Introduction
Vibrio cholera is the causative agent of Cholera, a severe epidemic diarrheal disease that attacks both children and adults. Infection results from the consumption of food or water contaminated by the bacterium Vibrio cholera (3). The disease is treatable but can cause death within just a few hours if no intervention is taken. Cholera remains a serious public health concern. The World Health Organization estimates 3-5 million cholera cases every year with a reported 100 000- 120 000 deaths (9).
However, there is a marked disparity in prevalence rates between developed and developing countries with poor sanitation in the later having been cited as the main cause (9). In the United States, cholera cases remain extremely low and this has been attributed to improved hygiene and sanitation over the year (8). Cholera cases reported in the United States are those that result from travel to endemic areas and the consumption of undercooked seafood.
Incidence rates remain low with 0.50 cases per 100,000 population from 2003-2008 recorded for people older than 50 years (8, 9). Worldwide Cholera statistics are not accurate as many cases/incidences are not reported (8, 9). Many countries fear the negative impact Cholera outbreak reports may have on local economic activities such as trade and tourism (8, 9). Recent epidemics have been reported in Zimbabwe (2008-2009) and in Haiti (2010).

Vibrio cholera is a comma-shaped, anaerobic bacterium whose size ranges from 1-3 µm in length and 0.5 – 0.8 µm in diameter (8, 3). Its major proteinous building blocks are a flagellin H antigen and a somatic O antigen (8). The bacterium belongs to the genus Vibrio and shares the characteristic features of these members such as facultative anaerobism, asporogenosity, motility, and being gram-negative (5).
These bacteria are also predominantly aquatic, inhabiting areas such as estuaries and brackish water with algal bloom (5, 9). In such an aquatic environment, the bacterium thrives in association with zooplankton and phytoplankton where they exist as free-swimming cells, attached to plants, algae, copepods and other sea animals (4). Apart from water sources eating raw or undercooked seafood has also been associated with the development of the disease (5).
This is one of the main sources of transmission in the United States (1). The bacterium has the ability to ferment glucose, sucrose and mannitol and this feature has been utilized in many laboratory tests (5). The main reservoirs of Vibrio cholera are humans and water. Animals do not play any role in transmission (8). Infection is high in communities with poor hygiene standards. Other etiological factors cited are human migration and seasonal climatic warming along the coastlines.
These conditions enable Vibrio members to thrive. Interestingly, studies have shown that people with type O blood group have a higher than normal susceptibility to cholera (8). Although there are many subgroups of the bacterium only the O1 and O139 serogroups have been known to cause epidemic and pandemic Cholera(5). There are three serogroups of Vibrio O1 namely: Inaba(O antigen A and C), Ogawa (O antigen A and B) and Hikojima (O antigen A, B and C) (8).
Mechanism of pathogenesis
There are about 200 strains of Vibrio Cholerae bacterium but only two strains, O1 and S139 are associated with pandemic and endemic cholera(8). The S139 strain (Bengal) is endemic in Asia (8, 5). A person gets infected from ingesting water or food contaminated with Vibrio cholera. Infection dose for the manifestation of clinical symptoms varies depending on the mode of infection but is higher from water compared to food (8).
Nevertheless, infection requires a very high ingestion dose. Once ingested the bacteria migrate to the small intestines and begin to multiply (6). The incubation period may last 18h to 5 days (5). However, large quantities of ingested Vibrio cholera are needed in order to develop symptoms (6). Cholera is highly virulent (9). Signs of Cholera get noticeable 18h to 5 days after ingestion (5). General symptoms are akin to those of gastrointestinal diarrhea and include sudden weight loss, excessive thirst, postural hypotension, fatigue, dry mouth, sunken eyes, wrinkled skin, somnolence and comma in advanced stage (8). Children may experience hypoglycemia (8).
Children and adults normally experience similar signs although extreme drowsiness, convulsions and coma are rare in adults (8). Most Vibrio cholera infections are asymptomatic. In fact, mild to moderate infections may not be distinguishable from other causes of gastroenteritis (8). Symptomatic cholera is distinctively characterized by voluminous watery diarrhea at the peak of infection often with vomiting (8).

