Introduction
Congestive heart failure is an acute disease connected with contestations in the heart’s ventricular chambers, which narrow them and prevent blood from healthy ejection in the artery. It occurs in all populations but is especially dangerous for those with weak hearts, such as elders or people with excessive weight. Those with COVID-19 in their medical history are more vulnerable, too, due to their weak lungs and increased heart load. While the diseases can be treated by breathing facilitation and medication in a hospital, they do not eliminate the disease’s cause, which should be treated separately.
Congestive Heart Failure: An Overview
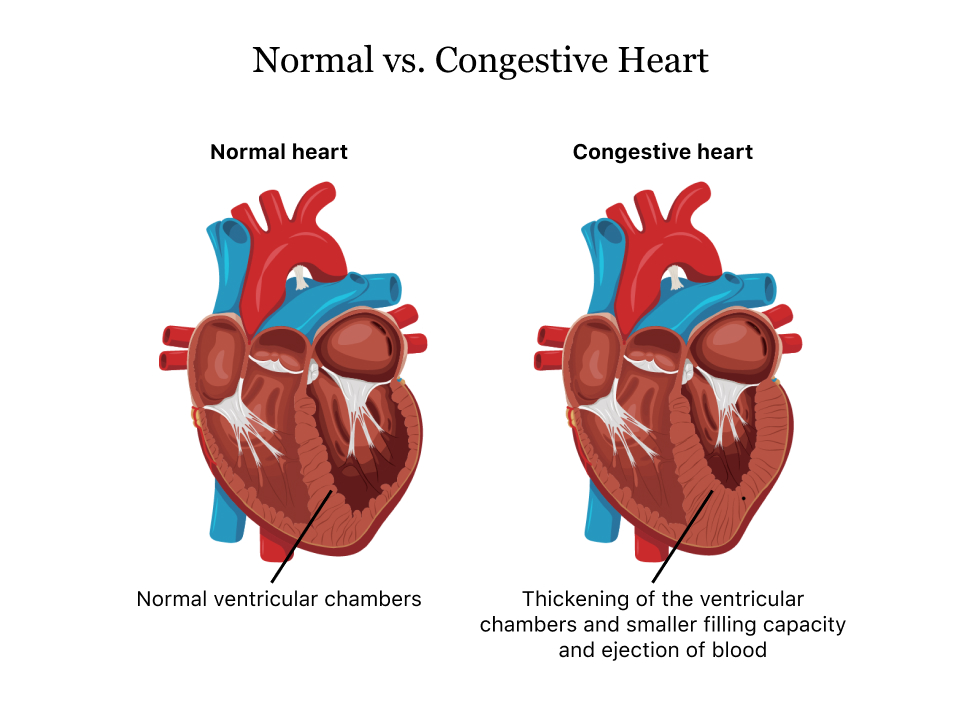
Congestive heart failure is one of the common types of heart disease, with high mortality and risks among all populations, especially the elderly. It is the most common cause of hospitalization of patients 65 or older, and over 1 million hospitalizations occur yearly (Scott & Winters, 2015). While the disease is acute, its development is rapid, and immediate hospitalization is necessary; it is a complication of various heart problems, such as myocardial dysfunction (La Franca et al., 2020). The dysfunction leads to liquid retention in heart tissue, which thickens, narrows ventricular chambers, and prevents blood from being ejected, as shown in Figure 1 (Llamas, 2023). As the heart becomes more and more congestive, the risk of dysfunction grows, as there can be a moment when it will be unable to initiate blood circulation and fail. As the organism cannot function without a beating heart, immediate hospitalization, and medication are necessary to save the patient’s life.
Congestive heart failure is a serious problem, as, despite various treatment types, they deal only with the consequences to save a patient’s life and not remove the failure cause. There are various medication methods: ventilation is used to ensure safe patient breathing and oxygenation. Medicaments like diuretics, beta-blockers, and angiotensin-converting enzyme inhibitors are used to reduce blood pressure and remove excess liquid from the congestive heart (Scott & Winters, 2015). Coronavirus disease can increase the risk and severity of heart failure, and the failure increases the risk of severe COVID-19 complications (Standl and Schnell, 2021). While heart failure victims can be saved in most cases, they require additional treatment to improve heart function and prevent further failures.
COVID-19 Effects on Heart Failure
There are many facts that coronavirus disease and heart failure risk are interconnected: the whole picture one can see in Figure 2. People who suffered from COVID-19 have more risk of heart failure in similar conditions compared to those who did not. Myocardial injury is a common consequence of the disease, and as mentioned, it is a prerequisite of congestive heart failure (Standl and Schnell, 2021). Lung impairment, which can also be a long-term consequence, means that the heart must work more to provide the same amount of oxygen to the organism. In case of any congestion, the chance of failure will grow as heart contractions must be stronger and more frequent.
In addition, patients who experience heart failure have a greater chance of getting COVID-19. Their mortality also increases highly, up to two-fold, compared to those with no heart failures (Standl and Schnell, 2021). The reason is that a weaker heart, with various dysfunctions, cannot pump blood efficiently to provide enough oxygen to the organism. Oxygenation is crucial when lungs are damaged by COVID-19; thus, the chance of complications or even death increases. Hypertension of lung arteries, another common consequence, is detrimental for COVID-19 patients, too, increasing the chances of acute cardiovascular events (Standl and Schnell, 2021). Therefore, COVID-19 complications are much more common in patients with heart failure.
