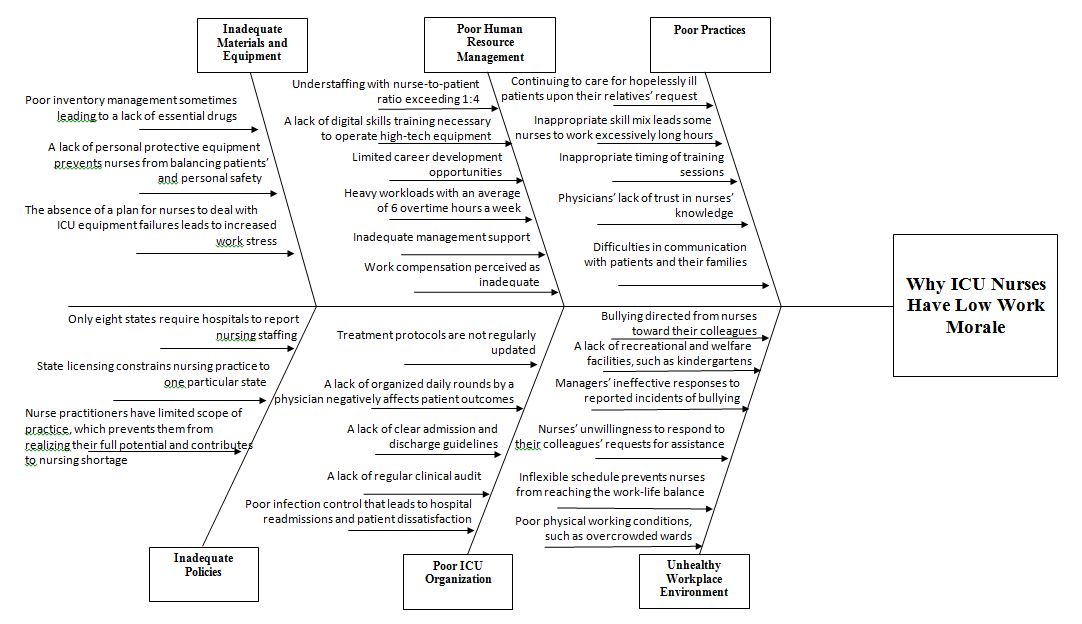
The diagram above analyzes the root causes of the low work morale of nurses working in the intensive care unit (ICU) at the hospital where I am employed. It shows six main reasons underlying nurses’ low morale: inadequate materials and equipment, poor HR management, poor practices, unhealthy workplace environment, poor ICU organization, and inadequate policies. Each of these causes contains several details that explain what constitutes a particular cause.
The first cause leading to nurses’ low work morale is inadequate materials and equipment. According to the diagram, this cause includes such factors as poor inventory management, a lack of personal protective equipment, and the absence of a plan for dealing with equipment failure. Each of these factors affects nurses’ morale by increasing their work stress. They experience moral distress when they lack the essential drugs for treating critically ill patients, cannot protect themselves from becoming infected or do not know what to do when the equipment malfunctions. The second cause is a more global one – inadequate policies at the country’s level. For example, currently, only eight states require hospitals to report their nursing staffing levels (de Cordova et al., 2019). Further, nurses’ licenses confine them to the state that issued their licenses, and nursing practitioners have a limited scope of practice despite their advanced knowledge. All these policies contribute to the problem of a nursing shortage, which, in its turn, exerts pressure on nurses, decreasing their work morale.
The third cause of nurses’ low morale is poor human resource management, comprising six elements. Among them, understaffing and heavy workloads result in significant nurses’ stress as they have to work long hours to provide care to the number of patients that exceeds the required nursing-patient ratio. These factors also lead nurses to perceive their compensation as inadequate, which, coupled with limited career development opportunities, may result in turnover intentions. A lack of digital skills training prevents nurses from effectively operating complicated ICU equipment, and insufficient management support may decrease nurses’ commitment to the profession. The fourth cause is the poor organization of the ICU. As is seen from the diagram, the ICU in this hospital lacks several significant guidelines, protocols, and procedures. It leads to an increased degree of uncertainty in the nursing practice. With not knowing what their organization expects them to do under certain circumstances, nurses become dissatisfied with their job.
The fifth cause is an unhealthy workplace environment, which includes both physical and psychological dimensions. In particular, there are cases of bullying and a lack of managers’ response to reported bullying incidents, which negatively affect the work morale of the victims of bullying. Further, a lack of welfare and recreational facilities and inflexible schedules negatively affect nurses’ morale by preventing them from reaching the right work-life balance.
Finally, the sixth cause is poor practices that are common in the ICU in this hospital. One important practice affecting nurses’ morale is continuing to provide care to hopelessly ill patients upon their relatives’ request. Nurses perceive such care as futile, which results in their moral distress and requires psychological interventions to help them cope with such situations (Asayesh et al., 2018). Inappropriate timing for training sessions means that nurses are asked to attend training while they are providing care to critically ill patients. It leads to their dissatisfaction because they have to skip the training as caring for the patient is more important. Further, physicians’ lack of trust in nurses’ skills undermines nurses’ professional identity, which also leads to decreased work morale. While each cause has to be addressed to increase nurses’ morale, poor practices seem to be changed more easily because they require interventions at the hospital’s management level.
References
Asayesh, H., Mosavi, M., Abdi, M., Masoud, M. P., & Jodaki, K. (2018). The relationship between futile care perception and moral distress among intensive care unit nurses. Journal of Medical Ethics and History of Medicine, 11, 2.
de Cordova, P. B., Pogorzelska-Maziarz, M., Eckenhoff, M. E., & McHugh, M. D. (2019). Public reporting of nurse staffing in the United States.Journal of Nursing Regulation, 10(3), 14–20. Web.