The stool resembles ‘rice water’ and may have a characteristic ‘fishy’ smell (5). However, victims infected may not necessarily exhibit the hallmark watery diarrhea but mild diarrhea without serious debilitating symptoms (5). Vomiting is caused by reduced motility in the gastric and intestines (8). Vomiting may not always be present (5). The vomitus is normally a clear alkaline fluid (5). This causes the body to lose so much water that patients develop severe dehydration and shock and entire vascular collapse within just a few hours(8). If unchecked, death commonly results in less than 24 hours (8). Dehydration is proportional at the intracellular, intravascular and interstitial levels (8). The WHO has classified dehydration as severe, moderate or mild and specifies appropriate interventions for each (8). Severely dehydrated children and adults may suffer from tachycardia, extremely low pulse and hypotension (8). Without early interventions measures Cholera fatalities can be a high of over 50 %( 5).
Development of the disease is brought about by the colonization of the proximal small intestine upon which the bacterium produces a cholera toxin that accelerates diarrhea. The fluid and electrolytes (K+ and bicarbonates) loss is confined to the duodenum and upper jejunum (8). The major salts lost are bicarbonates and potassium ions (8). The endotoxin of the O1 type is made up of proteinous subunits 5B and 2A that confers virulence (3). The O139 strain produces a similar endotoxin except that its virulence is enhanced by lipopolysaccharide and a novel O-antigen capsule (8).
Methods for growth in the Lab
Vibrio members can grow at high PH or bile salts, conditions which inhibit the growth of potential confounders such as Enterobacteriaceae (8). Lab cultures are used to confirm cholera outbreaks. TCBS (Thiosulphate Citrate Bile Sucrose Agar) is one of the selective agars used in the isolation and rapid cultivation of Vibrio cholera (7). This medium is highly selective and is able to provide nutritional sustenance for the vibrio species while eliminating non-vibrio micro-organisms.
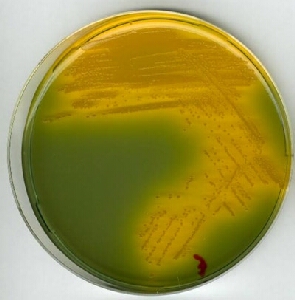
For culturing, sample fresh feces is placed onto a TCBS (Thiosulphate Citrate Bile Salts Sucrose) agar (5). TCBS agar is composed of nutrients, salts and coloring agents namely: mixed peptone, yeast extract, sucrose, sodium citrate, ferric citrate, sodium chloride, sodium thiosulphate, oxbile, sodium cholate, Thymol blue, Bromothymol blue and agar. The PH of this growth medium is around 8.6 at room temperature and pressure (7).
These ingredients set up conditions that inhibit the growth of Enterobacteriaceae (4). Oxbile and bile salts suppress enterococci (4). The Thymol- Bromothymol blue mixture changes to an indicative yellow color when acid is formed from sucrose fermentation by Vibrio cholera (4).
Following 6-12h of incubation, a second inoculation in the same plate is done and incubated for 18-24hours. Growth is evident from the appearance of large smooth and round yellow colonies and is interpreted as a positive identification (7, 8). Yellow coloration is due to the fermentation of sucrose by the Vibrio members (4). No color change indicates a negative reaction. Specific strains of Vibrio known to produce the yellow color include Vibrio alginolyticus, Vibrio cholera and Vibrio fluvialis (7). However, the yellow color can also be attributed to non-vibrio members such as Enterococcus faecalis, E.coli as a well as Proteaus mirabilis (7).
Positive identification can be confirmed from agglutination on a non-selective medium with O1 or O139 antiserum (5). Notable rapid tests include dark-field microscopy in which the effect of O1 or O139 antiserum is observed on a wet mount of a liquid stool sample(5). Rapid tests are recommended for monitoring the disease in remote areas where cultures are not viable (5).
Serological tests such as slide agglutination can be used to identify Vibrio cholerae O1 serotype antigen on suspect samples (2). However, additional characterization may be necessary to ascertain the cholera toxin (2). Positive serotype identification is based on agglutination on anti-sera to type-specific O antigen(2). Other tests used to reveal important public health information include hemolysis, molecular subtyping, and antimicrobial sensitivity assays (2).
Biochemical tests used to confirm isolates of Vibrio cholera include oxidase tests, String test, Klinger’s Iron agar test, Triple sugar, Iron Agar, salt broth as well as Voges, Poskaver test. Hemolysis tests are based on the ability of certain Vibrio members ability to lyse erythrocytes (2). Although many such strains are now non-hemolytic, it is still used to differentiate various continental strains (2). Specific tests include Plate Hemolysis, Tube and Hemolysis Assay (2). Modern methods with high sensitivity and specificity such as Polymerase Chain Reaction (PCR) have also been developed. PCR has been used to screen food samples (8).
