Introduction of a Change Management Theory
- Lewin’s change model (1951);
- Lewin: the pioneer of change theories;
- Phase 1: unfreezing;
- Phase 2: transitioning;
- Phase 3: refreezing.
For the current project, a change model introduced by Kurt Lewin will be used. The theory involves three steps: unfreezing, moving or transitioning, and refreezing (Mitchell, 2013; Shirey, 2013). At the first stage, the preparation for change is performed. Particularly, the team leader recognizes a problem, delineates the need for change, and encourages others to notice the need for change (Shirey, 2013). At the second stage, it is crucial to view change not as an event but as a process. At this phase, a detailed plan of actions is created. The difficulties at this stage are associated with fear and doubt (Shirey, 2013). The third phase presupposes the stabilization of change (Cummings & Worley, 2015). The change becomes integrated into the existing system.
Lewin’s Change Model: Strength and Weaknesses
- Strengths:
- versatility;
- practicality;
- simplicity of use;
- easiness of understanding;
- Limitations:
- overly simplified;
- static perspective;
- linear.
Lewin’s theory has several crucial advantages. First of all, it is versatile and practical. Secondly, the theory is simple, and it can be employed even by beginning leaders. Also, since the model is old, there is much experience that can be borrowed (Shirey, 2013). Finally, the theory is easy to understand and implement.
Although Lewin’s change model is rather popular, there is some criticism concerning it. The major disadvantage is that it may be overly simplistic and cannot be regarded as a scholarly approach. Secondly, the static perspective of the model hinders analyzing a variety of complex modern issues (Shirey, 2013). Thirdly, the present-day healthcare system is non-linear, which makes it impossible to apply the theory to some issues.
Step 1: Unfreezing
- Recognizing the problem.
- Outlining the need for change.
- Mobilizing others.
At the first stage, I will recognize the problem and mobilize others to notice the need for change. In order to do so, I will inform the community about the seriousness of the issue of homelessness among adolescents and young adults. In particular, I will prepare a report in which significant statistical data will be included. Over 1.6 million of young adults and adolescents in the US are reported to be homeless annually (Haskett, Armstrong, & Tisdale, 2016). Then, I will explain the need to change these drastic numbers. It is the duty of public health professionals, as well as other community members, to eliminate the incidence of young people’s homelessness. Next, I will invite a team of specialists and stakeholders to support the initiative and create a plan of actions.

Step 2: Transitioning
- Creating the plan of actions.
- Eliminating doubts and fears.
- Involving as many stakeholders as possible.
The second step in Lewin’s change model is moving or transitioning. At this point, it is necessary for a leader to prepare a detailed plan of actions based on the needs of the suggested program. My plan will consist of the following steps: preparing a detailed report on the issues, gathering a team of professionals each of whom will contribute to the development of the project, and inviting stakeholders from the community to support the program. Since a common problem at this stage is feeling uncertain and doubtful about the positive development of the project, I will eliminate fear and doubts by offering examples from similar projects that proved to be successful. A study by Rahman et al. (2014) may be employed to analyze the effectiveness of interventions aimed at reaching homeless youths. Research by Rahman, Turner, and Elbedour (2015) may be used to demonstrate positive outcomes of educating the homeless.
Step 3: Refreezing
- Stabilizing the change.
- Embedding the program into policies.
- Incorporating the aspects of the intervention in the existing practices.
At the final stage of Lewin’s change model, it is necessary to make sure that the change has been accepted at various levels of the community life and policy regulations. Thus, it will be necessary to prepare a final report delineating the achievements gained with the help of the program. In particular, I will analyze the outcomes and compare them with the findings of previous studies. Also, I will investigate the statistics to evaluate how the situation with homelessness among young adults and adolescents in the community has altered. Finally, I will suggest changes to policies and regulations that will help to improve the situation in the future.
Team’s Roles and Responsibilities for Step 1
- Public health leader: preparing the report, gathering and analyzing data.
- Team members: predicting complications and suggesting the best solutions.
- Accountant: assessing the required resources.
- Public health leader: inviting stakeholders and encouraging them to participate in the program.
During the unfreezing stage, each team member will have a range of duties to fulfill. The public health leader will synthesize the information on the problem and suggest a set of solutions to be included in the project. Also, the leader will appoint responsibilities to team members. The social worker will explain the issues concerned with building cooperation between our agency and the homeless youth. The career counselor will analyze the most suitable professions to be suggested to the vulnerable population. The psychologist will investigate and present the difficulties in work with such individuals and will suggest the ways of managing these issues.
Team’s Roles and Responsibilities for Step 2
- Public health leader: creating the plan of actions.
- Team members: expressing their suggestions and performing their responsibilities.
- Stakeholders: providing support in implementing the project.