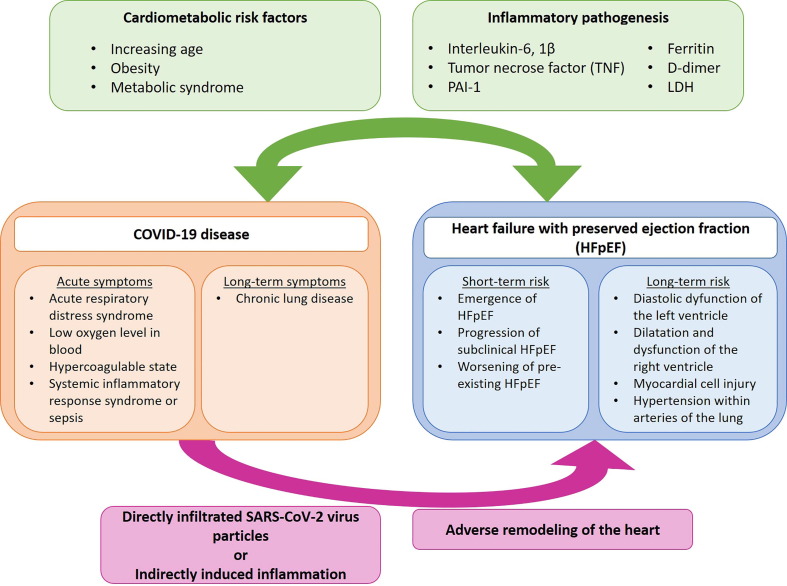
Therefore, people with COVID-19, or those with it in their medical history, should be watched if they have no severe heart problems, as the risk of heart failure increases. Their hearts and circulatory systems are weaker, while damaged lungs require that they should beat faster and stronger, thus increasing the chance of failure in case of congestion. Conversely, people who suffer heart failure are more vulnerable to COVID-19. Their hearts are weaker, and they are vulnerable to cardiovascular complications and suffer from a lack of oxygenation (Standl & Schnell, 2021). The respiratory and cardiovascular systems of the organism are deeply interconnected, both serving the purpose of the body’s oxygen supply: COVID-19 damages the former, and heart failure impairs the latter. If one component of the system becomes weakened by one of them, another one is required to work more, becoming much more vulnerable to another disease.
Congestive Heart Failure Treatment and Intervention
The most common way to treat patients with congestive heart failure is the combination of non-invasive ventilation and pharmacological treatment, which enables a physician to return the patient’s heart functioning. Non-invasive positive-pressure ventilation improves oxygenation and breathing, which is crucial when a patient’s heart is dysfunctional, and decreases the blood pressure, reducing venous preload. From the pharmacology, angiotensin-converting enzyme (ACE) inhibitors, nitrates, and diuretics are primarily used (Scott & Winters, 2015). Each of them acts on various aspects of the heart and circulatory system, and together, they reduce the consequences of heart failure, enabling a patient to recover.
Many challenges are present in congestive heart treatment, as they usually cannot solve the cause of the problem. Nitroglycerine and other beta-blockers reduce venous and arterial dilation and decrease tension in the heart chambers (Scott & Winters, 2015). ACE inhibitors, such as enalaprilat, lower the blood afterload, decreasing the blood pressure, and can be administered with beta-blockers. Diuretics, such as furosemide, help decrease the liquid level in heart tissues, easing the congestion, but they should be issued after beta blockers and with renal perfusion. Beta-blockers, ACE inhibitors, diuretics, and positive-pressure ventilation, used together, can decrease the heart load and congestion, helping a patient recover. However, the initial causes of heart failure should be elucidated after that and treated separately; in other cases, the failure can be repeated.
Summary and Conclusion
Congestive heart failure is a serious acute disease, that is prevalent among the elderly population, has a high mortality rate, and requires quick hospitalization and immediate treatment. While the disease starts abruptly, it is always preceded by problems such as excessive weight, increased arterial pressure, or problems with myocardial tissue. Its mechanism is based on the liquid retention in heart tissue, which leads to congestion, narrowing chambers, and preventing normal blood flow via vessels. As respiratory and cardiovascular systems are interconnected and serve the same purpose of body oxygenation, COVID-19, which injures the lungs, greatly increases the risk and severity of heart failure. Congestive heart failure is treated by positive-pressure ventilation and administering beta-blockers, ACE inhibitors, and diuretics, which decrease arterial pressure and contestations. While they enable physicians to save a patient’s life, the causes of heart failure should be elucidated and treated separately to eliminate the chance of a new failure.
References
La Franca, E., Manno, G., Ajello, L., Di Gesaro, G., Minà, C., Visconti, C., Bellavia, D., Falletta, C., Romano, G., Dell’Oglio, S., Licata, P., Caronia, A., Gallo, M., & Clemenza, F. (2020). Physiopathology and diagnosis of congestive heart failure: Consolidated certainties and new perspectives. Current Problems in Cardiology, 100691. Web.
Llamas, M. (2023). Congestive heart failure | Types, symptoms, and treatment. Drugwatch.com. Web.
Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine Clinics of North America, 33(3), 553–562. Web.
Standl, E., & Schnell, O. (2021). Heart failure outcomes and Covid-19. Diabetes Research and Clinical Practice, 175, 108794. Web.