Case Study
Steven is a forty-three-year-old American male that has lived alone in his house for more than ten years. He has a longstanding diagnosis of bipolar disorder which was diagnosed in the patient fifteen years ago. The individual has been admitted to several mental health rehabilitation centers after the episodes of severe depression and the related suicidal thoughts and one attempt. Steven is divorced, and his condition was among the causes of the split with his wife. The analysis of Steven’s case is based on Clark and Clarke’s (2014) biopsychopharmacosocial (BPPS) approach to psychiatric nursing, which entails the promotion of patient-centered care and planning by exploring the relevant areas of influence.
Biological
The physical health of Steven requires the management of a range of comorbidities. Over a decade ago, he was diagnosed with liver disease, which runs in his family. However, his lifestyle and unhealthy dietary choices have certainly contributed to the diagnosis. It is crucial to managing Steven’s liver damage because of the possibility to result in scarring and subsequent liver failure, which is a life-threatening condition (Osna et al., 2017). To manage the condition, Steven has been prescribed medications, but he has often failed to take them because his psychological health was debilitating.
Psychological
The patient’s mental health negatively influences his quality of life. Specific triggers for both manic and depressive symptoms include prolonged alcohol use, loneliness, and stressful events. The patient’s bipolar disorder is characterized by the prevalent occurrence of depressive features with a less lasting presence of ‘low’ episodes (Bobo, 2017). Steven’s bipolar disorder-related depressive symptoms manifest through the decreased appetite to the point of not eating anything for several days. The patient has also experienced extreme fatigue and low energy alongside feelings of hopelessness, despair, guilt, and worthlessness (Koenders et al., 2020). At present, Steven has been prescribed the atypical antipsychotic lurasidone (Latuda) in combination with Lithium to treat his symptoms of bipolar depression (Ostacher et al., 2017).
The manic episodes in Steven’s case are characterized by racing thoughts, increased agitation and activity, as well as the decreased need for sleep to the point of not sleeping for forty-eight hours and more (WHO, 2019). In addition, the patient reported having poor decision-making during his manic episodes. Steven also reported distorted sleeping patterns as one of the most consistent and long-term symptoms of bipolar disorder (Gold & Sylvia, 2016). Disruptions in his sleep have been directly associated with either high or low episodes. When Steven experiences manic episodes, his sleep patterns change to the opposite. The extreme levels of energy and racing thoughts make it difficult for him to fall asleep to the point that he has to take medication that would allow him to have some sleep.
Steven has been known to be harmful toward himself during depressive bipolar disorder episodes. During a severe ‘low,’ Steve drank a bottle of vodka and got to a high floor in his apartment complex, and stood on the ledge of a balcony for several minutes before his neighbor noticed him and pulled him from the dangerous spot. Such behavior is troubling because individuals with BD are at high risk for suicide, especially if their condition remains untreated (Dome, Rihmer, & Gonda, 2019).
The patient has had some experience with receiving mental health services acutely. He was admitted to a mental health ward after attempting to jump off a balcony during a depressive episode. Steven was prescribed medication and referred to a mental health specialist, but he failed to continue his care on a long-term basis because the manic episode gave him the sense of confidence that he was fine, even when he was not. However, without consistent support, therapy, and medication, Steven finds himself spiraling into severe depression after a manic episode and the related comorbidities (Post, 2020).
Pharmacological
From the pharmacological perspective, Steven has shown several side effects from the prescribed medication. During the first years after the initial diagnosis of bipolar disorder, Steven has been prescribed an antidepressant (Lexapro) to manage his ongoing depressive symptoms. However, there have been limited results with the prescription because of its varied effectiveness for bipolar depression (Jelen & Young, 2020). Lexapro was a mistake in prescription in Steven’s case because the medication is recommended not to be given as a monotherapy option in individuals with bipolar (Yamaguchi et al., 2018). Taking antidepressants for several years has resulted in Steven developing more pronounced and severe episodes of mania.
After the failure with taking antidepressants, Steven was prescribed a mood stabilizer Lithobid, 300 mg per day. After taking Lithium for some time, Steven realized that the medication was more effective in treating his manic episodes rather than depressive ones (Gitlin, 2016). This resulted in the furthering of the depressive symptoms and increased suicidal ideation, which led to a suicide attempt by trying to jump from a balcony of his apartment building. After being admitted to an acute psychiatric facility, Steven received an adjusted medication prescription which included a combination of a mood stabilizer and an atypical antipsychotic drug.
