Design proposal introduction
- Central venous catheters (also abbreviated as CVCs) are susceptible to being colonized by various microorganisms.
- The key objective is the application of antiseptics on the patients’ skin (Bion et al., 2012).
Central venous catheters (also abbreviated as CVC) can be used to monitor health indicators and vitals in addition to regulating the intake of medication and blood products or important nutrients. The issue that will be reviewed within the current study revolves around the idea that CVCs are susceptible to being colonized by various microorganisms. Consequently, this leads to a situation where different blood infections transpire, the costs of health care increase, and the occurrence of morbidities grows. In perspective, the scope of this study is to evaluate the existing evidence concerning the benefits of using antiseptic treatments when dealing with CVCs and apply it in practice. The key objective of the reviewed study was in the application of antiseptics on the patients’ skin and observing the ultimate occurrence of blood infections by reason of the use of CVCs (Bion et al., 2012). The researchers also consulted a number of other research projects in the area and identified several articles (randomized control trials) that dwelled on the use of antiseptic treatment and its overall efficiency. The data concerning the use of almost 3500 CVCs was analyzed (Lai et al., 2016). The significance of the problem can be explained by the fact that some patients were assigned more than one CVC and subsequently, this number did not correlate with the total number of patients. Lai et al.’s (2016) study was supported by both the government and a number of pharmaceutical companies.
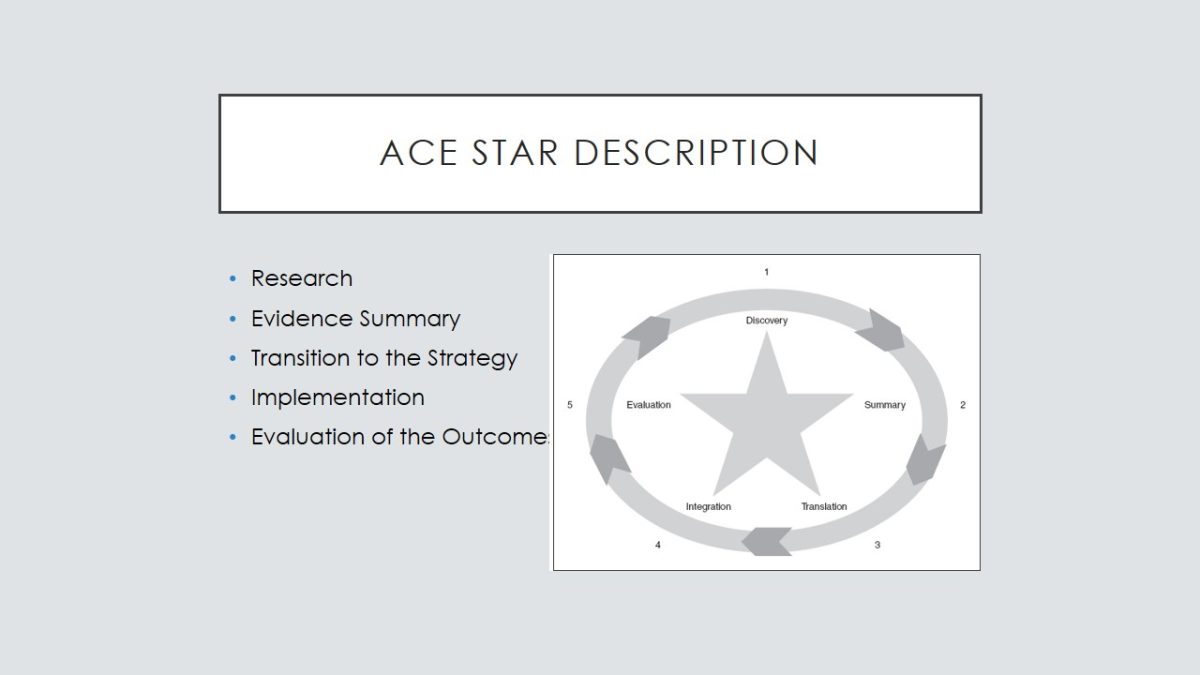
Ace star description
- Research.
- Evidence Summary.
- Transition to the Strategy.
- Implementation.
- Evaluation of the Outcomes.
