- Neurological disorder common for older population.
- A “cognitive impairment in at least two domains interfering with activities of daily living” (Waldemar & Burns, 2016, p.1).
- A form of dementia.
- Confusing cognitive and behavioral symptoms.
- Disorder with multifactorial nature (Castrillo & Oliver, 2016).
Alzheimer’s Disease is a form of dementia characterized with cognitive impairment. It was first described in 1906 by Alois Alzheimer who presented his observations of the patient with dementia. Castrillo and Oliver (2016) believe that AD develops as a result of combining such factors as genomic, environmental, and epigenomic. The disease is characterized with asymmetric cognitive decline. The process of diagnosing is complicated due to the variety of symptoms that develop individually and are usually revealed after neuropathological changes happen (Lazarov & Tesco, 2016).
Alterations associated with Alzheimer’s Disease
- Cognitive changes:
- Progressive loss of episodic memory;
- Visuospatial deficiency;
- Decline of executive functions.
- Behavioral changes:
- Hallucinations;
- Agitation;
- Delusions;
- Sleep disturbances;
- Depression;
- Distractibility;
- Apathy;
- Wandering (Waldemar & Burns, 2016).
AD is associated with different changes, both cognitive and behavioral. A patient can observe some or all of them depending on the development of the disease. One of the major cognitive symptoms is the loss of episodic memory that is progressing. At the same time, the old memories are rarely affected. Another change typical for AD includes visuospatial deficits. It makes people with AD feel unsafe in new locations. Behavioral alterations are the most frequent. Moreover, these alterations progress in the course of the disease development. Both cognitive and behavioral changes decrease the quality of life of patients with AD and often their relatives.
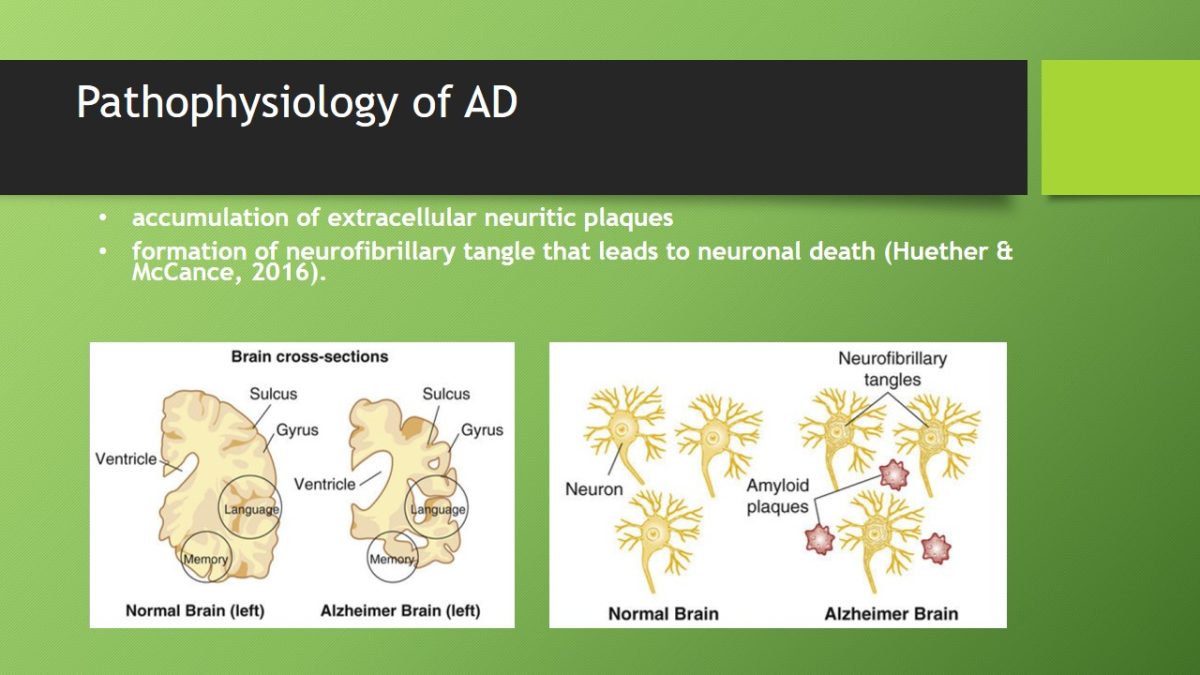
Pathophysiology of AD
- Accumulation of extracellular neuritic plaques.
- Formation of neurofibrillary tangle that leads to neuronal death (Huether & McCance, 2016).
The researchers still argue concerning the cause of AD. However, there are some pathophysiological processes that are linked to the development of the disease. Thus, DNA methylation is considered to be an epidemic marker for AD (Hammer & McPhee, 2014). Pathologic changes in the brain include “accumulation of extracellular neuritic plaques” that contain a core of amyloid beta protein, “intraneuronal neurofibrillary tangles, and degeneration of basal forebrain cholinergic neurons with loss of acetylcholine” (Huether & McCance, 2016, p. 1110). The accumulation of toxic fragments of amyloid beta protein condition the formation of “diffuse neuritic plaques, disruption of nerve impulse transmission, and death of neurons” (Huether & McCance, 2016, p. 1110). The loss of neurons in its turn causes brain atrophy. Finally, these processes result in memory and attention decline, and deterioration of other cognitive functions.