Over time, Steven has found it more challenging to manage his condition with medication. Lithium has taken a toll on Steven in terms of his physical health as it has resulted in persistent headaches, dizziness, appetite changes, hand tremors, as well as occasional nausea and vomiting (Ortiz & Alda, 2010). The prescription of lithium in Steven’s case has been problematic because of his liver disease. As Carrier et al. (2016) and Culpepper (2014) found in patients with advanced chronic liver diseases, the prescription of specific psychiatric treatments should be avoided. The fact that Steven has already had liver disease before being diagnosed with bipolar I disorder should be considered in the further recommendations concerning his treatment.
Before being diagnosed with bipolar disorder, Steven had frequently used alcohol as a means of coping with his depressive state. He did not understand that he was experiencing a bipolar ‘low’ and considered his feelings sadness and anxiety and wanted to numb them with the help of alcohol (Johnson, 2018). When Steven was in an elevated mood, he felt that alcohol would help him stay active and excited. However, overusing alcohol during the periods of ‘highs’ led to Steven falling back into a depressive state quickly (WHO, 2019). Taking medicines for bipolar disorder with alcohol can exacerbate adverse side effects such as dizziness, the impairment of memory, confusion, as well as increased risks for falls and injury (Anderson, 2019).
Social
Steve currently lives alone and has lived alone for quite some time because of the divorce. He does not hold any aggression toward his former wife and blames all bad events on himself and his inability to take the situation under control. He has no siblings and very few friends, spending most of his time at home. The social isolation has caused some issues in his mental state and the worsening of depressive symptoms because there is no one there to offer help or support. Steve’s former wife calls him occasionally to remind him to take his medication.
Being on his own and having a weak support system makes Steve consider suicide during his depressive episodes. COVID-19 and the associated lockdown orders have reduced the social interaction Steven gets further, creating conditions of extreme isolation for him. As Pfefferbaum and North (2020) note, the pandemic has had substantial negative effects on people’s mental health overall, with those most vulnerable affected especially strongly. Due to lacking social support, the patient sees alcohol use as the answer to loneliness and as a way to uplift one’s spirits (Brooks et al., 2017). He quit his office job and has worked remotely since the symptoms have become debilitating. However, being alone at home meant that Steven had less structure in his life, which reduced stress and social responsibility; however, it furthered his depressive episodes (Dome et al., 2019).
Critique of the BPPS Model
While the BPPS model has found widespread adoption in healthcare, it has some substantial issues that its critics frequently highlight. One position aims to expand the model, with its adherents stating that its lack of a spiritual domain reduces its effectiveness. They claim that, since one’s spirituality substantially affects their beliefs on matters such as hope or suicide, it has to be explicitly included in the analysis. The opposite perspective is outlined by Huda (2019), with its proponents criticizing the nonscientific nature of the BPPS model. They state that it is poorly defined, complicating analytic understanding through the introduction of vaguely related perspectives and their equal consideration, which in practice is not always substantiated. As a result, it is possible for the model’s user to become distracted by minor facts and misunderstand the patient’s condition.
Mental State Examination
- Level of consciousness: normal.
- Appearance and General Behavior: the patient looks older than their stated age due to the poor visible condition of their skin. He is unkempt, likely due to his tendency not to leave his house and generally antisocial patterns of behavior. The patient’s clothing is subdued and dirty, his posture is kyphotic, and his gaze is furtive.
- Speech and Motor Activity: no problems with output or articulation, no signs of mania being shown currently. Movement is slow and non-spontaneous, likely as a result of the patient experiencing a “low” at the moment.
- Affect and Mood: affect is restrained, with the patient showing limited emotional responses. The overall mood is negative and dysphoric in its overall nature, indicative of a depressive condition.
- Thought and Perception: the patient does not exhibit signs of a thought disorder. His ideas appear to be realistic and rooted in events he has experienced. His concerns are realistic, though his condition sometimes elevates them to irrational levels.
- Attitude and Insight: the patient demonstrates a highly pessimistic attitude, claiming that he has already tried all he could and that it has not helped. This experience also leads him to demonstrate signs of helplessness and surrender to his condition. He views the illness as nonpsychiatric, considering it the result of his failures in life as well as alcoholism.
- Examiner’s Reaction: examiner felt that the patient was not particularly unusual, exhibiting the standard signs of depression. With that said, they expect that the patient may show a different response if examined during a manic episode.
