Background
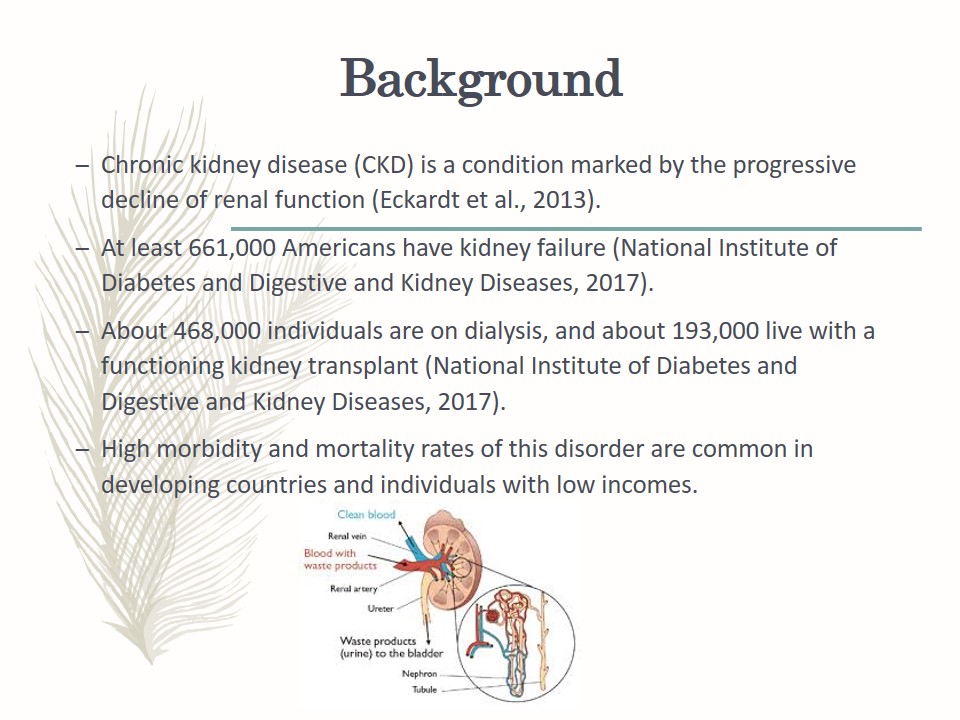
- Chronic kidney disease (CKD) is a condition marked by the progressive decline of renal function (Eckardt et al., 2013).
- At least 661,000 Americans have kidney failure (National Institute of Diabetes and Digestive and Kidney Diseases, 2017).
- About 468,000 individuals are on dialysis, and about 193,000 live with a functioning kidney transplant (National Institute of Diabetes and Digestive and Kidney Diseases, 2017).
- High morbidity and mortality rates of this disorder are common in developing countries and individuals with low incomes.
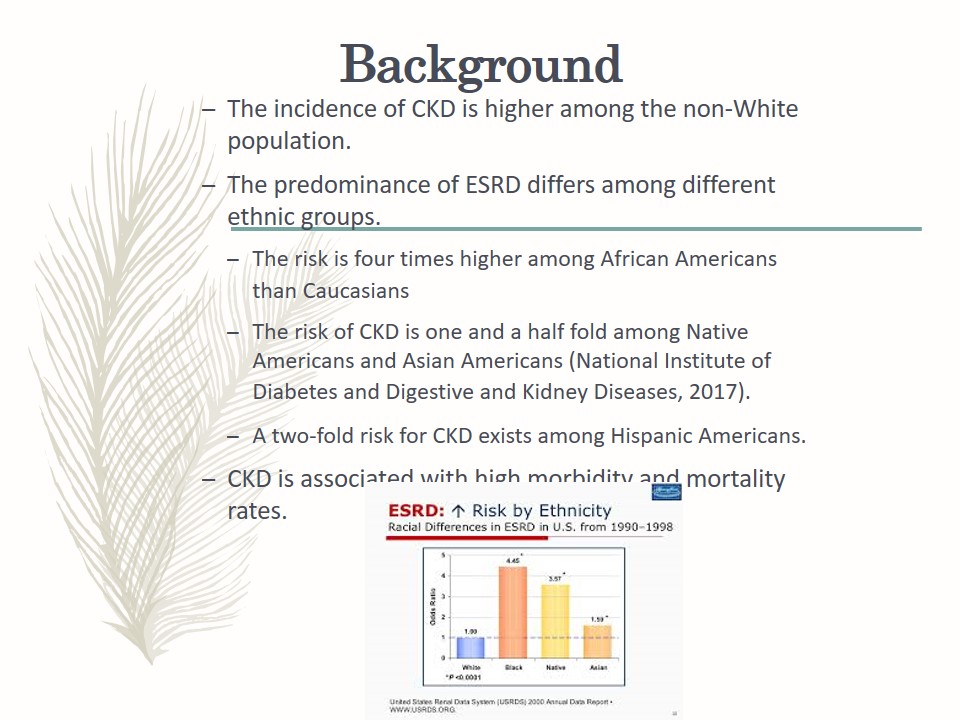
- The incidence of CKD is higher among the non-White population.
