Introduction
Osteoarthritis/ degenerative joint disease is a “chronic condition characterized by deterioration of joint cartilage and the formation of reactive new bone at the margins and sub-chondral areas of the joints” (Schilling, 2010, p. 388). Rheumatoid arthritis is a “chronic systemic inflammatory arthritis of auto-immune origin, and it systematically affects the synovial joints” (Emery, 2011. p. 1). This paper aims at discussing the pathophysiology of the two diseases while highlighting their differences and similarities.
Pathophysiology
Osteoarthritis
As can be seen from the definition of osteoarthritis above, the major issue of osteoarthritis is loss of articular cartilage at the synovial joints, presumably through enzymatic action. But, interleukin has also been suspected to cause this loss. As the cartilage erodes with time, the underlying bone is exposed and left unprotected. Sequentially, thickening and hardening (sclerosis) of the exposed bone results. Gross alteration occurs at the joints, where damage is evident, from formation of fibrotic synovial lining that impedes mobility, and in some occasions, the synovial fluid may defect to form cysts. In addition, there is formation of new bone called osteophyte (bone spur).
Rheumatoid Arthritis
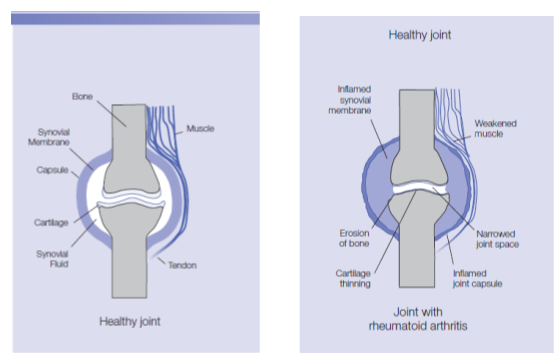
Depending on the causative factor, the pathogenesis of disease may take a slightly different course. While genetic mutation at the human leukocyte antigen locus and the presence of auto-antibodies alter the structure of joint formation, environmental factors may later joint formation in a different way. The figure below shows the difference between a healthy joint and one with rheumatoid arthritis.
Factors
Genes
A genetic link to rheumatoid arthritis is confirmed by observations made between monozygotic and dizygotic twins in reference to the disease. Rheumatoid arthritis is attributed to specific alleles prevailing at the human leukocyte antigen (HLA)-BRBI locus alongside auto-antibodies: the rheumatoid factor and anti-cyclic citrullinated peptide. Genetic disorders, such as hyperparathyroidism, are strongly linked to arthritis because they can initiate and speed up cartilage breakdown and inflammation of the synovial joints. Genetic disposition that inhibits the synthesis of collagen is associated with osteoarthritis
Environmental factors
These factors cause inflammation of the synovium, which results in synovitis and joint destruction.
Similarities
Age and disability
Both diseases cause disability. Both diseases begin during the middle ages and progress into old age. As the synovium deteriorates, disability sets in, and mobility is reduced within an individual.
Etiology
Some risk factors are responsible for the occurrence of both diseases. For example, both diseases are genetically susceptible and are both attributed to environmental factors, especially obesity.
Differences
Etiology
Rheumatoid arthritis is associated with other causative factors that are not associated with osteoarthritis, and the converse is the case. While the Epstein-Barr virus is associated with rheumatoid arthritis, chemicals such as steroids are only attributed to osteoarthritis (Emery, 2011; Schilling, 2010).
Incidence
There is variation in different reports regarding the most common arthritis, but most reports indicate that osteoarthritis is the most common (Fidelix, Macedo, Maxwell & Fernandes, 2014). Rheumatoid arthritis affects 0.5% to 2% of the entire worldwide population. On the other hand, osteoarthritis affects 10% of the world’s population.
Diagnosis
Magnetic resonance imaging is used to indicate any abnormalities in the bony and soft tissues. Increased erythrocyte sedimentation is attributed to injury on the synovium. X-rays are another procedure used to view any joint deformity, joint fusion or bony growths. Clinical assessment, laboratory tests and X-rays are used to diagnose rheumatoid arthritis.
Treatment
Treatment for both rheumatoid arthritis and osteoarthritis is the same. It entails weight management, creating a balance between rest and exercise, use of medication such as cox-2 inhibitors, join care and stabilization using clutches, and in severe cases, surgery may be performed.
Conclusion
Arthritis is a debilitating disease that is treatable with the aim of managing symptoms, but it has no cure. No specific cause is associated with the occurrence of arthritis, but a multifactorial complex is associated with the disease.
References
Australian Government: Department of Health and Ageing. (2009). A picture of rheumatoid arthritis in Australia. Canberra: Australian Institute of Health and Welfare.
Emery, P. (2011). Pocket Reference to Early Rheumatoid Arthritis. London: Springer Healthcare.
Fidelix, T., Macedo, C., Maxwell, L., & Fernandes, M. (2014). Diacerein for osteoarthritis. COCHRANE SUMMARIES. Web.
Schilling, J. (2010). Professional Guide to Pathophysiology (3rd ed.). Ambler: Lippincott Williams & Wilkins.