Introduction
Cancer treatment and management are one of the main challenges facing the healthcare industry in the UK. According to Fawcett and McQueen (2011), “there are more than 200 types of cancer originating from different causes, presenting with different symptoms and requiring different forms of treatment or management” (p. 2). Change in lifestyle with specific reference to eating habits is one of the risk factors increasing cases of cancer (Fawcett & McQueen 2011). A report released in 2010 by Cancer Research UK (2010) shows that 324, 579 people were diagnosed with various forms of cancer in 2010. The report further asserts that 28% of all deaths in the UK are as a result of cancer. In 2010, 157,250 cancers related to deaths were recorded in the UK. According to MacMillan Cancer Support (2012), there were approximately 1.7 million people living with cancer in the UK. This figure is expected to double by 2030 (MacMillan Cancer Support 2012). The above trend underscores the importance of effective cancer treatment plans.
According to Hubbard (2010), healthcare professionals are required to make complex decisions on cancer treatment and prevention. One of the reasons that explain the complexity of cancer treatment is the high degree of uncertainty. Additionally, the lack of adequate clinical trials to prove the efficacy of a particular cancer treatment increases the complexity of treatment (Hubbard 2010). According to Nutt and Wilson (2010), organizations in different economic sectors are increasingly incorporating the concept of multidisciplinary teams (MDTs) in an effort to deal with complex situations. The healthcare industry in the UK has integrated the concept of MDT in an effort to lower the rate of mortality as a result of cancer. The decision to incorporate the concept of MDT in cancer treatment is informed by the heterogeneous nature of the disease. Consequently, it is imperative for multiple interventions to be undertaken in order to deal with the disease more effectively.
Problem statement
There has been a marked increase in the relevance of MDTs in the operation of firms within the healthcare industry (Blazeby & Wilson 2006). Cancer treatment decisions are mostly made within the context of MDTs. These sentiments are echoed by Nutt and Wilson (2010) who assert that MDTs are “double edged swords” with regard to solving complex problems. Their effectiveness emanates from the fact that they are comprised of different professionals who possess diverse and exceptional skills and knowledge on various healthcare issues. The heterogeneous nature of the team enhances its creativity in solving complex problems as a result of information pooling (Nutt & Wilson 2010). However, decision making in MDTs is faced with a number of challenges. Blazeby and Wilson (2006) assert that little is known about decision making in MDT meetings. To improve the relevance of MDTs within the healthcare sector, it is imperative for healthcare professionals to understand the challenges that hinder the decision-making process.
The heterogeneous nature of MDTs is one of the elements that increase the complexity of the decision-making process. Nutt and Wilson (2010) are of the opinion that the degree of commitment amongst members in heterogeneous teams is relatively low compared to homogenous teams. This may lead to conflict amongst team members hence hindering the effectiveness with which decisions are made (Smidts, Pruyn & Riel 2001). Additionally, the likelihood of MDTs experiencing poor communication and coordination is relatively high (Schmitt 2012). Gopal (2009) asserts that a lack of effective communication is one of the problems experienced by multidisciplinary teams MDTs. This hinders cooperation and information sharing which are paramount in the operation of MDTs.
Despite the aforementioned challenges, research on the factors that hinder decision making in MDTs is not exhaustive. Inadequate team management skills may limit the MDT’s ability to treat and manage cancer. There are a number of aspects that must be taken into account in order for MDTs to be successful. For MDTs to be successful, an effective decision-making process must be integrated. Some of the key requirements include effective communication, good leadership, patient involvement, effective guidelines and standards, and good team dynamics.
Justification
Considering the complexity associated with treating and managing cancer, it is imperative for healthcare professionals to develop effective treatment plans. If this is not done, cancer will continue being one of the leading causes of death in the UK. However, this is only possible through the formulation and implementation of effective decisions. Currently, caring for cancer patients is increasingly becoming a multidisciplinary event. This arises from the fact that there are various types of cancer whose effects and forms of treatment vary. Consequently, it is paramount for decisions on the treatment plan to be made by all the healthcare professionals and support staff. Intervention by diverse healthcare professionals will reduce the rate of mortality as a result of cancer significantly.
Research objectives
This study will be guided by a number of objectives which include;
- To identify the significance of the MDMs in the decision-making process.
- To explore the decision-making process in MDTs.
- To explore factors associated with impeding the decision-making in Cancer MDTs.
Research questions
In line with the above objectives, the following research questions will be considered.
- What is the significance of MDMs in the decision making process in MDTs?