The ACE Star Model is usually applied to comprehend the stages and key characteristics of knowledge acquiring and transmittance within the framework of evidence-based practice. The core strength of this model consists in the fact that it allows combining old-fashioned concepts and innovative knowledge with the intention of improving the quality of health care. By means of this model, the health care providers are able to develop a framework that will be at the helm of organizing the methods and procedures of the evidence-based practice. The Star Model is a graphic representation of the phases of knowledge renovation and application of the transformed knowledge in practice. By means of this particular model, the nurses are able to make the best use of the exclusive features of evidence-based practice. Therefore, the existing knowledge is also reviewed within the context of evidence-based practice and serves as the basis of the overall evidence-based practice network. A sequential representation of knowledge significantly impacts the process of implementing it in real-life situations. The five stages of the knowledge transformation are as follows:
- Research.
- Evidence Summary.
- Transition to the Strategy.
- Implementation.
- Evaluation of the Outcomes.
The Star Model is used to outline the evidence-based processes, and the ultimate outcome of the transformation is the improvement of the quality of health care.
Scope of the problem
- The use of antiseptics when dealing with central venous catheters and the subsequent prevention of blood infections.
- It is recurrently associated with increased health care costs, causal morbidity, and subsequent death (Parienti et al., 2012).
The practice issue of the current evidence-based project is the use of antiseptics when dealing with central venous catheters and the subsequent prevention of blood infections. This is a rather important problem because these infections are recurrently associated with increased health care costs, causal morbidity, and subsequent death (Parienti et al., 2012). The outcomes of blood infection are commonly mistreated or underestimated by the researchers. The existing statistic suggests that the current percentage of blood infections is 0,07% (meaning that 7 out of 1000 patients died because of a blood infection that was transferred by means of the CVC. On a broader scale, this issue is relevant because the existing body of knowledge presents insufficient evidence regarding the use of antiseptics in addition to the CVC (Bion et al., 2012).
Practice issues
- Occurrence of morbidities.
- Healthcare costs.
- Colonization of catheters by microorganisms.
- Blood infections leading to death.
The CVC (also known as central venous catheter) is used in numerous cases when it comes to monitoring certain health indicators or controlling the intake of medication, nutrition or blood products. The practice issue consists in the fact that catheter is susceptible to being colonized by microorganisms. In perspective, this leads to blood infections and increases the occurrence of morbidities and the costs of health care.
Team and stakeholders
- Nurse manager.
- Two nurse practitioners.
- Pharmacist.
The key team members that will be included in the team are as follows:
- Nurse manager.
- Two nurse practitioners.
- Pharmacist.
The decision to pick these four health care practitioners is based on the supposition that the researcher will have to gain insight into each of the stages of the project.

Roles and responsibilities
- Nurses – to implement the EBP and apply necessary antiseptic treatments (Parienti et al., 2012).
- Pharmacist – to provide the nurses with necessary medications.
- Nurse manager – to guide the team.
The role of the nurse practitioners can be described as the implementation of the developed evidence-based practice plan. They will have to follow the guidelines and apply necessary antiseptic treatments on the skin of the patients with CVCs in the area where the catheter enters the body (Parienti et al., 2012). Consequently, the pharmacist will be responsible for providing the nurses with the necessary medications and consult them regarding the application of the antiseptic treatment. The nurse manager will ultimately guide the team and give out internal team directions intended to help them handle the assignment.
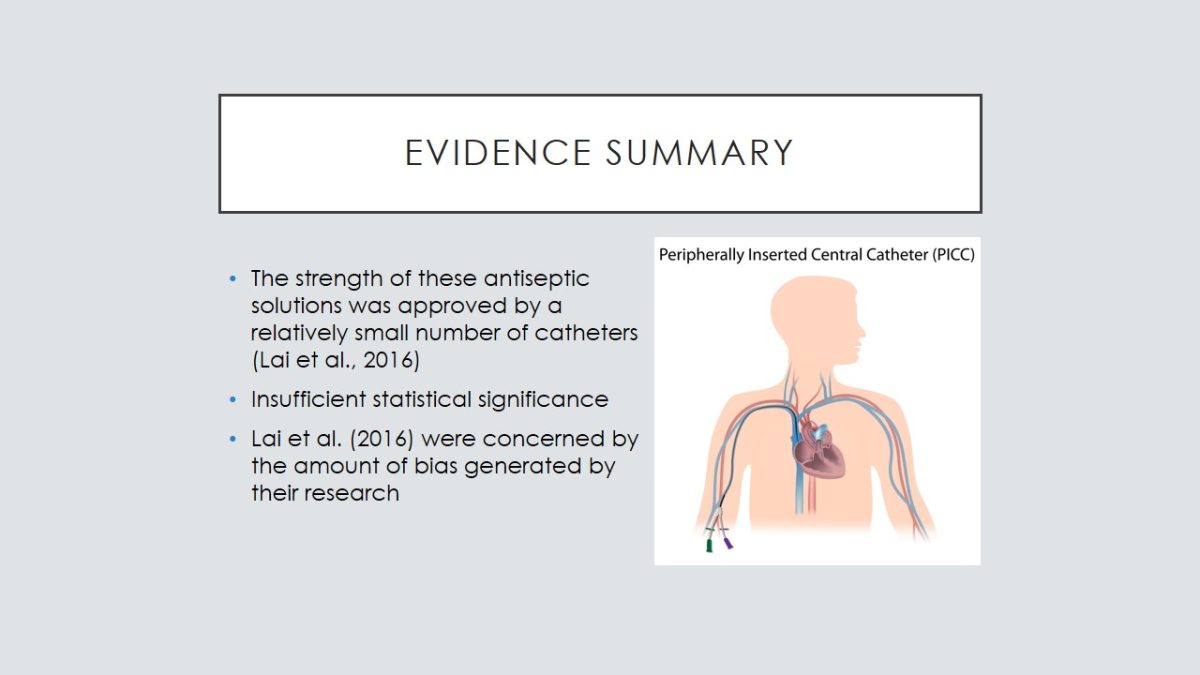
Evidence summary
- The strength of these antiseptic solutions was approved by a relatively small number of catheters (Lai et al., 2016).