- The predominance of ESRD differs among different ethnic groups.
- The risk is four times higher among African Americans than Caucasians;
- The risk of CKD is one and a half fold among Native Americans and Asian Americans (National Institute of Diabetes and Digestive and Kidney Diseases, 2017);
- A two-fold risk for CKD exists among Hispanic Americans.
- CKD is associated with high morbidity and mortality rates.
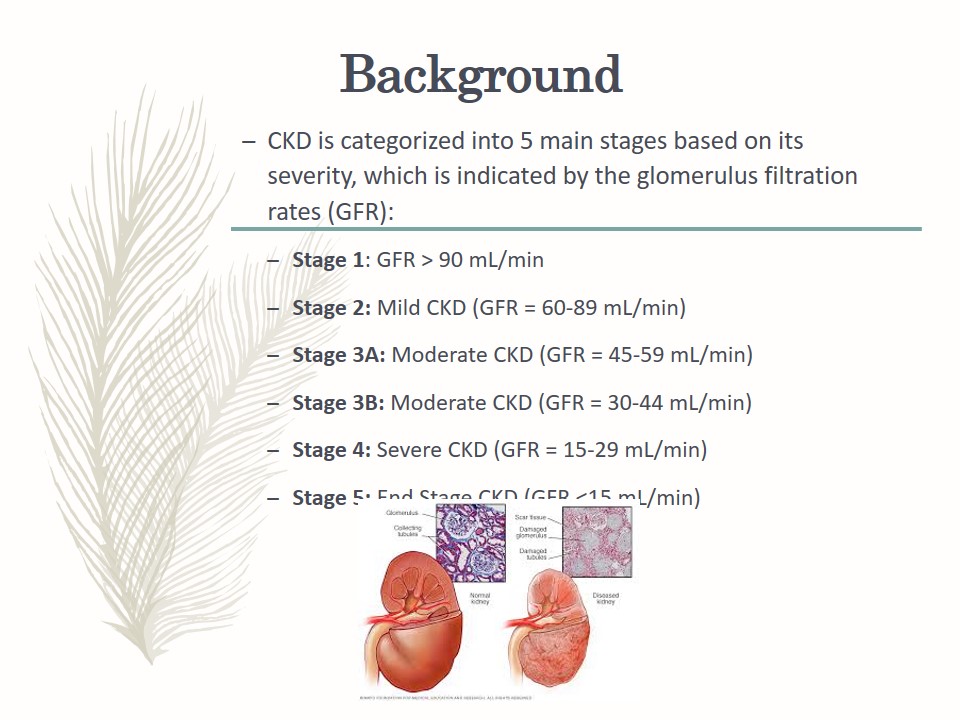
- CKD is categorized into 5 main stages based on its severity, which is indicated by the glomerulus filtration rates (GFR):
- Stage 1: GFR > 90 mL/min;
- Stage 2: Mild CKD (GFR = 60-89 mL/min);
- Stage 3A: Moderate CKD (GFR = 45-59 mL/min);
- Stage 3B: Moderate CKD (GFR = 30-44 mL/min);
- Stage 4: Severe CKD (GFR = 15-29 mL/min);
- Stage 5: End Stage CKD (GFR <15 mL/min).
A healthy kidney has about 1 million nephrons, each of which plays a significant role in the total glomerular filtration rate (GFR).
Any damage to the kidney (regardless of the cause) interfere with the integrity of the nephrons and their capacity to sustain the required GFR.
However, the remaining nephrons strive to maintain the GFR, which overworks them leading to hyperfiltration and compensatory hypertrophy.