- What are the main factors that hinder decision making in MDTs?
- What are the main elements that should be taken into account in the decision-making process in MDTs?
Contribution to knowledge
The findings of this study will be of great significance to healthcare professionals and other stakeholders in the healthcare industry in their quest to provide optimal care to cancer patients. First, the study will contribute towards a great appreciation of the importance of multidisciplinary teams in solving complex decisions on how to treat cancer. As a result, their contribution to the medical field will be enhanced. Secondly, healthcare professionals will gain insight into the factors that may hinder the effectiveness of MDTs. As a result, they will be able to counter such hindrances hence improving their operational efficiency. By highlighting the significance of multidisciplinary team meetings in making cancer treatment decisions, the study will enable healthcare professionals to appreciate the role of teamwork. As a result, healthcare professionals will appreciate the importance of information sharing in dealing with the complex issues that are associated with cancer treatment.
Literature review
The National Health Service in the UK incorporated the MDT model in 2000 in an effort to ensure that cancer treatment and care is in line with the available evidence. As a result, the status of MDTs in making key decisions on cancer treatment has increased significantly (Patkar & Acosta 2011). MDTs enables healthcare professionals to share information on how to care for cancer patients. This leads to the development of an effective treatment plan hence improving the quality of care provided. According to Patkar and Acosta (2011), effective cancer treatment plans enhance survival amongst cancer patients. Therefore, it is imperative for healthcare professionals to appreciate the role of MDTs in making optimal decisions that will improve cancer treatment and management.
In light of the aforementioned complexity with regard to cancer treatment and management, this section seeks to evaluate the contribution of MDMs in the process of making cancer treatment decisions. The process that multidisciplinary teams follow when making decisions on how to treat cancer and manage cancer is also evaluated. Moreover, the author explores the factors that impede decision making in cancer MDTs.
Multidisciplinary meetings (MDMs)
Considering the complexity associated with cancer treatment and management, it is essential for healthcare professionals to ensure that a high level of coordination and knowledge sharing is attained (Chew 2004). This can be achieved by integrating the concept of multidisciplinary care. Previous studies show that effective multidisciplinary meetings in cancer treatment increase cooperation amongst healthcare professionals. This arises from the interaction that is created amongst healthcare professionals from diverse areas of specialization (Devitt, Phillip &McLachlan 2010). In an effort to develop effective treatment plans, multidisciplinary teams convene meetings regularly. The meetings are aimed at discussing the most effective options for treating and managing cancer (Ministry of Health 2012). Such team meetings are critical in the operation of multidisciplinary teams. Consequently, it is imperative for healthcare professionals to be effective in planning and conducting MDMs.
Significance of MDMs in decision making
Improved treatment planning
Multidisciplinary meetings play a fundamental role in the process of making decisions on how to treat and manage various forms of cancer. Firstly, the meetings enable multidisciplinary team members to identify new issues that should be integrated into the treatment process. Devitt, Phillip, and McLachlan (2010) opine that MDMs enable healthcare professionals to adopt a holistic approach in treating and managing cancer. Moreover, MDMs enable healthcare professionals to discuss various issues regarding the patient and to follow-up on their progress with regard to a particular treatment (Ueno & Cristofanilli 2012). MDMs also create a perfect opportunity for healthcare professionals to share expert opinions on various issues associated with the treatment process. According to Wheless, McKinney, and Zanation (2011), one of the aspects discussed during MDMs relates to newly diagnosed malignancies. This leads to the formulation of preliminary treatment plans on the basis of available evidence. The findings of the discussion are communicated to the patient. As a result, the likelihood of developing an optimal treatment plan in addition to identifying new issues is increased (Sandok 2011). Therefore, one can assert that MDMs provide a perfect peer-reviewing opportunity which improves the effectiveness and efficiency of the decision making process.
Secondly, MDMs are very effective in improving the efficiency with which cancer treatments are conducted. According to Devitt, Phillip, and McLachlan (2010), multidisciplinary meetings are very effective in reducing the amount of time that a patient needs to access treatment. This arises from the fact that effective treatments plan are developed and implemented. MDMs are characterized by a high educational benefit. As a result, healthcare professionals who attend MDMs develop a greater understanding of diverse traditional health disciplines. According to Abdulrahman (2011), multidisciplinary meetings provide valuable teaching opportunities to junior doctors and medical students. Furthermore, MDMs lead to an improvement in the level of interaction amongst healthcare professionals from diverse areas of specialization (Patkar & Acosta 2011). In summary, MDMs contribute to improvement in cancer treatment by creating an environment that stimulates the generation of new knowledge. Moreover, MDMs provide an opportunity for high-quality, efficient, and evidence-based recommendations on how to manage and treat cancer patients to be made.
