Overview
This fact sheet aims at providing scientific evidence on the relationship between obesity, chronic inflammation and CVD.
Obesity
The occurrence of obesity in industrialized countries is very high. In addition, it is deemed to result in high CVD morbidity and mortality rates. The increase in obesity is an indicator for evolving lifestyles supported by the availability of highly processed foods that are energy-dense. Meta-analytical reports have indicated that the relative risk of CVD as a result of metabolic syndrome is 1.5 to 2. Inflammation is evident among persons with metabolic syndrome that is mainly a result of abdominal obesity (6). Metabolic syndrome is perceived as a group of metabolic disorders with insulin resistance as a central marker. Insulin resistance is associated with typical dyslipidemia (6). Other metabolic disorders, which together define metabolic syndrome include:
- High blood pressure
- Dysglycemia leading to glucose intolerance
- Type 2 diabetes
- Inflammation
The association between obesity and CVD is attributed to chronic inflammation. Most of the literature on obesity, inflammation and CVD targets adults. This is because CVD stems from chronic inflammation and will therefore manifest in later years (1). Initially, adipose tissue was not deemed as having inflammatory potential until evidence of elevated secretion of inflammatory factors from adipose tissue of obese individuals was obtained. Literature has increasingly aimed at demonstrating that there is a direct relationship between an increase in adipose tissue mass and systemic inflammation.
CVD and Systemic Inflammation
Systemic metabolism is affected by molecular and cellular changes that result from enlarged adipocytes in obese individuals. This is illustrated in figure 1 below (6). However, other intermediate risk factors such as “dyslipidemia, hypertension and diabetes” are involved (5).
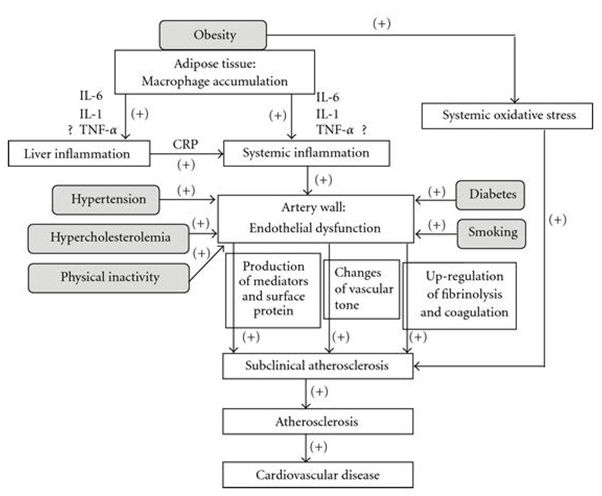
Enhanced courses are shown by the plus symbols alongside the arrows.
Local inflammation results from accruing macrophages in adipose tissue. In obese individuals, the proinflammatory proteins: IL-6 and TNF-α, are more detectable compared to lean individuals (1, 2). In addition, there is an increase in the numbers of macrophages in obese persons and these scavenge apoptotic adipocytes. The increase and accumulation of macrophages and local inflammation are believed to be the reason for several metabolic dysfunctions associated with obesity like systemic inflammation and atherosclerosis (2).
Recent evidence indicates that adipocytes also exhibit detectable properties of intrinsic inflammation. The adipocyte is as sensitive to cytokine-mediated inflammatory signals as well as infectious diseases as the macrophages (4). Once its host of receptors is stimulated, the following takes place:
- Activation of multiple inflammatory signal transduction cascades
- Induction and secretion of several acute phase reactants and potent inflammatory cytokines
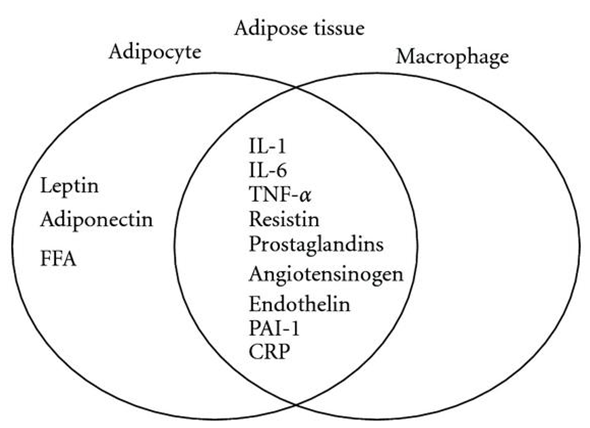
Even though induction and secretion of various inflammatory mediators and acute phase reactants are restricted to paracrine and autocrine effects, the action of adipocytes and macrophages significantly contributes to systemic inflammation. The figure below shows the cytokines produced by the synergistic action of macrophages and adipocytes in the adipose tissue of obese individuals (Wang, Nakayama).
Conclusion and Recommendations
Literature shows that chronic low-grade inflammation is associated with metabolic syndrome, insulin resistance, atherosclerosis, diabetes and obesity by creating a pro-inflammatory environment marked by escalating levels of reactive oxygen and nitrogen.
Research indicates that sex hormones are associated with obesity. However, the association between obesity and female sex hormones is not clear. Research (3) indicates that there is a relationship between obesity and inflammation in the context of weight loss. However, the sustainability of weight loss using various methods requires further investigation.
References
- Weiss TW, Seljeflot I, Hjerkinn EM, Arnesen H. Adipose tissue pro‐inflammatory gene expression is associated with cardiovascular disease. International Journal of Clinical Practice 2011; 65 (9): 939-944.
- Li Z, Wang P, Miao C. Adipokines in inflammation, insulin resistance and cardiovascular disease. Clinical and Experimental Pharmacology and Physiology 2011; 38 (12): 888-896.
- Wang Z, Nakayama T. Adipose tissue, inflammation, and cardiovascular disease. Mediators of Inflammation 2010; 2010: 1-17.
- Berg AH, Scherer PE. Adipose tissue, inflammation, and cardiovascular disease. Circulation Research 2005; 96: 939-949.
- Ahluwalia N, Andreeva VA, Kesse-Guyot E, Hercberg S. Dietary patterns, inflammation and the metabolic syndrome. Diabetes & Metabolism 2012. Web.
- Després JP. Abdominal obesity and cardiovascular disease: is inflammation the missing link? The Canadian Journal of Cardiology 2012; 28(6): 642-652.