In the end, the kidney function declines.
The effects of kidney function decline manifest in the form of an increase in plasma solutes such as creatinine and urea. However, this manifestation normally becomes apparent after the total glomerulus filtration rate has reduced to half the normal value.
The increase in plasma creatinine value is a factor of GFR reduction.
Genetic Contribution to CKD
- Genetics plays an important role in the development of CKD.
- Monogenic disorders, for example, X-linked Alport syndrome and complex polygenic diseases elevate the risk of CKD (Smyth, Duffy, Maxwell, & McKnight, 2014).
- Genetic variation in certain genes is attributed to a decline in renal function over time.
- Changes in the α-adducin and apolipoprotein genes promote renal function deterioration (Smyth et al., 2014).
- Mutations in the epsilon 4 variant of apolipoprotein genes lower the risk of unfavorable renal sequels.
- Genetic disorders such as atypical hemolytic uremic syndrome (HUS), Dent disease, and nephronophthisis increase the risk of CKD.
- Genetic modifications in apolipoprotein L1 (APOL1) genes among blacks are related to ESRD due to elevated blood pressure (Smyth et al., 2013).
- Blacks who lack the risk genotype and European Americans are more predisposed to nondiabetic CKD.
- Changes in the FGF-23 gene, which is associated with circulating levels of the hormone fibroblast growth factor 23 (FGF-23) are linked to a higher incidence of CKD.
- Single-nucleotide polymorphisms (SNPs) are associated with changes in the GFR.
- Polymorphisms in genes involving the renin-angiotensin system (RAS) and the immune system are implicated in susceptibility to CKD (Smyth et al., 2013).
Risk Factors for CKD
- Systemic hypertension.
- Nephrotoxins, for example, nonsteroidal anti-inflammatory drugs (NSAIDs).
- Decreased perfusion due to grave, severe dehydration or shock incidents.
- Proteinuria.
- Elevated cholesterol levels (hyperlipidemia).
- Elevated phosphate levels with calcium phosphate deposition.
- Smoking.
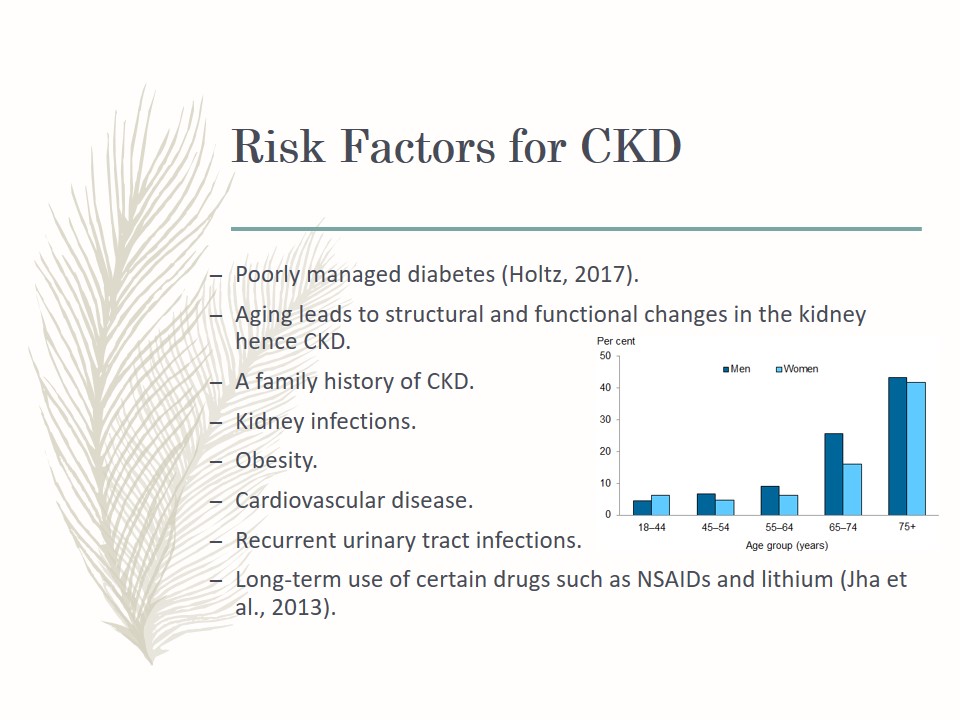
- Poorly managed diabetes (Holtz, 2017).
