Experimental Studies
Vitamin D and LDL
Among nine observational studies, seven unambiguously identified the nature of the relationship between vitamin D and LDL, and two did not find any association between these components. In addition, six of these seven studies demonstrate inverse correlation. At the same time, the results of the seventh study by Skaaby et al. (2012) argue that there is a direct relationship. However, on closer examination, LDL level changes in this observation are insignificant and of low statistical value (Skaaby et al., 2012). Therefore, the available evidence suggests a clear inverse relationship between vitamin D and LDL.
However, experimental studies do not show such a clear picture, as out of five papers, only three emphasize LDL reduction with vitamin D supplementation. The remaining two, by Makariou et al. (2017) and Wenclewska et al. (2019), indicate an increase in these lipoprotein levels. The results of the first work can be considered insufficiently statistically significant since the observed change in the LDL level is much less than the standard deviation (Makariou et al., 2017). On the other hand, the results of the study by Wenclewska et al. (2019) show a small but steady upward trend in LDL that cannot be ignored. Therefore, empirical evidence suggests an inverse relationship between vitamin D supplementation and LDL, but it needs further verification and analysis.
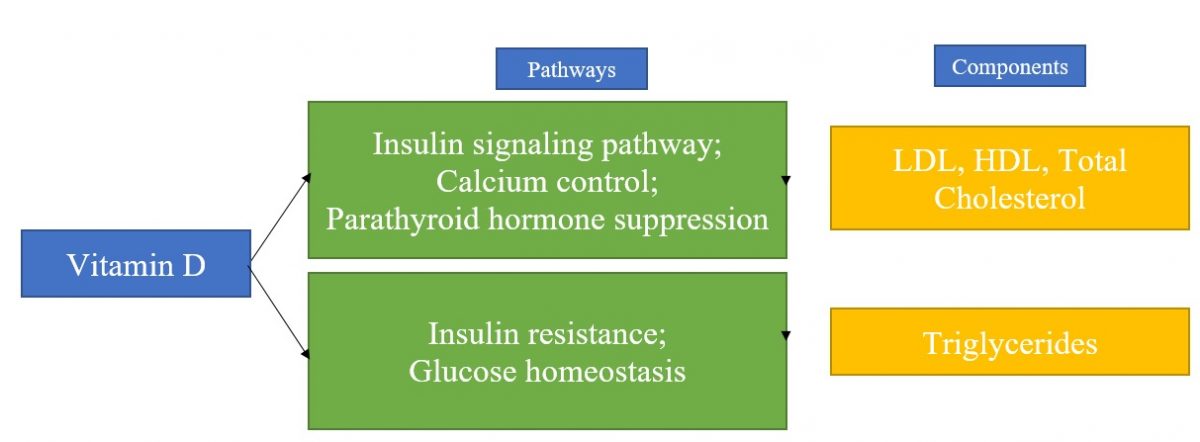
Finally, the reviewed literature makes it possible to identify pathways that influence the relationship between vitamin D and LDL. This vitamin significantly impacts various bodily functions, from reproductive to immune (Wieder-Huszla et al., 2019). In addition, it is closely associated with maintaining glucose homeostasis via the insulin signaling pathway (Wenclewska et al., 2019). However, the specific mechanism by which vitamin D affects lipids and metabolic syndrome (MetS) is less clear (Skaaby et al., 2012). Part of the research links MetS to insulin secretion and sensitivity, using this already well-studied pathway to explain this problem (Schmitt et al., 2018). However, one study takes a more specific approach, looking at calcium control and parathyroid hormone suppression as theoretical pathways (Skaaby et al., 2012). Thus, the particular mechanisms of vitamin D interaction with lipids remain not fully understood.
Vitamin D and HDL
Five of the nine observational studies reviewed found an association between vitamin D and HDL. Each of these cases demonstrates a direct correlation: higher vitamin D levels accompanied increased HDL and vice versa. However, four more studies did not indicate any relationship between these parameters, indicating a lack of evidence in comparison with triglycerides, for example. Thus, evidence from observational studies mostly underlines the positive relationship between these components but requires more detailed and careful investigation.