- Insufficient statistical significance.
- Lai et al. (2016) were concerned by the amount of bias generated by their research.
In addition to the existing evidence, the researcher identified certain data regarding the risks of CVCs in comparison to peripherally introduced catheters and analyzed the method of subclavian insertion in terms of the risk of blood infection. No particular evidence-based or clinical practice guidelines were identified. The strength of the research projects can be explained by the low level of partiality of the obtained data.
If we take into consideration the strength of the evidence, we may see that the comparison between povidone-iodine and chlorhexidine solution provides us with the most robust results. Nonetheless, one should remember that the strength of these antiseptic solutions was approved by a relatively small number of catheters (Lai et al., 2016). Additionally, each of the comparisons was supported by a limited number of trials. This means that even though the findings of the study are significant, they cannot be interpreted in a confident manner. Another finding of the study consisted in the fact that the amount of obtained data was insufficient to reach a verdict regarding the statistical significance of the results of the conducted research. It was also identified by the authors of the research that the small number of trials adversely impacts the validity of the research results (this can also be connected to a limited number of catheters). Therefore, Lai et al. (2016) were concerned by the amount of bias generated by their research and could not make a univocal conclusion regarding the effect of small studies that were analyzed within the framework of the presented research.
Recommendations for change
- Use chlorhexidine solutions when performing antiseptic treatment.
- Use the subclavian site as the primary place of catheter insertion (Chopra, O’Horo, Rogers, Maki, & Safdar, 2013).
- Use cleansing approach to the treatment (Patel et al., 2013).
- Not sure if antiseptic skin cleansing influenced the occurrence of mortality and morbidities (Raad et al., 2016).
There are several recommendations that can be formed on the basis of the obtained evidence. First, the author proposes to use chlorhexidine solutions when performing antiseptic treatment of CVCs during the pilot program. Second, the author intends to use the subclavian site as the primary place of catheter insertion (Chopra, O’Horo, Rogers, Maki, & Safdar, 2013). Third, it is important to evade idle catheter days so as to certify timely replacement of catheters and minimize the chance of triggering blood infections or catheter colonization. The interventions were analyzed by the authors of the article on the basis of the existing evidence. First, the researcher did not find any significant differences between cleansing/ no cleansing approach to the treatment (Patel et al., 2013). Therefore, there were no particular recommendations regarding the use of catheters or antibiotics and the prevalence of blood infections. Second, the authors analyzed the use of chlorhexidine and did not find any critical variances in the infection rates among the patients with CVC (Chopra et al., 2013). Nonetheless, this treatment is recommended because it helps to reduce the occurrence of blood infections and the ultimate process of colonization (Lai et al., 2016). Moreover, the occurrence of bloodstream infections is also mitigated. The authors of the article did not provide any recommendations regarding the use of chlorhexidine but claimed that the difference between these two treatments is almost impalpable and it cannot be explicitly stated if antiseptic skin cleansing influenced the occurrence of mortality and morbidities (Raad et al., 2016).