- Cognitive Abilities:
- Attention: the patient has somewhat diminished reaction speed and ability to memorize sequences of letters. However, the abnormality is not large and can be attributed to his alcohol abuse.
- Language: no visible issues. The patient has passed both speaking and comprehension tests without much difficulty.
- Memory: the patient has complained of memory loss episodes, mostly related to alcohol binge drinking. Other than that, their short- and long-term retention appear to be at levels that are close to optimal.
- Constructional Ability and Praxis: while the patient is experiencing tremors, they do not impede him from performing learned motor acts. They do not suffer from a constructional inability or other mental impediments in this regard, either.
- Abstract Reasoning: the patient is experiencing few to no issues with his abstract reasoning. Tests have shown that it is functioning normally, and the patient’s overall presentation supports this conclusion.
Care Plan Commentary
Steven’s case calls for a comprehensive and rigorous overhaul of the. The plan is patient-focused and was developed through collaboration with Steven who identified his needs in terms of his areas of influence (Gliedt et al., 2017). It also follows guidelines by the National Institute of Health and Cares Excellence (2016), which demand adherence to person-centered and recovery-focused care in all aspects of nurse training and work. The nurse acted as the liaison between the patient and the various medical professionals whose aid was required. The BPPS model used for exploring Steven’s case has provided valuable data about Steven’s prior interactions (Gliedt et al., 2017). The adverse interactions between the four areas of influence contributed to the deterioration of his psychological health as well as increased alcohol use (Carrier et al., 2016). The care plan has been made accessible and provided to Steven in both printed and digital formats (NMC, 2020). Evidence-based interventions that address the mental health issue go beyond the psychological component and also help patients deal with stigmatization and discrimination (O’Donnell et al., 2018). Drawing from the evidence provided by Smith et al. (2013), the care plan will rely on regular patient-provider relationships, with an ongoing review and assessment leading to changes if necessary. Steven has a clear understanding of the services provided to him by his healthcare team, which is essential for care continuity and patient education (NMC, 2020).
Evidence-based management of liver disease implemented is a biological intervention that includes BCAA-rich supplementation, abstinence from consuming alcohol, corticosteroid therapy, and adherence to a strict dietary regimen (Fukui et al., 2016). Steven is set to undergo regular screenings with the assigned nurse, which will liaise with an interdisciplinary team that also includes his psychotherapist, a pharmacologist, a dietician, and a social worker. The pharmacologist will review Steven’s prescriptions and adjust them if necessary (Carrier et al., 2016). The nurse will structure their interventions around therapeutic engagement, following practices such as active listening and regular devotion of time.
The role of Steven’s nurse caretaker is the regular monitoring of his vital signs, introducing monitoring charts for food and fluid intake. Steven will be subjected to the NEWS tool to monitor changes in his health. Specifically, the tool will monitor respiratory rate, oxygen saturation, body temperature, systolic blood pressure, heart rate, and BPM. The nurse will also regularly schedule liver function test screenings for the patient and attend them with Steven. In collaboration with the nurse, a dietician will develop a plan of nutrition. EBP recommendations for a liver disease-specific diet include a decreased intake of carbohydrates and high-fat foods, adequate hydration, as well as tobacco and alcohol abstinence (Arab et al., 2014). Smoking and alcohol cessation interventions will also be carried out.
A significant issue in Steven’s treatment is that he struggles with following his medication schedule despite having a monitor and with lithium level assessments. To that end, the nurse caretaker will help him develop a system that will enable him to take his medication regularly and consistently. They will educate him about the side effects and interactions of all the drugs he is currently taking or will be prescribed. Per “Lexapro side effects” (2020), the drug can commonly cause “diarrhea, drowsiness, ejaculatory disorder, headache, insomnia, nausea, and delayed ejaculation.” Lithobid, on the other hand, can result in a broad range of effects, such as fainting, thirst, weight gain, acne, diarrhea, and others, but they are less common (“Lithobid side effects,” 2020). The two drugs also interact with each other, increasing the risk of an irregular heart rhythm, and the side effects of both are exacerbated by alcohol intake (“Drug interaction report,” n.d.). Hence, Steven needs to reevaluate his drug and alcohol intake practices with the nurse caretaker’s help.
