Background
Many people in the United States of America have diabetes, a chronic condition. According to the Centers for Disease Control and Prevention (CDC), as of February 2020, approximately 34.2 million Americans—about 10% of the population—had been diagnosed with diabetes (Shin et al., 2021). Type 2 diabetes, which accounts for nearly all cases, is primarily attributable to unhealthful lifestyle choices and environmental factors and is preventable and controllable (Shin et al., 2021). Heart disease, kidney failure, and blindness are some devastating outcomes that can result from diabetes, making it the sixth most prominent cause of mortality in the United States.
There is a critical need for efficient interventions to prevent and control diabetes due to the disease’s enormous toll on American health and prosperity. The funding request aims to address the problem of diabetes by supporting individuals at risk of developing the condition and educating those who have already been diagnosed (Shin et al., 2021). The proposal outlines a comprehensive plan to combat diabetes in neglected areas. The proposal aims to reduce diabetes rates and improve the quality of life for individuals with the disease.
Organizational Overview
The Health and Wellness Initiative (HWI) is a charitable group that aims to reduce the prevalence of diabetes and other chronic illnesses through education and advocacy. Since its inception in 2008, HWI has established a solid reputation for delivering high-quality health interventions and programs that address the root causes of chronic diseases (Shin et al., 2021). With a focus on marginalized regions that have a disproportionately high prevalence of diabetes, HWI’s strategy for combating the disease centers on expanding access to healthcare resources and information (Shin et al., 2021). HWI collaborates with healthcare professionals, community groups, and government officials to provide effective solutions.
HWI employs doctors, nurses, and health educators who are passionate about their mission to promote healthy behaviors and improve people’s health. HWI can effectively contact and connect with its target groups thanks to its partnerships with local hospitals, clinics, and community organizations (LaManna et al., 2019). HWI’s programs and treatments are designed to help individuals feel more confident in making positive changes to their health and lifestyle (LaManna et al., 2019). The ultimate objective is to build a society where people of all socioeconomic backgrounds have access to quality healthcare and can live long, healthy lives without the threat of developing chronic conditions, such as diabetes.
Experience
Health-First’s community-based intervention programs have been proven effective in combating chronic disease at its source. Improved health outcomes for program participants have resulted from our prior work in obesity, hypertension, and smoking cessation (Shin et al., 2021). We have effectively connected and engaged with our target demographics thanks to our solid ties with local community organizations, schools, and companies (Shin et al., 2021). We have the knowledge and background to successfully conduct a program to reduce the prevalence of Type 2 diabetes in persons who are already at risk.
Problem Statement
The prevalence of diabetes among American adults is high enough to warrant serious attention as a public health issue. Around 10% of the US population, or 34.2 million individuals, had been diagnosed with diabetes as of February 2020, according to the CDC (Wu & McGoogan, 2020). Another 33% of the population, or 88 million, had pre-diabetes (Shin et al., 2021). The most common kind of diabetes, known as type 2 diabetes, is a long-term condition that can be avoided in most people but has catastrophic consequences, including cardiovascular disease, stroke, blindness, renal failure, and limb loss.
Those with lower socioeconomic status, lower levels of education, and poorer incomes bear a disproportionate share of the diabetes burden, according to empirical studies. Disparities in healthcare availability, health-related behaviors, and environmental and social factors contribute to unequal health outcomes (Wu & McGoogan, 2020). Finding effective strategies that can be scaled up and available to people of all backgrounds and socioeconomic circumstances is a top priority (Shin et al., 2021). This funding proposal aims to outline a comprehensive plan that addresses the breadth and depth of the diabetes epidemic, with measurable positive effects on the lives of those who will benefit from it.
Methodologies for Addressing the Problem
This plan aims to improve the situation in several ways, including increasing access to healthcare, educating the public, and promoting healthier lifestyles. Diabetes, its risk factors, and preventative measures will be brought to the forefront of the public consciousness through community outreach and education efforts (LaManna et al., 2019). Minorities, low-income neighborhoods, and rural locations have a disproportionately high prevalence of diabetes; hence, these programs will focus on them (Macomb et al., 2020).