At this stage, the actual implementation of change will be performed. The public health leader will present a detailed plan of actions and will invite team members to make any relevant corrections to it. The social worker will communicate with homeless adolescents and young adults to persuade them to participate in the program. The psychologist will analyze the needs of the vulnerable population and will consult the homeless youth on the issues that bother them. The specialist in career counseling will help the youths to decide what education they would like to obtain and what occupation they would like to have. By assembling the efforts of all these specialists, as well as other team members, we are planning to reach the needed change. The change will be impossible without stakeholders such as school and college directors, shelter managers, therapists, and charity organization managers. All of these people will help to implement and support the project.
Team’s Roles and Responsibilities for Step 3
- Team members: reporting on the progress.
- Stakeholders: reporting on outcomes and outlining limitations.
- Public health leader: preparing a comprehensive description of the program results.
At the last stage of change model, it will be necessary to stabilize the change by embedding it into the existing policies. The principal responsibility at this phase will be taken by the public health leader. I will need to provide the justification for the program’s success so that the community would make this change permanent. To do so, I will prepare a statistical comparison of data and write a report on the achievements. Team leaders will help me in this process. Stakeholders will perform the analysis of benefits and limitations of the intervention.
Outcome Measures
- The elimination of the number of homeless adolescents and young adults.
- The improvement of healthcare among the vulnerable population.
- The development of positive thinking among the homeless youth.
To evaluate the success of the program, I will assess several factors. First of all, I will check whether the rate of homelessness among young people has decreased. The desired outcome is a decrease by at least 15%. Secondly, I will evaluate the healthcare condition of the young people enrolled in the program. The expected result is the improvement by at least 20%. Thirdly, I will assess the attitude of homeless youths who have participated in the project. The desired outcome is the improvement of positive thinking and the desire to obtain education and occupation in the majority of the respondents.
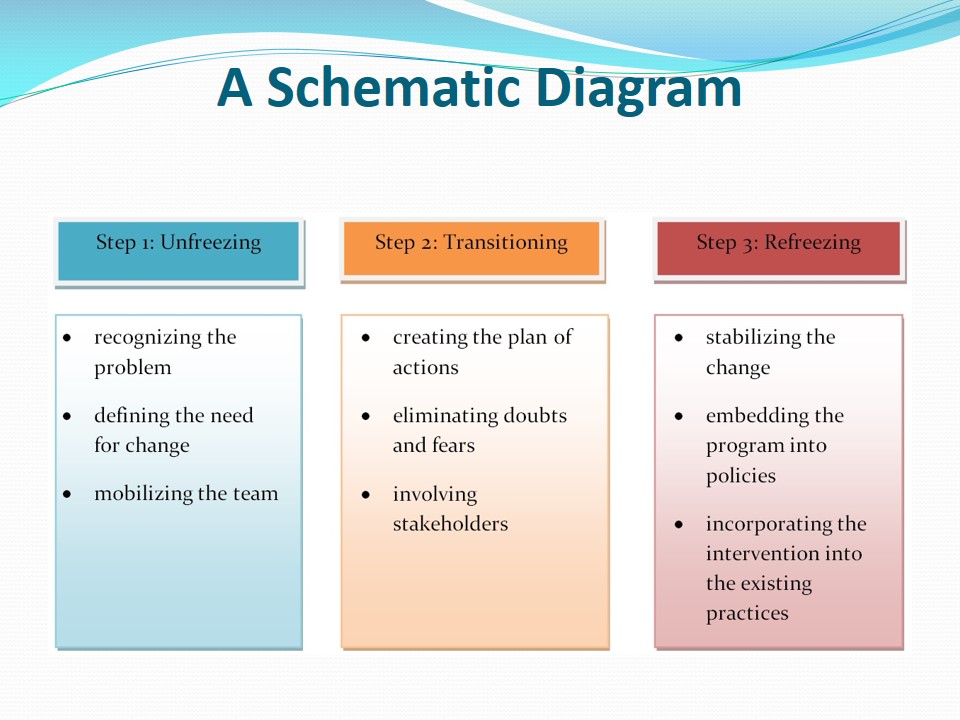
A Schematic Diagram
The diagram presents the steps of the change effort that our team has addressed.
References
Bonevski, B., Randell, M., Paul, C., Chapman, K., Twyman, L., Bryant, J., … Hughes, C. (2014). Reaching the hard-to-reach: A systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Medical Research Methodology, 14(42), 1-29.
Cummings, T. G., & Worley, C. G. (2015). Organization development and change (10th ed.). Stamford, CT: Cengage Learning.
Haskett, M. E., Armstrong, J. M., & Tisdale, J. (2016). Developmental status and social–emotional functioning of young children experiencing homelessness. Early Childhood Education Journal, 44(2), 119-125.
Mitchell, G. (2013). Selecting the best theory to implement planned change. Nursing Management, 20(1), 32-37.
Rahman, M. A., Turner, J. F., & Elbedour, S. (2015). The U.S. homeless student population: Homeless youth education, review of research classifications and typologies, and the U.S. federal legislative response. Child & Youth Care forum, 44(5), 687-709.
Shirey, M. R. (2013). Lewin’s theory of planned change as a strategic resource. JAMA, 43(2), 69-72.