Steven has experienced a variety of lithobid side effects, which were exacerbated both by his alcohol intake and by his liver disease. Most commonly, he has had headaches, felt dizzy, and experienced hand tremors, and more rarely, he has had nausea and vomited. Since Lithobid is not recommended for his state (Carrier et al., 2016), Steven should stop taking the drug. The levels in Steven’s blood will be monitored, and the prescriptions will be regularly discussed with the pharmacist, the psychiatrist, and other nurses. It will be replaced with a more suitable pharmacological intervention should this replacement (as opposed to the removal of the drug’s intake) be necessary. The replacement drugs will be screened for side effects and interactions and adjusted in the case their usage is not acceptable. Mwebe (2018) also recommends the usage of the Glasgow Antipsychotic Side Effect Scale (GASS). Steven will also learn about the common side effects of each medication he is taking and the coping methods to use should they arise.
The nurse will carry out patient-provider meetings once every two weeks to identify the effectiveness of the sequence of therapeutic interventions and prioritize the steps based on Steven’s feedback (Smith et al., 2013). Both face-to-face and web-based CBT will be implemented to address Steven’s depression and suicidal thoughts, prevent their onset, avoid ED visits and hospitalizations linked to suicidal attempts, and decrease the medical risks of self-injurious acts (Brodsky, Spruch-Feiner, & Stanley, 2018). In addition, the CBT Readiness Assessment Tool was used, resulting in a score of 7 (based on the Likert scale between 0 and 10), indicating Steven’s higher than average level of readiness (Trusz et al., 2011).
Another significant issue Steven has is that, until recently, he did not understand the condition that he had, which resulted in him misjudging his depressive episodes and coming close to suicide as a result. To prevent the emergence of similar issues in the future, Steven will have to undergo education about his symptoms and triggers. It will be continuous and enable him to see the negative effects of his excessive alcohol intake. He will learn how to recognize the early signs of an incoming episode so that it does not take him by surprise. He will also learn the appropriate responses, such as calling the appropriate number (learning which will be part of the intervention). In addition, the patient and the caretaker will review the strategies and medications that have been successful in the past. This information can be included in Steven’s advance care plan so that his helpers know what actions to take to manage his crisis even if they are not experienced in caring for him (Nizette, O’Brien, & Evans, 2016). As a result, he will be prepared for his condition and be able to mitigate the effects of the episodes, reducing the negative effects they have on his life. Johnson (2018) also recommends the usage of a bipolar diary for the patient to document his moods. In doing so, he will be able to understand the qualities each of his moods has and control themselves better.
Examples of numbers that Steven can call for support in crises include his nurse caretaker, care coordinator, friends, family, and local crisis management hotlines. The nurse will work with Steven to develop a collaborative crisis plan per National Institute for Health and Care Excellence (2020) recommendations. Additionally, the training will focus on identifying Steven’s strengths that will let him overcome his issues internally. Per the recommendations by Kvam et al. (2016), it will recommend that he engage in exercise to help deal with his depression. The role of the nurse caretaker in this effort is to help the patient achieve personal growth and capitalize on their strengths to achieve partial or full independence (Hercelinskyj & Alexander, 2020). One example of an approach that can help Steven learn how to manage his condition is CBT, which will help him identify misconceptions and problematic thinking patterns in which he engages during critical situations. The nurse can refer Steven to a qualified therapist to perform this procedure.
Finally, the intervention will focus on Steven’s troubled sleep patterns. The nurse caretaker believes that the reason for this problem is that his daily life practices are not conducive to healthy sleep, with a variety of problematic behaviors compounding to result in serious sleep issues. Hence, he will undergo sleep hygiene education to inform him of what factors may cause him to have difficulty going to sleep and how he may address them. Per Pandi-Perumal, Narasimhan, and Kramer (2017), this learning consists of studying practices that affect sleep, such as alcohol consumption in the evening, and a review of current issues and ways to fix them with the physician. Through this holistic assessment, the patient and the caretaker will develop a comprehensive plan for addressing the former’s problems that will be integrated into the broader treatment program. Steven’s sleeping patterns will also be monitored to determine his progress in overcoming the issue, with additional reviews and interventions taking place if the current intervention is unsuccessful.
Because the patient indicated that his support system was weak, the emphasis of the nurse’s agenda is regularly reviewing Steven’s daily life in society (NMC, 2020). As suggested by Naylor et al. (2016), the integrated health approach will help individuals like Steven to improve their social, mental, and physical wellness. Evidence-based intervention for increasing social support to the patient includes reducing Steven’s social isolation through him engaging in community groups, extending social support outreach by engaging in work and hobbies, as well as facilitating self-development (O’Rourke, Collins, & Sidani, 2018). Specific hobbies that Steve will undertake include painting, yoga, and meditation. The latter two have the potential of improving his physical health and being complementary to the established mental health improvement plan (Kaushik et al., 2020).
