The Problem: Medication Errors
- Medication errors: the use of wrong medications or wrong dosage.
- The most common medication errors are related to the choice of patients, the right time to take drugs, and repetitive prescriptions (Wahr & Merry, 2017).
The problem of medication errors or inappropriate treatment is strictly interconnected with common mistakes and omissions related to the practical work of certain solutions. Nowadays, many researchers including Wahr and Merry (2017) regard medication errors as one of the key problems of the healthcare system as the mistakes related to dosages, incorrectly chosen patients, and medications that are prescribed repeatedly is detrimental both to patient outcomes and the level of trust to healthcare specialists. Therefore, specialists from many healthcare institutions in the country understand that the approach to the choice of HIT solutions should be improved.
Patient Safety
Threats to patient safety exist due to the presence of the human factor.
The challenges to patient safety include medication errors, the lack of information on reaction to drugs, and delayed completion of orders.
It is known that patient safety is protected with a wide range of healthcare information technology innovations. The problem of patient safety cannot be analyzed separately from the topic of HIT-related innovations as the latter, together with professionalism of healthcare specialists presents the key allowing to improve patient safety in the country. The importance of patient safety studies cannot be overstated, but it needs to be acknowledged that the challenges to patient safety exist due to ineffective use of information on orders, prescriptions, and health history in healthcare institutions. To reduce the impact of negative factors identified, healthcare institutions need to adopt new IT systems with proven effectiveness.
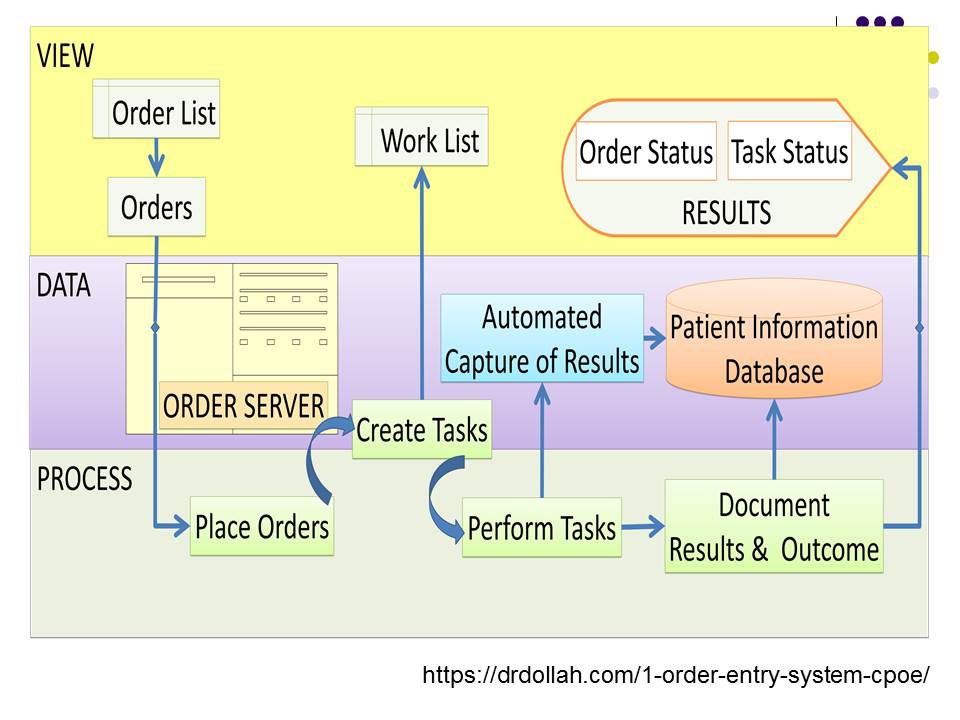
What is CPOE?
CPOE or Computerized Physician Order Entry is the technology that involves the exchange of data on treatment instructions and requirements with the help of CPOE software.
The technology allows to use great amounts of information in a more effective way.
Taking into account the importance of healthcare problems discussed before, I am glad to introduce the solution that is proven to be effective for reducing the frequency of medication mistakes and their negative outcomes. Computerized Physician Order Entry is the technology that allows healthcare practitioners to exchange medical treatment guidelines to make the work of healthcare specialists less time-consuming and help them to utilize a patient-centered approach. CPOE involves the creation of the effective system ensuring a rapid order completion. Also, speaking about the most prominent features of the discussed HIT innovation, it is important to note that it provides an opportunity to integrate the information related to health history and current prescriptions to facilitate the decision-making process and reduce the number of medication mistakes.