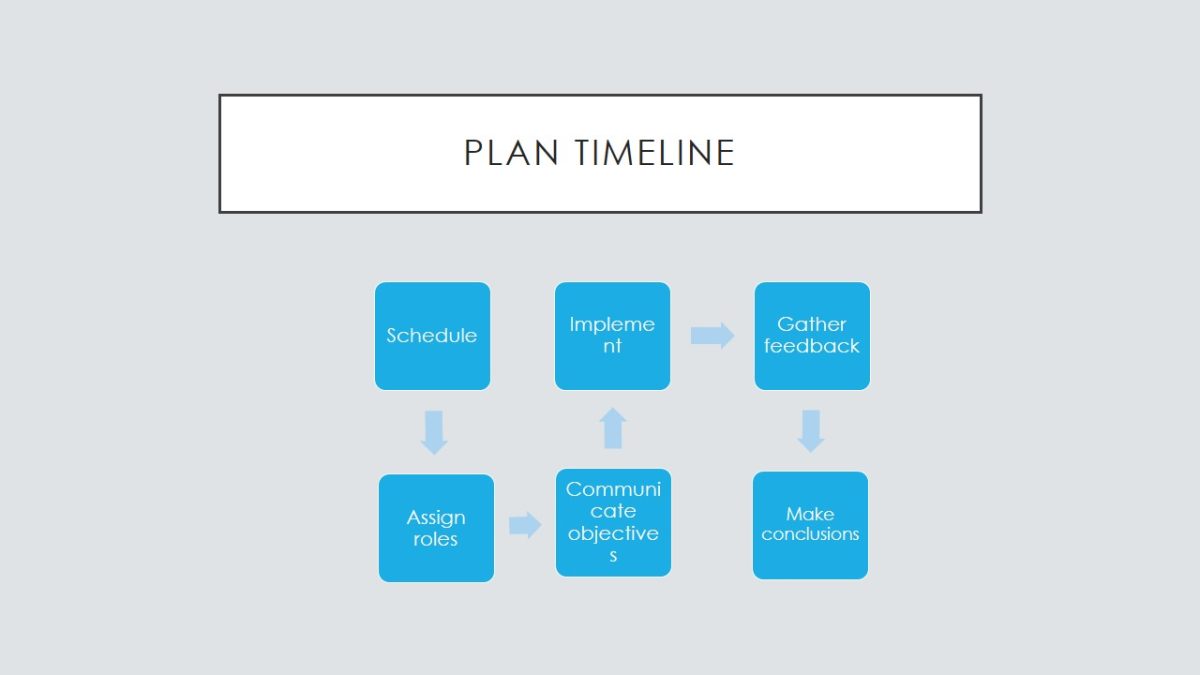
Action plan
- Develop a schedule.
- Assign roles and responsibilities.
- Communicate the objectives.
- Implement the plan.
- Gather feedback.
The first step will be to develop a specific schedule so as to define working hours for each of the members of the team. The second step will be to assign roles and tasks because it is necessary to plan this activity efficiently. The third step will be to communicate the objectives of the project to the team and the patients that will be involved in the project. The fourth step will be to implement the plan and follow the preset guidelines. The last step will be to gather feedback from all the participants of the experiment, analyze the obtained data, and make conclusions regarding the usefulness of nurse rotation and antiseptic treatment. The results will be reported in the form of a survey (a mixed questionnaire with both open and multiple-choice questions).
Plan timeline
- Schedule.
- Assign roles.
- Communicate objectives.
- Implement.
- Gather feedback.
- Make conclusions.
The timeline for this plan is 60 days.
Process, outcomes, and reporting
- Define the effectiveness of antiseptics.
- Qualitative measurements.
- Internal meeting reports.
The researcher expects to define perfect nurse rotation times and assess the effectiveness of antiseptic treatments with CVCs. These outcomes will be measured qualitatively so as to support the evidence-based approach to this study. Moreover, the researcher is going to specify the number of variables that will serve as indicators of the success of the implementation of the program. The results will be reported on internal meetings so as to support the principle of confidentiality and not to disclose any of the important findings or claims before the end of the project.
Next steps
- Evaluate more literature.
- Align the project with the proposed model of knowledge transformation.
- Integrate the changes into practice (Raad et al., 2016).
In order to implement the proposed plan on a larger scale, the researcher will need to evaluate more relevant literature on the subject so as to synthesize a more significant body of knowledge and adjust the project accordingly so that it would comply with the concepts of the knowledge transformation model discussed above. The application of this project to the facility as a whole is questionable due to the local character of the research project. So as to make the changes permanent, the researcher expects to conduct meetings and discuss the key aspects of the innovative plan in order to integrate it into the practice of the designated hospital department (Raad et al., 2016).

Disseminating the findings
- Weekly gatherings.
- Communication of the findings.
- External meetings and electronic distribution.