Cognitive Behavioral Therapy Critique
The plan is extensive and likely to take a substantial time to implement, over which Steven’s progress will have to be carefully monitored. The patient will have to educate himself extensively, and the nurse will need to monitor him and act as a liaison to the other team members. There is a risk that they will not be able to devote enough time to the patient and that issues will go unnoticed. Crises are also problematic, as, without constant oversight, the patient will not necessarily be able to manage the episode alone. With that said, this plan combines mental health treatment and society reintegration best, which is why it was formulated in this form. CBT should also be approached carefully, as Townend et al. (2017) highlight its recent apparent loss of effectiveness. Steven’s readiness to engage in it is also in question, and Wenzel (2017) recommends the use of motivational interviewing before engaging in CBT. CBT is also not holistic, focusing excessively on mental processes and ignoring the social, biological, and environmental factors.
Plan of Care
Identified Needs
- Mental health needs: establish mental health at a manageable level for the patient as related to his bipolar disorder diagnosis;
- Physical health needs: manage physical comorbidities associated with bipolar medication side effects as well as the long-term diagnoses of liver disease;
- Behavioral needs: managing depression and mania as well as suicidal thoughts, prevent self-harm.
- Self-care needs: establish a cohesive self-care plan that includes dietary and lifestyle changes, smoking cessation, and mild physical activity;
- Social needs: improve socialization with friends, family, and members of the community.
SMART Goals
- Mental Health SMART Goal: To help reach a stable mental health baseline with holistic and pharmacological treatment and improve life quality despite Steven’s diagnosis.
- Physical Health SMART Goal: To enable Steven to reach the desired quality of physical health through appropriate diet and lifestyle choices, medication, and alcohol abstinence.
- Behavioral Health SMART Goal: To help Steve live with his diagnoses safely and without risks by teaching preventive measures and holistic practices for balanced behavior.
- Self-care SMART Goal: To help Steven act in his personal care, healthy lifestyle choices, and self-development.
- Social SMART Goal: To enable socialization and interactions with the outside environment by promoting independence and the strengthening of relationships.
Actions/Interventions
Mental Health (psychological)
- Closely monitor whether the patient takes the prescribed medication for the management of his bipolar diagnosis;
- Schedule therapy appointments beforehand so that Steven has a clear idea of his schedule; explain the importance of attending them regularly;
- Use frequent follow-ups and calls with Steven to facilitate close communication and monitoring of the patient’s status;
- Reduce the severity of Steven’s depressive episodes by allowing him to express his feelings and discover his triggers independently.
- Encourage Steven to participate in activities he likes and promote his integration into a social network.
Medications (pharmacological)
- Review the medications Steven is taking, determine their side effects, contraindications, and interactions.
- Replace any potentially dangerous medications with safer alternatives.
- Provide Steven with help purchasing the medications and learning how to use them.
- Establish a medication schedule and help Steven adhere to it.
Physical Health (biological)
- Ensure that the patient takes the necessary medication for managing his liver disease;
- Schedule follow-up appointments every six months to screen Steven’s liver for any further damage associated with prescription medication for bipolar disorder;
- Encourage reduction and the subsequent cessation of alcohol to improve liver health as well as prevent adverse interactions between BD medication and Steven’s liver condition.
- Discuss Steven’s attitude to eating and take his weight regularly. Consult with a psychiatrist and a dietician to monitor Steven; use food and fluid charts.
Behavior (psychological)
- Healthcare team to differentiate between Steven’s manic and depressive symptoms to understand the influence on the patient;
- Persistent and longstanding periods of depression should be monitored carefully to prevent suicidal thoughts, self-harm, as well as suicidal attempts;
- Encourage Steven to find a creative outlet in order to put his struggles in a positive direction;
- Facilitate holistic practices such as meditation, yoga, and other practices of mindfulness.
- Educate Steven about sleep hygiene and develop a plan for overcoming his issues.
Self-Care (psychological)
- Help Steven develop a personalized and comprehensive self-care plan that involves a sleeping schedule, a diet and exercise program, and a schedule of taking prescription medication.
- Remind Steven of the regular therapy visits as well as any other check-ups and follow-ups.
- Ensure that Steven follows the plans and reports any challenges in compliance with his physician.