Among experimental studies, in four out of five cases, vitamin D supplementation also positively affected HDL levels. The only study showing a negative correlation is a work by Kelishadi et al. However, according to the results of their experiments, HDL levels differ very little, less than two mg/dL, while the standard deviation is 3.18 mg/dL (Kelishadi et al., 2014). Therefore, this result is insignificant, and a general analysis of the experimental work suggests solid experimental evidence of a relationship between vitamin D supplementation and HDL.
As in the case of LDL, the exact nature of the relationship between vitamin D and HDL remains not fully understood. The reviewed literature highlights the effects of vitamin D on multiple functions and its close association with various metabolic pathways (Wieder-Huszla et al., 2019). The insulin signaling pathway also seems to be an essential control mechanism (Scmitt et al., 2018). However, the path most closely identified is the regulation of calcium levels and the suppression of parathyroid hormone, as in the case of LDL (Skaaby et al., 2012). In addition, the literature makes it possible to identify the simultaneous influence of these pathways and their joint significance.
Vitamin D and Total Cholesterol
Six of the nine observational studies reported an inverse correlation between vitamin D and total cholesterol levels. At the same time, the authors of two more articles could not find any effect, and the work of Skaaby et al. (2012) noted a slight increase in this parameter. However, in contrast to the relationship between triglycerides and VLDL, the changes in values are extremely small, which reduces their significance. Therefore, based on evidence from observational studies, it is safe to say that there is a negative relationship between vitamin D and total cholesterol levels.
Experimental studies show, at first glance, an ambiguous result in the context of the relationship between vitamin D and total cholesterol. Out of five papers, three note a decrease in cholesterol levels, and two – an increase. However, in the case of Makariou et al. (2017), the increase in total cholesterol is statistically insignificant. However, the increase in total cholesterol in the study by Wenclewska et al. (2019) is caused by increased levels of both its components: HDL and LDL. Thus, there is little evidence for a direct relationship between cholesterol levels and Vitamin D supplements, suggesting that an inverse correlation predominates.
Considering the relationship between the level of total cholesterol and vitamin and analyzing the pathways that can explain this relationship, it is necessary to remember the components of this parameter. Since total cholesterol is made up of HDL, LDL, and other lipids, it is influenced by the same factors that have already been described above. Therefore, among potential pathways, insulin signaling pathway, sex hormone control, and blood pressure control measures can be identified. However, the most likely options concerning the lipid profile remain the management of calcium and parathyroid hormone levels (Skaaby et al., 2012). Moreover, according to the literature, the joint influence of factors is essential since their separate control does not change the picture as a whole (Ahmadi et al., 2015). Therefore, to fully explain these relationships, it is necessary to investigate additional pathways that affect lipid levels, both individually and in general.
Vitamin D and Triglycerides
Observational studies on the relationship between vitamin D and triglycerides show the most consistent results. Eight of the nine papers converge on the presence of feedback between these components, and only one article does not show statistically significant results (Wieder-Huszla et al., 2019). At the same time, other studies, such as the paper by Barbalho et al. (2018), show a significant increase in triglycerides in vitamin D deficiency. With the vast majority of investigations showing similar results, it is safe to conclude that there is strong evidence for an inverse relationship between vitamin D and triglycerides.
In the context of experimental studies, the most stable result is also observed since all five papers studied confirm a decrease in the triglycerides when using vitamin D supplementation. Therefore, the available experimental evidence additionally emphasizes the connection already established with the help of observations. However, it is worth noting that the reliability and unconditionality of such a relationship are because, unlike total cholesterol, HDL, and LDL, which are related to each other, triglycerides are a separate component. Therefore, its interaction with vitamin D is somewhat more straightforward.
The analyzed literature identified no mechanism that would directly explain the relationship between vitamin D and triglycerides. However, some already identified pathways may apply in this context. First of all, this association is best explained by the effect of vitamin D on insulin resistance. This mechanism provokes inflammatory cytokine production, which in turn is associated with obesity and, as a result, triglycerides (Kelishadi et al., 2014). In addition, the relationship between vitamin D and glucose tolerance may be a potential explanation (Baker et al., 2012). However, no exact explanatory effects have been found, and this issue requires further study.
References
Ahmadi, F., Damghani, S., Lessan‐Pezeshki, M., Razeghi, E., Maziar, S., & Mahdavi‐Mazdeh, M. (2016). Association of low vitamin D levels with metabolic syndrome in hemodialysis patients.Hemodialysis International, 20(2), 261-269. Web.