Public health campaigns, online tools, and community activities will all play a crucial role in spreading awareness about the programs. Lifestyle interventions will be implemented to promote healthy behaviors and minimize the risk of developing diabetes (Miller et al., 2020). The goal is to promote regular exercise, a balanced diet, and healthy weight maintenance. There is some evidence that group-based therapies, such as diabetes preventive programs, can help reduce the risk of Diabetes (LaManna et al., 2019). Continuous support and monitoring will be built into these programs to ensure they meet the intended audience’s needs.
Systemic changes in the healthcare industry will boost access to diabetes prevention, screening, and treatment. Priorities will include expanding access to diabetes screening and prevention programs, improving coordination between primary care physicians and specialists, and lowering the cost of medications and medical supplies (LaManna et al., 2019). Telehealth and other mobile health applications will also be implemented to enhance the quality of treatment provided to people with diabetes and their health outcomes.
Other potential approaches included expanding access to bariatric surgery for significantly overweight people, imposing a sugar tax to discourage excessive sugar intake, and requiring restaurants to label their food with nutritional information clearly. The DPP’s current participants were all eligible for the optional follow-up assessment. Follow-up was continued for a median of 5.7 years (IQR 5.5-5.8) with 2766 out of 3150 (88%) participants. (LaManna et al., 2019).
There were 910 people in the lifestyle group, 924 in the metformin group, and 932 in the initial placebo group (Shin et al., 2021). All three groups were offered group-implemented lifestyle intervention based on the successes of the DPP’s intensive lifestyle intervention (Miller et al., 2020). Metformin (850 mg twice daily as tolerated) was continued for those in the metformin group after being unmasked, whereas lifestyle intervention participants received additional assistance (LaManna et al., 2019). The onset of diabetes, according to the American Diabetes Association criteria, served as the primary endpoint.
Due to concerns about cultural insensitivity and potential backlash, these tactics were left out of the proposed strategy. The proposed approach, on the other hand, prefers tried-and-true techniques for reducing diabetes incidence, such as boosting community engagement, encouraging healthy lifestyles, and improving access to healthcare (LaManna et al., 2019). The proposed strategies for combating diabetes in the United States are all-encompassing, grounded in research, and considerate of other cultures (Miller et al., 2020). This plan intends to decrease the prevalence of diabetes and enhance the health of those who already have it by implementing community outreach and education initiatives, lifestyle modifications, and changes to the healthcare system.
Goals
This study suggests a thorough inquiry into the subject, utilizing SMART objectives, given the pressing need for diabetes prevention and education in the United States. With an estimated 122 million Americans suffering from diabetes or pre-diabetes, the financial and personal costs associated with the condition are substantial (Monika et al., 2021). The suggested program attempts explicitly to accomplish the next set of SMART objectives:
- Specific: The suggested program for preventing and educating people about diabetes intends to achieve particular objectives relating to blood sugar and lipid levels, weight growth and development, preventing and treating diabetes-related disorders, and enhancing health via a good diet. These explicit and measurable objectives make tracking development and success in obtaining the intended results possible.
- Measurable: To reduce diabetes prevalence among Americans through effective education and prevention strategies that promote health, decrease healthcare expenses, and improve overall quality of life.
- Achievable: A comprehensive diabetes education and preventive program created to accomplish these targets, to concentrate on individuals at high risk for acquiring diabetes, such as those with pre-diabetes, obesity, hypertension, or a family history of the illness. (Wu & McGoogan, 2020).
- Relevant: The proposed program would focus on individuals at high risk of developing diabetes, including those with prediabetes, obesity, hypertension, or a family history of the condition. The program will teach diabetic self-management, wholesome eating, exercise, and weight control. The program may address the requirements of those at risk, making it pertinent and efficient for controlling and preventing Diabetes.
- Time-bound: The program will be developed with cultural sensitivity and specificity to address the demands of different demographics, motivate people to take control of their health, and accomplish long-lasting lifestyle changes (Miller et al., 2020).
This plan, which emphasizes SMART objectives, seeks to reduce the number of Americans who have diabetes by implementing effective education and preventative measures that improve health, lower medical costs, and enhance people’s quality of life.