- Aging leads to structural and functional changes in the kidney hence CKD.
- A family history of CKD.
- Kidney infections.
- Obesity.
- Cardiovascular disease.
- Recurrent urinary tract infections.
- Long-term use of certain drugs such as NSAIDs and lithium (Jha et al., 2013).
Disease Prevention Strategies
- Avoidance of nephrotoxins.
- Consuming a healthy diet.
- Adhering to the physician’s instructions on over-the-counter drugs and avoiding the misuse of pain relievers.
- Maintaining a healthy weight through physical activity and healthy weight loss programs.
- Smoking cessation through support groups, counseling, and medications.
- Managing existing medical conditions such as diabetes mellitus and hypertension with the help of the physician
Disease Implications to the Social and Economic Demographics Globally
- CKD leads to premature morbidity and mortality globally.
- Significant financial resources are spent treating the disease.
- ESRD debilitates individuals and hampers their capacity to work.
- In the United States, new cases of CKD have stabilized at 110,000 annually.
- New cases in Japan stabilized as of 2012.
- Incidence rates have increased for many developing countries.
- There is a huge renal replacement therapy (RRT) gap globally.
New Innovations or Treatments for CKD
- Renal replacement modalities, including peritoneal dialysis, hemodialysis, and transplantation.
- Prompt diagnosis and using prognostic indicators for CKD through the use of biomarkers (Haase-Fielitz, Haase, & Devarajan, 2014). For example, the presence of urinary neutrophil gelatinase-associated lipocalin to indicate renal tubular damage and predict future CKD.
- Kidney repair and regeneration using totipotent cells (Camussi, Bruno, & Bussolati, 2016).
- Drugs meant to forestall dialysis and transplant, for example, Neo-Kidney Augment™ (NKA™) by RegenmedTX (Basu, Bertram, & Ludlow, 2017).
- Development of pharmaceutical agents that will avoid, minimize, or turn round the progression of CKD.
Strengths of Treatment Interventions
- Transplant Surgery:
- Improved quality of life
- Enhanced survival rates than in people who are treated with dialysis
- Eliminates the hours of daily dialysis treatment
- Hemodialysis:
- Allows 4 dialysis-free days in a week.
- Suitable for patients who are unable to conduct dialysis on their own.
- There is room for social interaction among patients undergoing treatment.
- Has a low risk of infection.
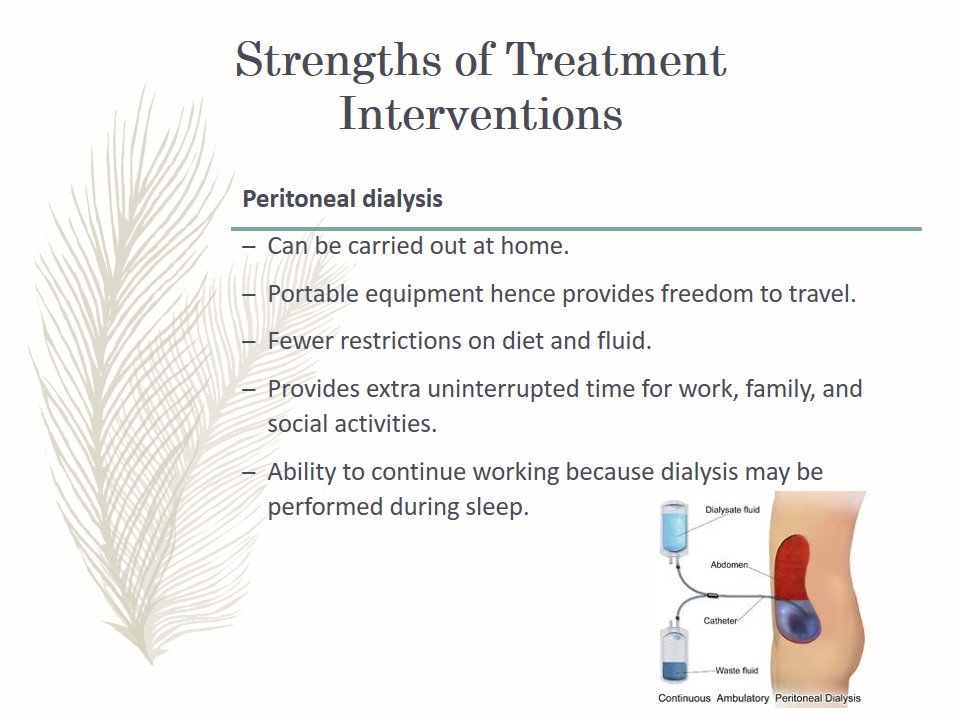
- Peritoneal dialysis:
- Can be carried out at home.