Alkhatatbeh, M. J., Abdul-Razzak, K. K., Khasawneh, L. Q., & Saadeh, N. A. (2017). High prevalence of vitamin D deficiency and correlation of serum vitamin D with cardiovascular risk in patients with metabolic syndrome. Metabolic Syndrome and Related Disorders, 15(5), 213-219. Web.
Baker, J. F., Mehta, N. N., Baker, D. G., Toedter, G., Shults, J., Von Feldt, J. M., & Leonard, M. B. (2012). Vitamin D, metabolic dyslipidemia, and metabolic syndrome in rheumatoid arthritis. The American Journal of Medicine, 125(10), 1036-e9. Web.
Barbalho, S.M., Tofano, R.J., de Campos, A.L., Rodrigues, A.S., Quesada, K., Bechara, M.D., de Alvares Goulart, R., Oshiiwa, M. (2018). Association between vitamin D status and metabolic syndrome risk factors.Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 12(4), 501-507. Web.
Ferreira, P. P., Cangussu, L., Bueloni-Dias, F. N., Orsatti, C. L., Schmitt, E. B., Nahas-Neto, J., & Nahas, E. A. P. (2020). Vitamin D supplementation improves the metabolic syndrome risk profile in postmenopausal women. Climacteric, 23(1), 24-31. Web.
Fu, J., Han, L., Zhao, Y., Li, G., Zhu, Y., Li, Y., Li, M., Gao, S., & Willi, S.M. (2019). Vitamin D levels are associated with metabolic syndrome in adolescents and young adults: The BCAMS study. Clinical Nutrition, 38(5), 2161-2167. Web.
Kelishadi, R., Salek, S., Salek, M., Hashemipour, M., & Movahedian, M. (2014). Effects of vitamin D supplementation on insulin resistance and cardiometabolic risk factors in children with metabolic syndrome: A triple-masked controlled trial. Jornal de Pediatria, 90(1), 28-34. Web.
Makariou, S. E., Elisaf, M., Challa, A., Tentolouris, N., & Liberopoulos, E. N. (2017). No effect of vitamin D supplementation on cardiovascular risk factors in subjects with metabolic syndrome: A pilot randomised study. Archives of Medical Sciences. Atherosclerotic Diseases, 2, e52. Web.
Salekzamani, S., Mehralizadeh, H., Ghezel, A., Salekzamani, Y., Jafarabadi, M. A., Bavil, A. S., & Gargari, B. P. (2016). Effect of high-dose vitamin D supplementation on cardiometabolic risk factors in subjects with metabolic syndrome: A randomized controlled double-blind clinical trial.Journal of Endocrinological Investigation, 39(11), 1303-1313. Web.
Schmitt, E. B., Nahas-Neto, J., Bueloni-Dias, F., Poloni, P. F., Orsatti, C. L., & Nahas, E. A. P. (2018). Vitamin D deficiency is associated with metabolic syndrome in postmenopausal women. Maturitas, 107, 97-102. Web.
Skaaby, T., Husemoen, L. L. N., Pisinger, C., Jørgensen, T., Thuesen, B. H., Fenger, M., & Linneberg, A. (2012). Vitamin D status and changes in cardiovascular risk factors: A prospective study of a general population.Cardiology, 123(1), 62-70. Web.
Wang, Y., Si, S., Liu, J., Wang, Z., Jia, H., Feng, K., Sun, L., & Song, S. J. (2016). The associations of serum lipids with vitamin D status.PLoS One, 11(10), e0165157. Web.
Wenclewska, S., Szymczak-Pajor, I., Drzewoski, J., Bunk, M., & Śliwińska, A. (2019). Vitamin D supplementation reduces both oxidative DNA damage and insulin resistance in the elderly with metabolic disorders. International Journal of Molecular Sciences, 20(12), 2891. Web.
Wieder-Huszla, S., Jurczak, A., Szkup, M., Barczak, K., Dołęgowska, B., Schneider-Matyka, D., Owsianowska, J., & Grochans, E. (2019). Relationships between vitamin d3 and metabolic syndrome.International Journal of Environmental Research and Public Health, 16(2), 175. Web.