Objectives
Funding for this planned project aims to improve the health of diabetic patients. The project’s goal is to equip participants with the knowledge and tools necessary to self-manage their diabetes, including tracking their glucose levels, taking their medications as prescribed, and making healthy dietary choices (Monika et al., 2021). Because of their elevated risk of cardiovascular disease, diabetics’ optimal blood lipid concentrations are another target (Wu & McGoogan, 2020). The project aims to educate participants on tools to control their cholesterol and triglyceride levels through medical treatment and behavioral interventions, including diet and exercise.
The project also aspires to supply adequate calories for a healthy weight, expected growth, and development while pregnant and breastfeeding. Healthy eating and portion control will be emphasized, and people will be shown how to shop for and prepare nutritious meals that respect their tastes and cultural backgrounds (Wu & McGoogan, 2020). The initiative also aims to prevent, postpone, and treat diabetes related problems (Wu & McGoogan, 2020). To prevent and manage neuropathy and cardiovascular disease, it will be necessary to provide knowledge and resources on the importance of routine healthcare visits, practical medication use, and lifestyle changes, including diet and exercise.
The project’s primary objective is to promote good eating habits among people. A balanced diet emphasizing nutrient-dense foods such as fruits and vegetables, whole grains, lean proteins, and healthy fats while minimizing processed and sugary foods intake is essential to achieving this goal (Wu & McGoogan, 2020). This funding project has lofty goals that should help people with diabetes live longer, healthier lives. This project has the potential to significantly improve the quality of life for people with diabetes by helping them maintain healthy blood glucose and lipid levels (Macomb et al., 2020). This would help obtain enough energy to support growth and development, avoid or manage diabetes-related complications, and promote overall nutritional health.
Outcomes
The study’s findings show that public health programs to raise awareness of type 2 diabetes over the last 30 years have resulted in better screening in the United States. Nevertheless, this study found significant disparities in the frequency of undiagnosed diabetes among various population groupings (Monika et al., 2021). According to this study, 20% to 30% of Americans have diabetes, yet only 9.5% have it (Wu & McGoogan, 2020). Unlike the CDC’s estimates of undiagnosed diabetes, which are based on a single blood test result, this study employed clinicians’ two-test criteria to screen for diabetes.
According to the statistics, the actual figure is substantially lower, and physicians in the United States generally do an excellent job with diabetes screening and diagnosis. There is still a long way to go since “undiagnosed Diabetes continues to be prevalent in various subgroups” (Macomb et al., 2020). According to the findings of this study, persons of color, primarily Mexican and Asian Americans, and those without access to health care are more likely to have undiagnosed Diabetes (Macomb et al., 2020).
Diabetes is a considerable danger to public health due to its global prevalence. Diabetes, characterized by persistently high blood sugar levels, affects about one-quarter of adults aged 65 and over in the United States (Macomb et al., 2020). Diabetes has grown more widespread in recent decades as the obesity pandemic has progressed. Diabetes patients with chronically high blood sugar levels might develop retinopathy, kidney failure, and nerve damage, to name a few problems.
The report’s figures were derived from a nationwide survey and a single case of hyperglycemia in the blood. If that figure is accepted, diabetes affects around 22% of the population (Monika et al., 2021). According to this study, the CDC predicted in the 2020 National Diabetes Statistical Report that 2.8% of the population aged 18 and above, or roughly 7 million Americans, have undiagnosed Diabetes (Bowen et al., 2021). For example, if a patient’s fasting glucose test results are abnormal, professional guidelines recommend either repeating the fasting glucose test a few weeks later or conducting a glycated hemoglobin (HbA1c) test (Mizumoto et al., 2020). To prevent giving patients a false positive Diabetes diagnosis, clinicians frequently delay making a diagnosis until they have validated a high-test result.
The same two-test criteria were used in this study, which included blood samples from the Centers for Disease Control and Prevention. According to the findings of this study, nationally representative samples of individuals in the United States have participated in these surveys for decades, which combine interview questions with physical examinations (Monika et al., 2021). Between 1988 and 2020, 34,924 persons were interviewed, with the final interview occurring just before the COVID-19 pandemic (Mizumoto et al., 2020).
