spontaneously or with treatment” (Fajt et al., 2017). In other words, this disease causes swelling and narrowing of the respiratory tract and the possible occurrence of excessive mucus on them (Figure 1). As a result of this process, there is difficulty breathing, coughing, and a slight whistle when inhaling and exhaling.
The peculiarity of this disease is that all people experience it in different ways. For someone, it may be asymptomatic, and for someone, it may have severe consequences that complicate everyday life. An asthma attack can become a particular danger for asthma patients. An unfavorable prognosis is that such a respiratory disease as asthma is not fully treated, but it can be controlled and put into remission. This can be done with the help of constant monitoring of the doctor and following all necessary instructions.
Depending on the symptoms, doctors distinguish several types of asthma. The first type is called mild intermittent asthma, which is characterized by rare symptoms and a low number of asthma attacks. The second involves the daily manifestation of symptoms that interfere with daily activities and is called moderate persistent asthma. The latter, severe persistent asthma, is characterized by even more frequent manifestations of asthma, which places severe restrictions on the patient’s vital activity and capabilities.
Therefore, based on the above qualifications, more detailed types of respiratory asthma disease are distinguished. This may be adult-onset asthma, which manifests itself in people under forty years of age, status asthmaticus, which continues to affect the human body, even with treatment and asthma in children. This type of disease varies from child to child and has such notable symptoms as cough, heavy breathing, and weakness.
Another common type of asthma is allergic asthma. It is emphasized that “the unique role of reactive oxygen species (ROS) had been identified as the main reason for this respiratory inflammation” (Qu, 2017, p. 32). The pathogens of this species include dust or pollen of flowers and plants. Moreover, there is also nonallergic asthma, which occurs at high or low temperatures, severe stress, or other respiratory diseases. A particular type is eosinophilic asthma, which is characterized by a high level of blood cells, and most often, people aged 35 and 50 years old have it (Bakakos et al., 2019). In addition, there is aspirin-induced asthma caused by taking aspirin, and such consequences as running nose, sneezing, and a cough.
Contraction of the Disease
The next aspect that requires detailed consideration is the ways of infection with the respiratory disease asthma. Thus, the aspects that can provoke asthma are external and internal factors before a person is born or a genetic predisposition. A particularly interesting impact factor is race, where African American or Puerto Rican people are more prone to the disease. Moreover, boys are more predisposed to the respiratory disease under study than girls. However, at an older age, this circumstance changes, and women suffer from asthma more often (Naeem & Silveyra, 2019). Moreover, asthma is also affected by various other diseases such as lung infections, obesity, and allergies. All groups of the population are exposed to the disease, regardless of age, gender, and social status.
Affect on the Patient
There are three main symptoms of the respiratory disease asthma. The first is the blocking of the airways, which manifests itself in the contraction of the muscles of the airways when breathing, which makes it difficult for air to pass. Next, there is inflammation, which is characterized by swelling of the bronchial tubes, which can significantly affect the work of the lungs. The last main symptom of asthma is the inability of the respiratory tract to function correctly. This affects the fact that the respiratory system is very susceptible to reactions to external and internal stimuli and narrows when interacting with them.
Other, more common symptoms that are most common in asthma patients are coughing, whistling while breathing, lack of air when breathing, pain or pressure in the chest. In addition, all these symptoms affect sleep disorders due to breathing difficulties and a general barrier to the performance of vital functions. It is worth noting that all people have asthma characterized by different symptoms for each person. Moreover, they can change over time, which is predominantly caused by asthma attacks that leave a mark on human health.
Another effect of asthma on people is that some symptoms may not manifest for a long time, while others may experience them constantly. Another exciting factor is the manifestation of asthmatic features only during physical exertion or in combination with other infectious diseases. With the help of medical examination, timely detection of asthma symptoms is critically necessary since their detection can significantly facilitate the patient’s life.
Treatment
As already mentioned, asthma is not a type of respiratory disease that can be cured entirely. At the same time, there are ways that can significantly ease the course of the disease or even put it into remission. One of the methods that are used for each patient is the use of special inhalers. The active effect of this drug is the effect of reducing swelling in the lungs and reducing mucus secretion. One of the most effective is inhaled corticosteroids, which are used throughout the treatment. The number of times of use and the time frame is determined by the patient’s attending physician.