Changes in body systems
- Central nervous system: problems with learning and memory; decline of intellectual function, loss of the sense of self.
- Digestive system: problems with swallowing, frequent choking, sense of smell impairment, possible problems with bowel control, fecal incontinence.
- Neuromuscular system: weak muscle control, loss of ability to walk, rigidness of muscles, frequent accidental injuries.
AD mainly influences the nervous system. At early stages, it reveals itself in the decline of intellectual function and can develop into the complete loss of self in the late stages of the disease. Some changes also occur in the digestive system. They are related to inability to swallow. Because of it, food and drinks sometimes get into the airways that can cause pneumonia. Finally, changes in neuromuscular system lead to the walking disability.
Factors influencing the pathophysiology of the alterations
- Genetics: increased risk for people with family history of AD.
- Gender: women at higher risk than men.
- Ethnicity: higher risk of AD for African Americans.
- Age: AD prevalence increases among older people.
- Behavior: active lifestyles decrease the risk of AD.
The pathophysiological changes characteristic of AD depend on some factors such as genetics, gender, ethnicity, age, and behavior. For example, they are more likely to develop in case a person has AD in the family history. Also, the incidence of pathophysiological alterations increases with aging. Moreover, women are at higher risk of developing pathophysiological changes as well as African Americans or Hispanics if compared to men and other ethnicities correspondently. However, moderate physical activity can be one of the preventive factors for AD.
Factors influencing diagnosis
- Timely detection of symptoms.
- Comorbid diseases with similar symptoms.
- Misinterpretation of cognitive symptoms.
- Lack of doctor’s competence in AD diagnosing.
AD diagnosing is a complex intervention. It is important to assess the condition of the patient according to dementia criteria. One of the major challenges is the detection of symptoms. If the clinical manifestations of AD are defined correctly, the probability of the correct diagnosis increases. Another problem is related to diseases or other conditions with similar symptoms such as depression, delirium, or substance abuse. Cognitive symptoms can be misinterpreted, or considered to be normal changes or side effects of some medications. Finally, there is the risk that a physician is not enough experienced to detect AD symptoms and provide a proper examination and laboratory tests.
Factors influencing treatment
- Early detection.
- Timely medication to maintain mental function.
- Treatment compliance.
- Management of behavioral symptoms.
- Individual peculiarities of AD development.
- Support of families and caregivers (National Institute of Aging, n.d.).
The success of AD treatment depends on some factors. Early detection of the disorder is a decisive factor in treatment. Although AD cannot be cured, prescription of medication to support mental function and interventions aimed at management of behavioral symptoms can reduce the severity of symptoms and improve the quality of life. The peculiarities of AD development are also significant. In case of rapid progression, treatment can be less efficient. Finally, the ability of family members or other caregivers to provide the necessary care for patients with AD determines the patient outcomes as well.
Mind Map
Alzheimer’s Disease:
- PATHOPHYSIOLOGY:
- accumulation of extracellular neuritic plaques;
- formation of neurofibrillary tangle that leads to neuronal death (Huether & McCance, 2016).
- RISK FACTORS:
- Older age;
- Heart disease;
- High blood pressure;
- High cholesterol;
- Diabetes.
- TREATMENT:
- Pharmacological treatment;
- Appropriate nutrition;
- Management of behavioral symptoms;
- Participation of family members or caregivers.
- DIAGNOSIS:
- Interviewing a patient and caregiver;
- Physical and neurological observation;
- Cognitive tests;
- Psychiatric assessment;
- Brain investigation.
- CLINICAL PRESENTATION:
- Loss of episodic memory;
- Visuospatial deficiency;
- Decline of executive functions;
- Hallucinations;
- Agitation;
- Delusions;
- Sleep disturbances;
- Depression;
- Distractibility;
- Apathy;
- Wandering.
- EPIDEMIOLOGY:
- Over 44 million people with dementia in the world;
- More that half of dementias are AD;
- World prevalence 5-7%;
- Incidence increases with older age;
- Mostly affects people from 65 to 90.

References
- Castrillo, J.I., & Oliver, S.G. (Eds.). (2016). System biology of Alzheimer’s disease. New York, NY: Humana Press.
- Hammer, G.D., & McPhee, S.J. (2014). Pathophysiology of disease: An introduction to clinical medicine (7th ed.). New York, NY: McGraw Hill Education.
- Huether, S.E., & McCance, K.L. (2016). Understanding pathophysiology (6th ed.). St. Louis, MO: Elsevier.
- Lazarov, O., & Tesco, G. (Eds.). (2016). Genes, environment and Alzheimer’s disease. San Diego, CA: Elsevier.
- National Institute of Aging. (n.d.). Alzheimer’s disease fact sheet. Web.
- Waldemar, G., & Burns, A. (Eds.). (2016). Alzheimer’s Disease (2nd ed.). Oxford, UK: Oxford University Press.