According to the findings of this study, the 2017-2020 dataset revealed a national prevalence of 1.23%, which is lower than the CDC’s current estimate based on single test results and 9.5% of the overall diabetes prevalence (Bowen et al., 2021). Since 1988, the prevalence of undiagnosed diabetes has remained virtually steady, as estimated by this more cautious technique (Monika et al., 2021). Most people with undiagnosed diabetes appear to have been found by traditional procedures
According to the findings of this study, the number of people diagnosed with diabetes has risen considerably. From 4.6% of the population during the 1988-1994 survey period to 11.7% between 2017 and 2020 (90.5% of the overall prevalence of diabetes in the nation) (Monika et al., 2021). Consequently, the growth in diabetes prevalence in the United States during the last several decades is due primarily to an increase in the number of persons with the condition who have been detected and treated (Basch et al., 2020).
According to this study, Mexican Americans had a confirmed undiagnosed diabetes prevalence of 3.31%, about three times the national average and nearly four times the proportion (0.86%) for non-Hispanic white Americans (Basch et al., 2020). As a result, they are the demographic group with the highest rate of undiagnosed Diabetes (Mizumoto et al., 2020). Diabetes was undiagnosed in three times as many Asian Americans as whites.
Impacts
Despite reduced pharmaceutical therapy from participants’ doctors, the lifestyle intervention improved blood pressure and cholesterol levels. Since arbitrary cut-off points of hyperglycemia define diabetes, the progression of hyperglycemia must be controlled, or the onset of diabetes must be postponed. If one assumed that avoiding or delaying the beginning of diabetes based on established glycemic cut-offs would also avoid or delay the onset of long-term diabetic complications, one would be accurate. Diabetes problems were too rare to investigate treatment effects. As a result, a complete DPPOS follow-up is necessary to see whether postponing diabetes onset provides the same effect as avoiding it.
This study’s findings are consistent with previous research on the impact of lifestyle or other anti-diabetic drug therapy on delaying or preventing diabetes in the DPPOS. Two more lifestyle intervention trials with long-term follow-up based on this study discovered continued variability in the cumulative incidence of diabetes (Monika et al., 2021). The practices of the DPP lifestyle group were used in the Finnish Diabetes Prevention Study.
Over the 4-year intervention period, the rate of new diabetes cases fell by 58%, according to this study (Olivia et al., 2021). Even though the intervention was not actively delivered during the 3-year follow-up, there was a 39% reduction in the incidence (Olivia et al., 2021). This study, however, found that the prevalence of Diabetes complications was too low to investigate treatment effects. As a result, a thorough DPPOS follow-up is required to determine if delaying the onset of Diabetes has the same benefit as avoiding it.
The outcomes of this research show that the Da Qing12 preventive experiment included 577 Chinese people with impaired glucose tolerance, and its results were reported 18 years and 20 years afterward. After six years of treatment, 68% of the usual care group, 48% of the diet group, 41% of the exercise group, and 46% of the diet plus exercise group had Diabetes (Olivia et al., 2021). However, this study recorded a statistically significant reduction in cumulative incidence over 20 years for the three treatment groups compared to the usual care group (Basch et al., 2020). Nevertheless, interpreting data becomes more difficult due to the shift in how Diabetes is diagnosed over time (Monika et al., 2021). To our knowledge, the DPPOS is the only reported long-term follow-up of a pharmacological intervention to prevent Diabetes.
Evaluation Protocol
For the proposed plan to address the diabetes problem in the United States, an evaluation process is essential (Basch et al., 2020). There is a proposal for an evaluation scheme, as follows:
Baseline Assessment
A baseline evaluation will be performed before the approach is implemented to ascertain the current prevalence of Diabetes and pre-diabetes in the population. The present state of knowledge, attitudes, and actions toward diabetes treatment and prevention will also be evaluated (Monika et al., 2021). The evaluation process will give a complete picture of how well and how far the suggested strategy to combat Diabetes in the U.S. has reached its goal.