The findings of the study will be communicated by means of weekly gatherings. These gatherings will include the team responsible for the implementation of the project and other health care specialists that are interested in the outcomes of the research. The investigator expects to communicate the findings in the electronic format as well so as to reach out to the external stakeholders and other health care organizations. Several external meetings and briefings are also possible if the researcher expects to implement the findings of the current project on a bigger scale.
Forms
- Filling a survey.
- Different questionnaires for team members and patients.
- Reasonableness of the program and overall level of health care.
So as to evaluate the outcomes of the study, the researcher will ask the participants of the study and the members of the team to fill in a survey. This form will feature a number of questions that will be used to evaluate the ultimate eminence of the program and its alignment with the original goals. The patients will receive slightly different questionnaires so as to provide their opinion regarding the reasonableness of the implemented program, courteousness and professionalism of the members of the research team, and their overall contentment with the level of health care at the local facility.
Resources available
- Human Resources.
- Time.
- Briefing rooms for discussion.
- Necessary literature on the topic.
The list of the available resources includes a number of critical entries. First of all, it is human resources. At this point, the researcher takes into consideration the members of the team and the patients that will partake in the experiment. Second, the research team possesses the necessary time resource to conduct this research project. Also, the team has several facilities that may be used as briefing rooms and discuss the interim findings of the study. The researchers have access to literature sources both online and offline and can consult them at any given period of time.
Summary
- Use of catheters is less dangerous when antiseptics are applied (chlorhexidine).
- It is necessary to evade idle catheter days.
- It is possible to introduce the CVC into the subclavian site to reduce the load on the catheter.
The current paper dwelled on the basic stages and implications of a plan intended to mitigate the adverse outcomes of using central venous catheters (CVCs) without applying antiseptic treatments. The problem, in this case, consists in the fact that blood infections triggered by the colonization of catheters may lead to serious health damage or even death. The results of the research showed that it is important to use antiseptics when dealing with preventing blood infections (chlorhexidine solutions in particular). Also, the author was able to find that CVCs may be applied to the subclavian site in order to reduce the load on catheters. The concluding finding helped the researcher to suggest that evading idle catheter days will be beneficial and no catheter colonization will take place.
Extensive research on the use of central venous catheters and antiseptic treatments was conducted within the framework of the current study. The author analyzed the information presented by other investigators and put it together so as to get an evidence summary. Then, the researcher discussed the proposed strategy and its probable implications for the evidence-based practice and the given healthcare facility. The next step on the way to conducting an effective project was the implementation of the proposed plan that suggested that nurses should use antiseptic treatments and rotate after a specified period of time. The evaluation of the outcomes showed that the project is reasonable and can be applied in bigger-scale environments.
References
Bion, J., Richardson, A., Hibbert, P., Beer, J., Abrusci, T., Mccutcheon, M., . . . Harrison, D. (2012). ‘Matching Michigan’: A 2-year stepped interventional programme to minimise central venous catheter-blood stream infections in intensive care units in England. BMJ Quality & Safety, 22(2), 110-123. Web.
Chopra, V., O’Horo, J. C., Rogers, M. A., Maki, D. G., & Safdar, N. (2013). The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: A systematic review and meta-analysis. Infection Control & Hospital Epidemiology, 34(09), 908-918. Web.
Lai, N. A., Lai, N. M., O’Riordan, E., Chaiyakunapruk, N., Taylor, J. E., & Tan, K. (2012). Skin antisepsis during catheter insertion for reducing central venous catheter related infections. Cochrane Database of Systematic Reviews, 7(10), 1-14. Web.
Parienti, J., Cheyron, D. D., Timsit, J., Traoré, O., Kalfon, P., Mimoz, O., & Mermel, L. A. (2012). Meta-analysis of subclavian insertion and nontunneled central venous catheter-associated infection risk reduction in critically ill adults. Critical Care Medicine, 40(5), 1627-1634. Web.
Patel, G. S., Jain, K., Kumar, R., Strickland, A. H., Pellegrini, L., Slavotinek, J., . . . Karapetis, C. S. (2013). Comparison of peripherally inserted central venous catheters (PICC) versus subcutaneously implanted port-chamber catheters by complication and cost for patients receiving chemotherapy for non-haematological malignancies. Supportive Care in Cancer, 22(1), 121-128. Web.
Raad, I., Chaftari, A., Zakhour, R., Jordan, M., Hamal, Z. A., Jiang, Y., . . . Hachem, R. (2016). Successful salvage of central venous catheters in patients with catheter-related or central line-associated bloodstream infections by using a catheter lock solution consisting of minocycline, EDTA, and 25% ethanol. Antimicrobial Agents and Chemotherapy, 60(6), 3426-3432. Web.