- Portable equipment hence provides freedom to travel.
- Fewer restrictions on diet and fluid.
- Provides extra uninterrupted time for work, family, and social activities.
- Ability to continue working because dialysis may be performed during sleep.
Hemodialysis is a treatment modality that eliminates wastes and extra fluid from the blood.
The dialysis machine requires to access the circulatory system.
Three modes of access exist: fistula, graft, or catheter.
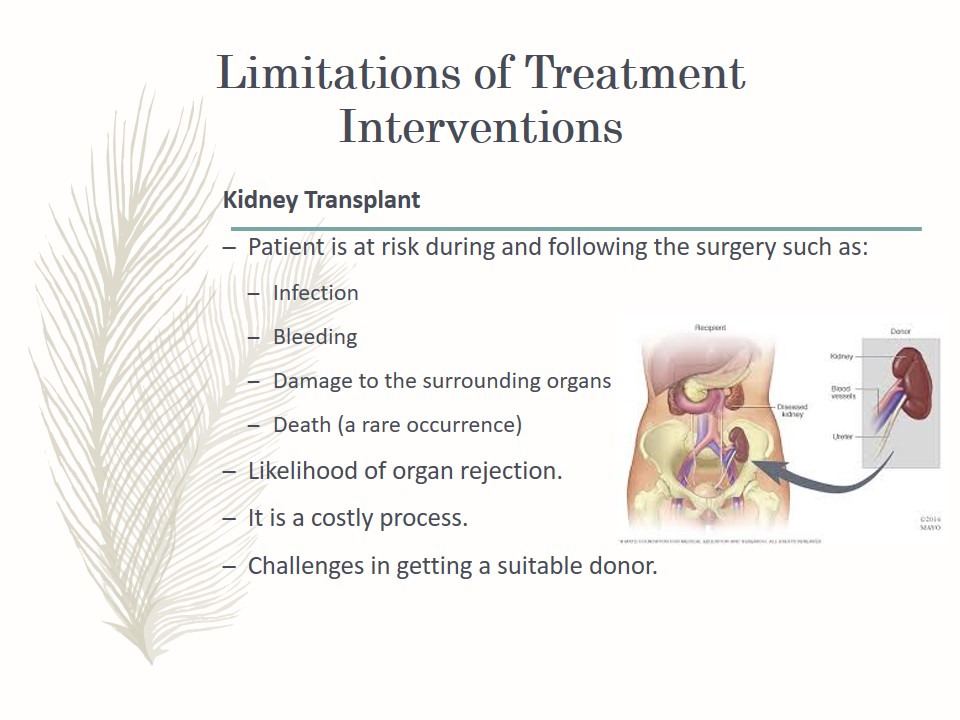
Limitations of Treatment Interventions
- Kidney Transplant:
- Patient is at risk during and following the surgery such as:
- Infection;
- Bleeding;
- Damage to the surrounding organs;
- Death (a rare occurrence);
- Likelihood of organ rejection.
- It is a costly process.
- Challenges in getting a suitable donor.
- The procedure is not suitable for all patients with CKD, e.g.,
- Patients with active or newly treated cancer;
- Low life expectancy;
- Dementia;
- Unmanaged mental disorders;
- Serious obesity (BMI values higher than 40);
- Existing drug or alcohol abuse;
- A history of medication non-adherence.
- Patient is at risk during and following the surgery such as:
- Hemodialysis:
- Each session lasts approximately 4 hours, which interferes with one’s schedule.
- Inconveniences if there is a need to travel.
- Restrictions in diet and fluid intake.
- Low blood pressure is a common complication.
- Lightheadedness.
- Shortness of breath.
- Abdominal cramps.
- Nausea, or vomiting.
- The access can become infected or form blood clots.
- Inability to work due to the time required for travel and treatment.
- Peritoneal Dialysis:
- Requires knowledge of equipment setup.
- An increased risk of hernia from the pressure of the fluid inside the abdominal cavity.