Implementation Assessment
The strategy’s progress and efficacy will be assessed regularly during its implementation phase. The number of patients who have been diagnosed with diabetes or pre-diabetes, as well as the number of people who have received education and support related to diabetes prevention and treatment, will be tracked regularly.
Outcome Evaluation
After implementing the plan, its efficacy in accomplishing its stated goals will be assessed through an outcome evaluation (Mizumoto et al., 2020). Diabetes prevalence, pre-diabetes rates, and improvements in knowledge, attitudes, and behaviors linked to management and prevention will all be measured and analyzed as part of this review.
Cost Evaluation
A cost-effectiveness analysis will assess the strategy’s monetary impact. The intervention’s price tag and potential savings due to better diabetes control and prevention will be factored into this evaluation. The evaluation’s findings will be utilized to fine-tune and enhance the strategy for future use; ultimately, this will help the intended population have better health outcomes and lower rates of diabetes.
Formative Evaluation Plan
Overview
This formative assessment plan is designed to determine the success of a U.S. diabetes education and prevention program in lowering the disease’s incidence and prevalence. The program’s overarching goal is to raise public awareness about the significance of early identification and management of diabetes by educating individuals on preventing the illness through lifestyle modifications (Olivia et al., 2021). In this document, we detail the approach and methods that will be used to assess the initiative’s success.
Evaluation Questions
The following evaluation questions will guide the formative assessment of the diabetes education and prevention program:
- How well-informed is the intended audience about diabetes?
- Do you think the teaching materials would help raise diabetes awareness?
- What prevents people from making the healthy lifestyle modifications necessary to prevent diabetes?
- After finishing the program, can people adjust their eating habits and exercise routines?
- How happy are those who have participated in the program in general?
Evaluation Methods
The following evaluation strategies will be employed to respond to the evaluation questions:
- Surveys. To measure the extent to which the population at large is familiar with diabetes, a survey will be conducted. The instructional materials and the program’s influence on participants’ knowledge and awareness of diabetes will be assessed by a follow-up survey.
- Focus groups. Diabetes prevention focus groups will be used to identify obstacles to adopting healthy lifestyle changes. Participant feedback and suggestions for program enhancements will also be gleaned from the focus groups.
- Pre- and post-program assessments. Measurements of participants’ dietary habits and physical activity levels will be taken before and after the program begins. After finishing the program, the participants’ capacity to control their Diabetes will be measured by these tests.
- Participant satisfaction surveys. To gauge how contented people are with the program as a whole, surveys of participants will be administered. You should also expect suggestions for tweaks to the application in the survey results.
- Data Analysis. Descriptive statistics, such as mean, median, and standard deviation, will be used to examine the data gathered from the surveys, focus groups, and evaluations (Olivia et al., 2021). The significance of the findings will also be evaluated using chi-square testing. The information gained from the discussions will be evaluated thematically to spot trends.
Timeline
The formative assessment will take place over a year. Here is the schedule for the assessment:
- Months 1-2: Development of survey and assessment tools.
- Months 3-4: Recruitment of participants and pre-program assessments.
- Months 5-8: Program implementation and post-program assessments.
- Months 9-10: Focus groups.
- Months 11-12: Data analysis and report writing.
The success of the diabetes education and prevention program may be gauged using the information gleaned from the formative assessment strategy discussed above. Participants’ capacity to manage their diabetes, as well as their understanding of diabetes and willingness to make healthy lifestyle changes, will all be factored into the evaluation. The evaluation’s findings will refine the program and increase its impact on diabetes prevention and management in the United States.
Summative Evaluation Plan
Overview
To determine how successful the Diabetes Education and Prevention program in the United States is, we will use a Summative Assessment Plan. The program’s overarching goal is to reduce the number of people with diabetes and pre-diabetes and stop Type 2 diabetes in its tracks (Monika et al., 2021). As a result of following this strategy, we will be able to assess how well the program met its predetermined objectives (Sophia et al., 2021). If the program successfully produces the expected results, an evaluation will be conducted, and enhancement suggestions will be offered.