How Can CPOE Improve the Healthcare System?
- Reduce the mistakes related to the lack of unity of professional terminology.
- Estrange the mistakes that occur due to the misinterpretation of treatment instructions (Prgomet, Niazkhani, Georgiou, & Westbrook, 2016).
- Manage healthcare orders to avoid the cases of late treatment.
In fact, the discussed technology has a number of opportunities to improve the current healthcare system if implemented correctly. First, order entry practices that were utilized prior to the global development of HIT innovations provide healthcare specialists with an opportunity to use atypical terms and abbreviations. In its turn, the lack of unity of professional terminology can be listed among the primary sources of medication mistakes. The influence of the human factors and specific ways to write certain letters or numbers can be seen as the leading cause of misinterpretation of data increasing the rate of medication mistakes. What is more, the use of the technology improves patient safety as effective data integration makes the work with healthcare orders more time-consuming and goal-oriented.
The Benefits of CPOE
- The process of information exchange between healthcare specialists is simplified;
- A large number of devices can be used to work with orders;
- The presence of the error checking function (Romanow, Rai, Keil, & Luxenberg, 2017).
Choosing an effective strategy related to HIT-related innovations, it is crucial for healthcare providers to consider the benefits and potential problems associated with the implementation of innovations. The use of CPOE in healthcare is beneficial to healthcare institutions, healthcare practitioners, and patients due to the number of advantages that it involves. In fact, the system based on CPOE makes it easier for healthcare specialists to communicate as the average response time is decreased. Another important positive feature exists because the system is portable and can be accessed by specialists even if they are far away from their working places. Also, you can work with orders using different digital devices. Finally, there is the advantage preventing users from making medication mistakes – the system double-checks new information to prevent unnecessary repetitions.
Possible Challenges
- The system cannot guarantee the absence of mistakes (therefore, users still need to double-check doubtful information).
- Considering different levels of computer literacy and adaptability of healthcare specialists, the speed of working processes may decrease for a short time (McCartney, 2014).
Unfortunately, every medal has two sides, and the implementation of CPOE may involve potential problems. Nevertheless, they can be reduced if healthcare institutions will focus more on long-term goals of its implementation. The first potential challenge that needs to be discussed is the inability of CPOE systems to identify all mistakes that can be found in treatment instructions. At the same time, the majority of studies confirm improved patient outcomes after the implementation of CPOE, and it means that every medication mistake has increased chances of being noticed by the software.
The second challenge discussed may disappoint managers of healthcare institutions who place a premium on quantity instead of quality. In fact, CPOE implementation is a significant change that requires specialists to get used to new everyday practices. Therefore, working processes may slow down for some time after the start of the implementation.
How is CPOE Implemented?
- IT governance and leadership: The assistance of innovative HIT leaders (Snedaker, 2016).
- The use of employee analysis to identify the perfect length of the training period;
- The readiness to meet changing CPOE standards.
In terms of the proper strategy that needs to be used for successful CPOE implementation, there are a few points to be paid focused attention to. First, CPOE has a great potential, but it tends to be misused; therefore, effective HIT leadership should be used to guide healthcare providers and elaborate the strategy. Next, stakeholders willing to implement CPOE systems should focus on the necessity of an appropriate training period. In its turn, its length must be defined based on the level of employees’ computer literacy and specific challenges. Finally, CPOE implementation is the task that requires concerted efforts of specialists on different levels and the willingness to meet the most recent standards.
References
McCartney, P. (2014). Computerized Provider Order Entry (CPOE): Evidence on implementation challenges. MCN: The American Journal of Maternal/Child Nursing, 39(1), 63.
Prgomet, M., Li, L., Niazkhani, Z., Georgiou, A., & Westbrook, J. I. (2016). Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: A systematic review and meta-analysis. Journal of the American Medical Informatics Association, 24(2), 413-422.
Romanow, D., Rai, A., Keil, M., & Luxenberg, S. (2017). Does extended CPOE use reduce patient length of stay? International Journal of Medical Informatics, 97(1), 128-138.
Snedaker, S. (2016). Leading healthcare IT. Boca Raton, FL: CRC Press.
Wahr, J. A., & Merry, A. F. (2017). Medication errors in the perioperative setting. Current Anesthesiology Reports, 7(3), 320-329.