Among inhaled corticosteroids, one can highlight beclomethasone, budesonide, and leukotriene modifiers. The latter block leukotrienes, which cause asthma attacks in patients. There are also long-acting beta-agonists that reduce tension in the muscles of the respiratory tract, ciclesonide (Alvesco), mometasone (Asmanex), and salmeterol (Serevent). Another subspecies are combined inhalers, which provide the patient with corticosteroid and a long-acting beta-agonist together when inhaling. Among them, such drugs as fluticasone and salmeterol (Advair Diskus, AirDuo Respiclick) or, for example, mometasone and formoterol (Dulera) are produced. In addition to inhalers, there are oral and intravenous corticosteroids, which include Methylprednisolone (Medrol), prednisolone (Flo-pred, Orapred, Pediapred, Prelone), and Prednisone (Deltasone). They are also often used together in inhalers and are used to reduce swelling and infection in the respiratory tract. Non-drug treatment, biological, is used in cases where medications do not have exceptional efficacy. Examples of such drugs are bevacizumab (Fastener), mepolizumab (Nucala), and reslizumab (Cinqair).
Prevention of the Disease
Medications are the primary way to treat respiratory asthma disease. However, there are some ways that will help control the disease and reduce cases of asthma attacks. These measures include avoiding the pathogens of asthma, if it is, for example, allergic, constant physical stress, maintaining a healthy lifestyle. Moreover, constant breathing exercises are recommended to alleviate asthma symptoms. This may also include activities such as yoga, acupuncture, or supplements like vitamin C. It is worth remembering that all these actions are performed simultaneously with taking the necessary medications prescribed to the patient by the attending physician.
Asthma Attack
The part that aroused the most significant interest in conducting this study was the attack of asthma as the most severe and dangerous manifestation of respiratory disease. This attack is characterized by a strong tone of the muscles of the respiratory tract, which causes their tightening and difficulty breathing. Thus, this process is called bronchospasm and can have severe consequences for human health. In addition, in addition to the narrowing of the airways, additional mucus is formed on them than usual. In addition to the difficulty of breathing, patients also experience wheezing, coughing, and trouble with regular activities. In addition to these symptoms, chest pain, a feeling of panic and anxiety, pale skin, and blue lips and fingertips may also appear.
Based on the above, it is critically important to note that asthma treatment should be applied in a timely and continuous manner to avoid the manifestation of such dangerous incidents. Without the use of drugs such as asthma inhalers or bronchodilators, people can suffer severe consequences for their health. Thus, in such cases, an urgent appeal to the ambulance is necessary for further provision of medical services and mitigation of symptoms.
To prevent the manifestation of an asthma attack, several rules must be followed to avoid negative consequences. They include the removal of asthma triggers, following the instructions of the attending physician on taking medications, and constant monitoring of the patient’s well-being (Gautier & Charpin, 2017). Coupled with the study of all aspects of the disease, it will help to understand the body better and can also reduce the number of attacks. It is also helpful in gaining knowledge about what measures should be taken when dangerous incidents of illness occur. It is worth emphasizing that such data and emergency care skills should also be known by all the close people around the patient.
Thus, this scientific work considered such a respiratory disease as asthma. First of all, the description of the disease was investigated and what is its mechanism. Further, the symptoms of asthma and what measures can be applied to reduce its impact were analyzed. Interest was aroused by asthma attacks, which were considered as useful additional information at the end of the work. In conclusion, it is essential to note that acquiring this knowledge and spreading awareness about them among the population will help significantly improve the dynamics of the spread of the disease and the occurrence of incidents dangerous to human health.
References
Ratini, M. (2021). Asthma. WebMD. Web.
Fajt, M. L., & Wenzel, S. E. (2017). Development of new therapies for severe asthma.Allergy, Asthma & Immunology Research, 9(1), 3-14. Web.
Qu, J., Li, Y., Zhong, W., Gao, P., & Hu, C. (2017). Recent developments in the role of reactive oxygen species in allergic asthma.Journal of Thoracic Disease, 9(1), 32-43. Web.
Bakakos, A., Loukides, S., & Bakakos, P. (2019). Severe eosinophilic asthma. Journal of Clinical Medicine, 8(9), 1375. Web.
Naeem, A., & Silveyra, P. (2019). Sex differences in paediatric and adult asthma. European Medical Journal (Chelmsford, England), 4(2), 27.
Gautier, C., & Charpin, D. (2017). Environmental triggers and avoidance in the management of asthma.Journal of Asthma and Allergy, 10, 47. Web.
Asthma. (n.d.). Mayo Clinic. Web.