Evaluation Design
A quasi-experimental setup with a different control group will be used for the analysis. Those not part of the program will be used as a comparison group for those in the program (Sophia et al., 2021). Shared demographic and health features will stratify the groups to minimize potential bias. The study will employ a before-and-after test design to evaluate the impact on participants’ understanding, actions, and health (Sophia et al., 2021). We will also use a process evaluation to gauge how well the program was carried out and whether or not it was implemented with integrity.
Data Collection
Quantitative and qualitative information will be gathered for the evaluation, which will be gathered before the program, during the program, and six months later. Surveys and biometric measurements will compile the quantitative data (LaManna et al., 2019). The surveys will measure progress in understanding, practice, and health. Biometric assessments will evaluate metabolic, cardiovascular, and skeletal alterations. Methods like focus groups and one-on-one interviews will be used to get qualitative information (Sophia et al., 2021). Focus groups and interviews will gain insight into participant experience, challenges to behavior change, and program enhancement ideas.
Data Analysis
Descriptive and inferential statistics will be used to examine the numerical data. The demographic and health features of the program’s participants and the control group will be described using descriptive statistics (Sophia et al., 2021). Knowledge, behavior, and health outcomes will be compared between the two groups using inferential statistics. Thematic analysis will be used to make sense of the qualitative data (Sophia et al., 2021). The research questions will guide the development of overarching themes that will be used to analyze the responses of program participants and draw conclusions about those responses.
Outcomes
The program’s success will be measured against the criteria mentioned above. The program’s success will be measured by contrasting before-and-after assessments of program members’ knowledge, behavior, and health (Sophia et al., 2021). The results will be evaluated twice: just after the program ends and again six months afterward (Monika et al., 2021). The results obtained will be analyzed quantitatively and qualitatively.
Recommendations
Based on the evaluation’s findings, improved program recommendations will be made. The proposed changes will make the program more efficient in generating the required results (Sophia et al., 2021). Changes to the program’s content, distribution, or implementation tactics could all be on the table (Monika et al., 2021). The assessment findings will inform the recommendations, which will be crafted in collaboration with the program’s key stakeholders.
Results Summary
The summative assessment plan for the United States Diabetes Education and Prevention program is essential for gauging the program’s success in reaching its stated goals and outcomes. The plan’s mixed-methods approach will yield complete information on the program’s effects on the intended audience (LaManna et al., 2019). Financial and time commitments associated with the evaluation plan have been thoroughly thought out and justified (Monika et al., 2021). To better meet the needs of people with diabetes and those at risk of getting the disease, the evaluation’s findings will inform future program enhancements.
Relationship to Goals/Outcomes
The objectives and results of the proposed diabetes education and prevention plan in the United States of America are well-defined. Focusing on type 2 diabetes, the program’s primary objective is to lower the national incidence and prevalence of the disease (Monika et al., 2021). The plan aims for optimal blood glucose and cholesterol levels, enough energy for a healthy weight and growth, prevention, delay, and treatment of diabetes-related issues, and better health through a balanced diet.
The program’s strategy is all-encompassing, encompassing education, prevention, and early intervention to achieve the goals above and objectives (Sophia et al., 2021). Plan participants will learn about diabetes, its risk factors, the value of a healthy lifestyle, and the significance of catching the disease early. Diabetes prevention is a primary goal of the program, which also emphasizes encouraging healthy lifestyle choices, including eating right and exercising regularly.
The program’s success criteria match its goals to reduce new diabetes diagnoses and the number of Americans with the disease. More people will be screened for diabetes, and a more significant percentage of people will engage in healthy lifestyle behaviors due to the program’s efforts to raise awareness of diabetes and its risk factors (Monika et al., 2021). Furthermore, the program’s goals must be met to maintain healthy levels of blood glucose and lipids, avoid diabetes-related problems, and supply adequate energy for weight maintenance and healthy development (Sophia et al., 2021). By achieving these results, we can lessen the health and financial toll that diabetes takes on the United States. The quality of life for diabetics will also improve if the prevalence and incidence of complications can be reduced.