- Excessive weight gain.
- It needs to be carried out every day, which is very disruptive.
- Peritoneal dialysis poses a risk for peritonitis, which is the infection of the thin membrane that lines the abdomen.
- Dialysis fluid may reduce protein levels and cause malnutrition.
- Restrictions on swimming and bathing.
The source of the kidney may be a living donor or a dead person.
A new kidney becomes functional the moment it is transplanted successfully.
However, special drugs are needed to prevent the chances of rejection. In cases of rejection, the patient continues with dialysis, and a second transplant may be performed.
A transplant surgery does not cure CKD. Therefore, recipients need to continue with other disease management strategies such as medications, diet, or dialysis.
A fistula is the preferred access method, which is created through a minor surgical procedure that connects an artery to a vein to form a larger blood vessel.
The benefits of a fistula include fewer complications and longevity of the access.
A graft involves connecting a vein to an artery using a small tube made of synthetic material.
A catheter involves inserting a tube into a large vein the neck and is commonly used when short-term dialysis is required or when it is impossible to create a fistula or graft.
Barriers to Treatment Interventions
- Challenges with renal replacement therapy (RRT) accessibility.
- Challenges with the management of other chronic diseases that culminate in CKD, for instance, cardiovascular disease, diabetes mellitus, and hypertension.
- Financial cost implications of sustaining a dialysis-reliant population.
- Lengthy periods required for the approval of pharmacological agents.
Prognosis
- By Demographics:
- The rate of CKD advancement depends on age and increases as one advances in age.
- Older people have a lower prognosis than younger ones.
- The underlying diagnoses such as hypertension and diabetes mellitus also hasten disease progression and affect the outcomes.
- Socioeconomic Standing:
- Socioeconomically disadvantaged populations have a disparate burden of CKD.
- Suboptimal clinical outcomes are common in this group because of failure to receive evidence-based care.
- The wealthy can afford hemodialysis and peritoneal dialysis and survive longer than those with a lower socioeconomic standing.
- Treatment options such as renal transplant are easily accessible to the affluent population only.
- Geographic Factors:
- Poor access to healthcare facilities, e.g., centers offering dialysis services.
Summary
- CKD is a debilitating disease that lowers the quality of lives of individuals.
- Pre-existing medical conditions such as diabetes mellitus and hypertension increase the risk for CKD and lower the prognosis of the disease.
- Different treatment options are available based on patient needs.
- Cost of treatment is the main barrier observed in the management of CKD.
Recommended Steps
- There is a need for nurses to create awareness about the causes and prevention of CKD.
- Patients suffering from diabetes, hypertension and cardiovascular disease should be counseled to manage their conditions to prevent CKD.
- CKD patients should be guided to delay the progression of the disease.
References
Basu, J., Bertram, T. A., & Ludlow, J. W. (2017). Regenerating kidney structure and function: An industry perspective. In Kidney Transplantation, Bioengineering and Regeneration (pp. 1177- 1187). Cambridge, Massachusetts: Academic Press.
Camussi, G., Bruno, S., & Bussolati, B. (2016). U.S. Patent No. 9,499,796. Washington, DC: U.S. Patent and Trademark Office.
Eckardt, K. U., Coresh, J., Devuyst, O., Johnson, R. J., Köttgen, A., Levey, A. S., & Levin, A. (2013). Evolving importance of kidney disease: From subspecialty to global health burden. The Lancet, 382(9887), 158-169.
Haase-Fielitz, A., Haase, M., & Devarajan, P. (2014). Neutrophil gelatinase-associated lipocalin as a biomarker of acute kidney injury: A critical evaluation of current status. Annals of Clinical Biochemistry, 51(3), 335-351.
Holtz, C. (2017). Global health care (3rd ed.). Burlington, MA: Jones & Bartlett Learning.
Jha, V., Garcia-Garcia, G., Iseki, K., Li, Z., Naicker, S., Plattner, B., … Yang, C. W. (2013). Chronic kidney disease: Global dimension and perspectives. The Lancet, 382(9888), 260-272.
National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Kidney disease statistics for the United States. Web.
Smyth, L. J., Duffy, S., Maxwell, A. P., & McKnight, A. J. (2014). Genetic and epigenetic factors influencing chronic kidney disease. American Journal of Physiology-Renal Physiology, 307(7), 757-776.