- Educate Steven about his symptoms and how to manage them by giving him crisis and GP numbers.
Social
- Help Steven find value in social interactions by enabling him to communicate with people more and share his struggles with others;
- Enable participation in support groups for individuals with mental health diagnoses
- Encourage reconnecting with old friends, colleagues, and family members to establish a robust support system.
Contingency Plan for a Crisis
- It is recommended to implement the following steps in case of a crisis relapse associated with a suicide attempt during a depressive episode.
- Control correct and appropriate administration of medication for bipolar disorder;
- Get the patient under the surveillance of healthcare specialists or in a designated mental health setting;
- Refer to a therapeutic professional, such as psychologist and psychiatrist;
- If mental health continues deteriorating, consider admitting Steven to an inpatient facility for continuous monitoring and therapeutic processes.
Risk Assessment
High
- History of suicidal ideation and attempts: therapy, community support groups, environmental safety controls, regular follow-ups, and check-ins;
Moderate
- Increased alcohol use: replacement therapy, community support groups, a lifestyle and dietary change plan;
- Risks of liver disease exacerbation: encouraging a healthy lifestyle change, a cohesive diet plan, alcohol use cessation;
- Risks of physical exhaustion: facilitating a healthy sleeping schedule, the introduction of mild exercises;
- Loneliness and isolation: participating in social activities, creating a support network for him;
Low
- Causing harm to others: therapy, ongoing monitoring of the mental state, improved quality of interactions with friends and relatives;
- Risk of injury: appropriate medication concordance.
Potential
- Liver disease exacerbation: implementing regular and effective screening for viral hepatitis and steatohepatitis; lifestyle and dietary adjustments;
- Absence of motivation and interest in life: encouraging taking up hobbies, engaging in volunteering, seeking community support, setting short-term goals.
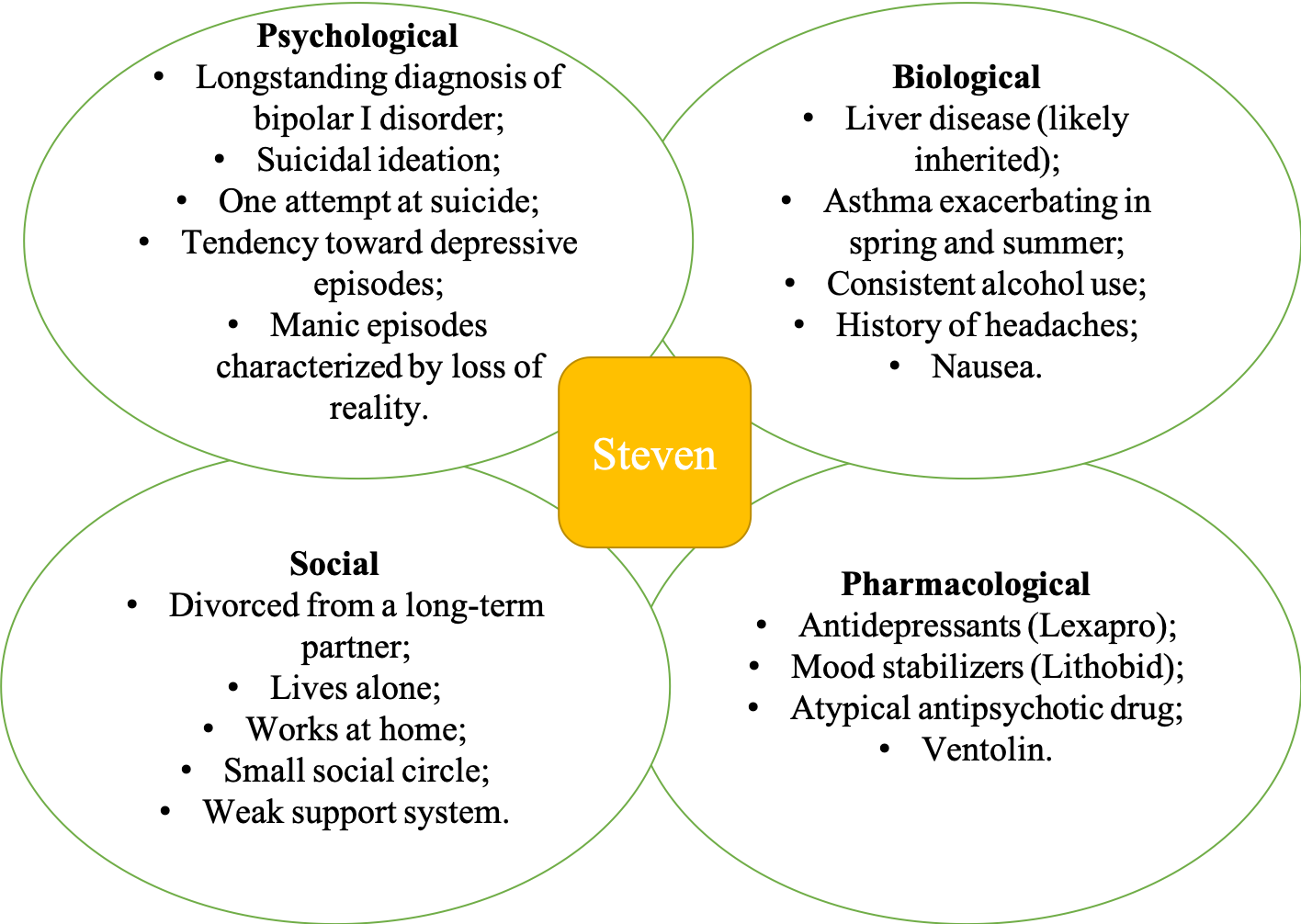
BPPS Diagram
References
Arab, J. P., Candia, R., Zapata, R., Muñoz, C., Arancibia, J. P., Poniachik, J., Soza, A., Fuster, F., Brahm, J., Sanhueza, E., Contreras, J., Cuellar, M. C., Arrese, M., & Riquelme, A. (2014). Management of nonalcoholic fatty liver disease: An evidence-based clinical practice review.World Journal of Gastroenterology, 20(34), 12182-12201. Web.