The United States of America’s plan for diabetes education and prevention is a well-defined and all-encompassing strategy with well-defined goals, objectives, and outcomes. The goals of the program to reduce the incidence and prevalence of diabetes in the United States are directly related to the goals of the plan, which include optimal blood glucose and lipid concentrations (Monika et al., 2021). Preventing diabetes-related complications and providing adequate energy for weight management and average growth and development (Wu & McGoogan, 2020). If this program improves the lives of persons with diabetes or at risk for it, it could reduce the health and economic burden of diabetes in the U.S.
Summary
In conclusion, diabetes affects millions of Americans and causes many problems and fatalities. The proposed financing addresses this issue by focusing on diabetes education and prevention programs. This plan proposes to lower the U.S. diabetes burden by raising awareness, encouraging healthy lifestyles, and providing early detection and management tools. Diabetes prevention and management in the U.S. can be significantly improved with financing, partnerships, and community support.
Budget
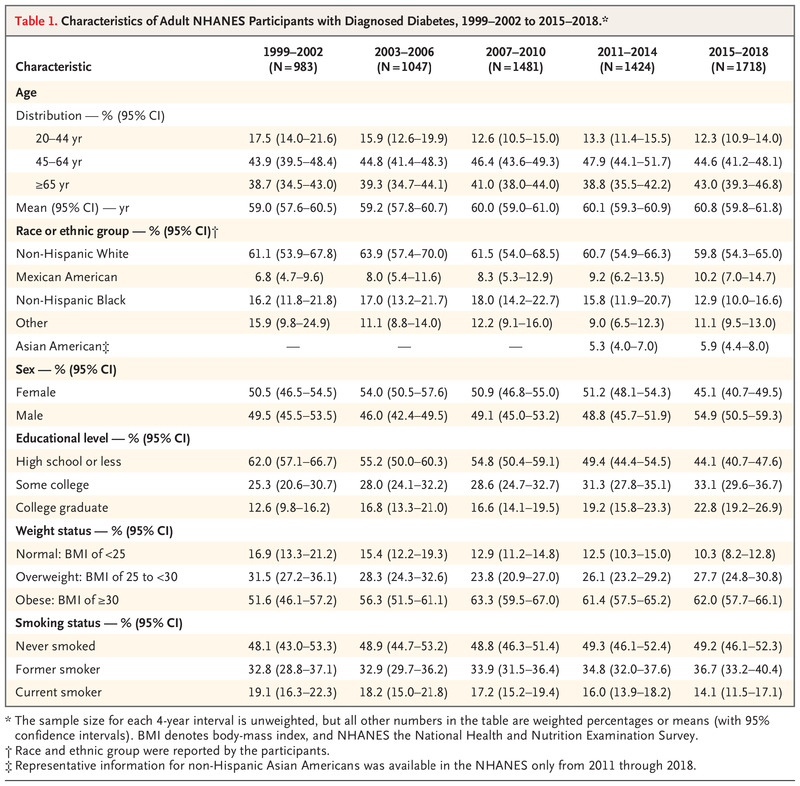
The size and scope of the diabetes education and prevention program in the US will determine the size of the evaluation budget. However, a rough budget can be made to cover the costs of the evaluation strategy (LaManna et al., 2019). The budget is an estimate that may change based on the particulars of the evaluation strategy. Some of the costs associated with the evaluation can also be covered by money set aside in the program budget (Wu & McGoogan, 2020). The budget evaluation plan’s projected costs are in Table 1 as follows:
Table 1. Budget Plan (Wu & McGoogan, 2020)
Budget Narrative/Justification
The necessity to ensure the Diabetes Education and Prevention program in the US meets its aims and objectives justifies the cost of the assessment plan for the program. Funding for the evaluation plan is essential to ensuring its thoroughness and strength in establishing the program’s success (Monika et al., 2021). Money has been allocated for data acquisition, processing, and report writing. A skilled workforce and high-end hardware/software are essential for doing these tasks successfully (Sophia Contreras et al., 2021). Incentives for study participants are built into the budget, in addition to monies for community engagement and participant recruitment.
Budget allocations also cover training and capacity building for program employees, which is essential for the successful rollout of the evaluation strategy. In addition, the budget allots resources for monitoring and quality assurance, guaranteeing proper program execution and reliable data collection (Monika et al., 2021). The budget narrative explains why all the allocated money is necessary and how it will be spent. Cost sharing, if any, and evaluation plan financing sources are detailed in the budget narrative (Sophia et al., 2021). The budget story guarantees the budget’s openness and accountability and that the allocated funds will be used efficiently to accomplish the program’s aims.