Disease treatment and prevention
Cholera is a treatable disease. Cholera patients lose a high amount of body fluids and electrolytes and the primary treatment regimens seek to first rehydrate the patient to restore the body hydration status in the shortest time possible(8). Rehydration may include Lactated Ringer solution, isotonic sodium chloride solution, or oral rehydration solution (ORS) (8). Intravenous rehydration is performed on severely rehydrated patients (9, 3). The WHO recommends oral rehydration solution for moderately dehydrated patients and replacement of 10% of the bodyweight within 2-4h in severely dehydrated patients (8, 5). The hydration is maintained until diarrhea ceases. Insufficient rehydration may lead to temporary survival only for patients to succumb later (5). For severely dehydrated patients, antibiotics (e.g. doxycycline) can also be used to reduce vomiting and the volume of rehydration solutions needed (8). For extremely debilitated patients a cholera cot may be used to monitor excretion and body hydration.
Patients with cholera are not able to feed but food should be provided as soon as they are able to eat (5). Health authorities are also required to set up accessible treatment centers in the affected areas. Cholera reporting standards and guidelines are periodically reviewed by the WHO (9). Inappropriate treatment has been known to cause complications such as acute renal failure, and miscarriage or premature delivery in pregnant women (8, 5). Painful muscle crumps in legs and limbs are common (5). However, with prompt and proper treatment the high fatalities and adverse effects associated with cholera can be significantly reduced.
Prevention of Cholera outbreak is aimed at hindering the transmission of Vibrio cholera from its source (5). In this case, greater emphasis is laid on improving sanitation and supply of drinking water, thorough cooking of food and mass health education (5,8). During Cholera outbreaks health authorities normally stress purification of water, food preparation, identifying signs of infection and locations for early treatment (9, 5, and 8).
Since its discovery, a number of vaccines against Vibrio cholera have been developed. These vaccines consist of killed V. cholerae and subunits that serve to stimulate immunity against future attacks. Some of them include the Oral ones such as Dukoral, Shancol and Orochol (5). Shancol confers longer protection against V.cholerae in children less than 5 years (5). The quality of these vaccines has improved overtime though some countries such as the US have to date not licensed their use or even recommended them (5). Some vaccines have also not been recommended by WHO due to their low protective efficacy and adverse side effects (1).
Conclusion
Vibrio cholera causes Cholera, a potentially pandemic disease estimated by WHO to claim over 120 000 lives yearly. Many of the bacterium strains are innocuous except for the O1 and S139 types which cause the disease. Infection is brought about by the ingestion of contaminated food and water. Pathogenicity is as a result of the bacterium colonizing the small intestine and releasing an endotoxin leading to development of major symptoms such as voluminous diarrhea and vomiting. Vibrio Cholerae can be cultivated in the laboratory using the TCBS Agar whereby positive growth is evident from development of yellow colonies. Further confirmatory tests can be performed by a number of serological and biochemical tests. The primary intervention for Cholera is rehydration. Vaccines have also been developed although they have only gained acceptance in some countries.
References
Butterton, J.R. (2012). Pathogenesis of Vibrio cholerae infection; Wolters Kluwer Health. Web.
Butler, S. M., & Camilli, A. (2005). Going against the grain: chemotaxis and infection in Vibrio Cholerae. Nature Reviews Microbiology, 3, 611-620. Web.
CDC (n.d.). Laboratory Methods for the Diagnosis of Vibrio cholerae; Centers for Disease Control and Prevention. Web.
Faruque, S.M. & Nair, G.B. (2008). Vibrio cholerae: Genomics and molecular biology. Norfolk: Caister Academic.
Merck, K.G.A. (2002). TCBS Agar. Web.
Sack, D.A., Sack, R.B., Nair, G.B. and Siddique, A.K. (2004), Cholera: The Lacent. Web.
Schoenstadt, A. (2012). Vibrio Cholerae. MedTV; Health Information Brought to Life. Web.
Sigma-Aldrich Inc. (n.d). 86348 TCBS Agar: SIGMA- ALDRICH. Web.
Thaker, V.V. (2011). Cholera: Medscape Reference. Web.
WHO (2012). Cholera; World Health Organization. Web.