Bobo, W. (2017). The diagnosis and management of bipolar I and II disorders: Clinical practice update.Mayo Clinical Proceedings, 92(10), 1532-1551. Web.
Brodsky, B. S., Spruch-Feiner, A., & Stanley, B. (2018). The zero suicide model: Applying evidence-based suicide prevention practices to clinical care.Frontiers in Psychiatry, 9, 33. Web.
Brooks, A. T., Lòpez, M. M., Ranucci, A., Krumlauf, M., & Wallen, G. R. (2017). A qualitative exploration of social support during treatment for severe alcohol use disorder and recovery.Addictive Behaviors Reports, 6, 76-82. Web.
Carrier, P., Debette-Gratien, M., Girard, M., Jacques, J., Nubukpo, P., & Loustaud-Ratti, V. (2016). Liver illness and psychiatric patients.Hepatitis Monthly, 16(12), e41564. Web.
Clark, L., & Clarke, T. (2014). Realizing nursing: A multimodal biopsychopharmacosocial approach to psychiatric nursing.Journal of Psychiatric and Mental Health Nursing, 21(6), 564-571. Web.
Culpepper L. (2014). The diagnosis and treatment of bipolar disorder: Decision-making in primary care.The Primary Care Companion for CNS Disorders, 16(3), PCC.13r01609. Web.
Dome, P., Rihmer, Z., & Gonda, X. (2019). Suicide risk in bipolar disorder: A brief review.Medicina (Kaunas, Lithuania), 55(8), 403. Web.
Drug interaction effects. (n.d.). Web.
Gitlin, M. (2016). Lithium side effects and toxicity: Prevalence and management strategies.International Journal of Bipolar Disorders, 4(1), 27. Web.
Gliedt, J., Schneider, M., Evans, M., King, J., & Eubanks Jr., J. (2017). The biopsychosocial model and chiropractic: A commentary with recommendations for the chiropractic profession.Chiropractic & Manual Therapies, 25(16). Web.
Gold, A. K., & Sylvia, L. G. (2016). The role of sleep in bipolar disorder.Nature and Science of Sleep, 8, 207-214. Web.
Hercelinskyj, G., Alexander, L. (2019). Mental health nursing: Applying theory to practice. Melbourne, Australia: Cengage Learning Australia.
Huda, A. S. (2019). The medical model in mental health: An explanation and evaluation. Oxford University Press.
Jelen, L., & Young, A. (2020). The treatment of bipolar depression: Current status and future perspectives.Current Behavioral Neuroscience Reports, 7, 1-4. Web.
Johnson, J. (2018). How does alcohol affect bipolar disorder? Web.