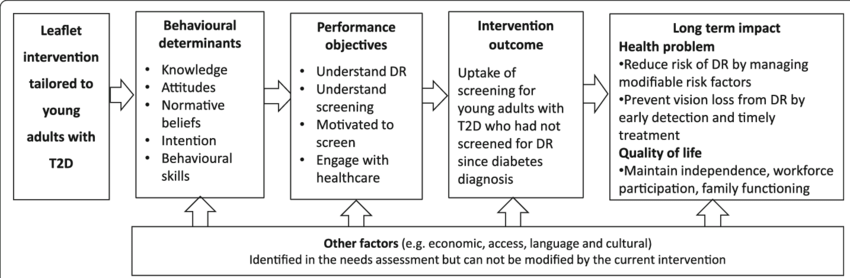
Logical Model
Diabetic retinopathy can be effectively treated if detected and treated early, but only if a patient has had a retinal examination. Diabetic retinopathy is the leading cause of blindness and vision loss in working-age adults, and it can develop quickly and severely in young adults (18–39) with type 2 diabetes (Sophia et al., 2021). Increased use of retinal screening among young adults with type 2 diabetes: a targeted intervention, as depicted in Figure 2 below.
References
Basch, C. H., Hillyer, G. C., Meleo-Erwin, Z. C., Jaime, C., Mohlman, J., & Basch, C. E. (2020). Preventive behaviors conveyed on YouTube to mitigate transmission of COVID-19: Cross-sectional study. JMIR public health and surveillance, 6(2), e18807. Web.
Bowen, A., Miller, A. D., Zambrano, L. D., Wu, M. J., Oster, M. E., Godfred-Cato, S., & Campbell, A. P. (2021). Demographic and clinical factors associated with death among persons< 21 years old with multisystem inflammatory syndrome in children—United States, February 2020–March 2021. Web.
LaManna, J., Litchman, M. L., Dickinson, J. K., Todd, A., Julius, M. M., Whitehouse, C. R., & Kavookjian, J. (2019). Diabetes education impact on hypoglycemia outcomes: a systematic review of evidence and gaps in the literature. The diabetes educator, 45(4), 349-369. Web.
Macomb, C. V., Evans, M. O., Dockstater, J. E., Montgomery, J. R., & Beakes, D. E. (2020). Treating SIRVA early with corticosteroid injections: a case series. Military Medicine, 185(1-2), e298-e300. Web.
Miller, A. D., Zambrano, L. D., Yousaf, A. R., Abrams, J. Y., Meng, L., Wu, M. J., & Campbell, A. P. (2022). Multisystem inflammatory syndrome in children—United States, February 2020–July 2021. Clinical Infectious Diseases, 75(1), e1165-e1175. Web.
Mizumoto, K., Kagaya, K., Zarebski, A., & Chowell, G. (2020). Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess Cruise ship, Yokohama, Japan, 2020. Eurosurveillance, 25(10). Web.
Monika, K., Ali, L., Timothy, L., Gabriel, Q., & Hadas. (2021). Alameda Health System Foundation grant proposal for diabetes education and prevention in children k–12. Department of Public Affairs and Administration, California State University, East Bay.
Olivia, B., Margaret, C., Jean, M., Gurbir, S., & Derek, W. (2021). Ronald McDonald House Charities Transportation Assistance Program Grant Proposal. California State University East Bay
Shin, S. M., Oh, T. J., Choi, S. H., & Jang, H. C. (2021). Effects of social distancing on diabetes management in older adults during the COVID-19 pandemic. Diabetes & Metabolism Journal, 45(5), 765-772. Web.
Sophia, C., Christabelle, D., Cristina, O., Jackeline, R., & Tiona, S. (2021). Grant proposal assembled. Department of Public Affairs and Administration, California State University, East Bay.
Wu, Z., & McGoogan, J. M. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama, 323(13), 1239-1242. Web.