Johnson, S. L. (2017). Therapist’s guide to clinical intervention: The 1-2-3’s of treatment planning (3rd ed.). Elsevier Science.
Kaushik, M., Jain, A., Agarwal, P., Joshi, S. D., & Parvez, S. (2020). Role of yoga and meditation as complimentary therapeutic regime for stress-related neuropsychiatric disorders: Utilization of brain waves activity as novel tool.Journal of Evidence-Based Integrative Medicine. Web.
Koenders, M., Dodd, Al., Karl, A., Green, M., Elzinga, B., & Wright, K. (2020). Understanding bipolar disorder within a biopsychosocial emotion dysregulation framework.Journal of Affective Disorders Reports, 2, 100031. Web.
Kvam, S., Kleppe, C. L., Nordhus, I. H., & Hovland, A. (2016). Exercise as a treatment for depression: a meta-analysis. Journal of Affective Disorders, 202, 67-86.
Lexapro side effects. (2020). Web.
Lithobid side effects. (2020). Web.
Mwebe, H. (2018). Psychopharmacology: A mental health professionals guide to commonly used medications. Critical Publishing.
National Institute of Health and Care Excellence. (2016). Transition between inpatient mental health settings and community or care home settings. Web.
National Institute of Health and Care Excellence. (2020). Bipolar disorder: Assessment and management. Web.
National Institute of Mental Health. (2017). Bipolar disorder. Web.
Naylor, C., Das, P., Ross, S., Honeyman, M., Thompson, J., & Gilburt, H. (2016). Bringing together physical and mental health: A new frontier for integrated care. Web.
Nizette, D., O’Brien, A., & Evans, K. (2016). Psychiatric & mental health nursing (4th ed.). Chatswood, Australia: Elsevier Health Sciences.
NMC. (2020). Professional standards of practice and behavior for nurses, midwives and nursing associates. Web.
O’Donnell, L., Himle, J. A., Ryan, K., Grogan-Kaylor, A., McInnis, M. G., Weintraub, J., Kelly, M., & Deldin, P. (2017). Social aspects of the workplace among individuals with bipolar disorder.Journal of the Society for Social Work and Research, 8(3), 379-398. Web.
O’Rourke, H. M., Collins, L., & Sidani, S. (2018). Interventions to address social connectedness and loneliness for older adults: A scoping review.BMC Geriatrics, 18(1), 214. Web.
Ortiz, A., & Alda, M. (2010). Treatment of bipolar disorder with comorbid migraine.Journal of Psychiatry & Neuroscience: JPN, 35(1), E1-E2. Web.
Osna, N. A., Donohue, T. M., Jr, & Kharbanda, K. K. (2017). Alcoholic liver disease: pathogenesis and current management. Alcohol Research: Current Reviews, 38(2), 147-161.
Ostacher, M., Ng-Mak, D., Patel, P., Ntais, D., Schlueter, M., & Loebel, A. (2018). Lurasidone compared to other atypical antipsychotic monotherapies for bipolar depression: A systematic review and network meta-analysis.The World Journal of Biological Psychiatry, 19(8), 586-601. Web.
Pandi-Perumal, S. R., Narasimhan, M., & Kramer, M. (eds.). (2017). Sleep and psychosomatic medicine. Boca Raton, FL: CRC Press.
Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510-512.
Post, R. (2020). How to prevent the malignant progression of bipolar disorder.Brazilian Journal of Psychiatry, 42(5). Web.
Smith, R., Dwamena, F., Grover, M., Coffey, J., & Frankel, R. (2013). An evidence-based patient-centered method makes the biopsychosocial model scientific. Patient Education and Counselling, 91(3), 265-270. Web.
Townend, M., Maguire, N., Stalmeisters, D., & Kingdon, D. (2017). CBT values and ethics. SAGE Publications.
Trusz, S. G., Wagner, A. W., Russo, J., Love, J., & Zatzick, D. (2011). Assessing barriers to care and readiness for cognitive behavioral therapy in early acute care PTSD interventions. Psychiatry, 74(3), 207-223.
Wenzel, A. (2017). Innovations in cognitive behavioral therapy: Strategic interventions for creative practice. Taylor & Francis.
WHO. (2019). Mental disorders. Web.
Yamaguchi, Y., Kimoto, S., Nagahama, T., & Kishimoto, T. (2018). Dosage-related nature of escitalopram treatment-emergent mania/hypomania: a case series.Neuropsychiatric Disease and Treatment, 14, 2099-2104. Web.