Improved communication and coordination of services
The success of multidisciplinary teams in the decision making is influenced by the degree of cooperation amongst the members (Monaghan & Sharma 2005). According to Monaghan and Sharma (2005), a high degree of collaboration between health professionals must be ensured in the process of treating and managing cancer (Lee & Ok 2007). To achieve this, an effective communication system amongst team members must be ensured. MDMs lead to improved communication between diverse healthcare professionals (Patkar & Acosta 2011). Patkar and Acosta (2011) further assert that “this reduces delays for patients on the medical admissions unit to a minimum and produces a more appropriate inpatient stay” (p.133). By integrating effective communication amongst team members, the likelihood of the team attaining high effective communication enables team members to share knowledge and skills hence developing a high level of interaction and cooperation.
MDMs play also play a fundamental role in the development of trust amongst the team members. This arises from the fact that the effectiveness with which the treatment plan s developed is dependent on the contribution of all the team members. According to Patkar and Acosta (2011), the absence of trust makes a team be dysfunctional. On the other hand, Lee and Ok (2007) assert that multidisciplinary team meetings enhance the relationship between diverse healthcare professionals due to the inclusion of healthcare professionals from diverse diagnostic disciplines. Thus, one can assert that the working relationship developed amongst healthcare professionals plays an essential role in the development of an effective cancer treatment plan. As a result, the patient’s quality of life, and hence their survival is enhanced.
Evaluation of cancer clinical trials
Multidisciplinary meetings provide team members with an opportunity to discuss diverse clinical trials. Ueno and Cristofanilli (2012) define clinical trials to include the various research studies that are conducted with the objective of discovering new methods and approaches of diagnosing, treating, preventing, and managing cancer. By evaluating available cancer clinical trials, multidisciplinary team members are able to compare new and standard treatment methods. As a result, the team is able to make effective decisions on the treatment approach to deal with various types of cancer. Ueno and Cristofanilli (2012) further assert that clinical trials enable MDTs to be effective with regard to staging and classifying cancer. According to Ueno and Cristofanilli (2012), “cancer classification and staging enable physicians to determine treatment more reliably, to evaluate results of management more accurately and to compare worldwide statistics” (p. 509). Abdulrahman (2011) further asserts that MDTs are more effective and accurate in making treatment decisions compared to individuals. In cases where individual treatment decisions are accurate, MDMs increase the credibility of relying on such decisions. In summary, the evaluation of clinical trials provides doctors with an opportunity to improve and protect the patient.
Improved equality
According to Tanfani and Testi (2012), “all cancer patients should be given an opportunity to access high quality cancer care services” (p.179). For example, all cancer patients living within the vicinity of a healthcare facility that is adequately equipped with a radiotherapy system should be provided with high-quality radiotherapy services. Such treatment increases the likelihood of the patient surviving. Tanfani and Testi (2012) assert that multidisciplinary meetings play a critical role in eliminating inequalities as a result of social class or geographical location. Thus, a multidisciplinary team is able to overcome geographical and social barriers that might limit the level of care given to patients.
Optimal utilization of resources
Multidisciplinary team meetings enable healthcare professionals to optimize the number of resources required to formulate a treatment plan for a particular type of cancer. Findings of a study conducted by Taylor (2010) reveal that a substantial amount of resources are consumed during team meetings. In the UK, there are approximately 1500 multidisciplinary teams whose obligation is to formulate cancer treatment plans. Taylor (2010) further asserts that “this corresponds to over one million person hours of attendance at meetings each year” (p.2). Moreover, some team members may incur additional cost and cost in the process of preparing materials that will enable them to participate in the MDMs. Taylor (2010) estimates the total annual cost for preparing and holding multidisciplinary meetings in cancer treatment to be 50 million pounds. The effectiveness of MDMs in the decision-making process is echoed by a study conducted by Sharma and Associates which is a US-based firm. The study was conducted by 253 colorectal clinical nurse specialists, doctors, and surgeons (Abdulrahman 2011). Ninety-six percent (96%) of the team members were of the opinion that MDMs leads to an overall improvement in the quality of care provided to colorectal cancer patients. On the other hand, 73% of the respondents were of the opinion that MDMs are very cost-effective (Abdulrahman 2011).
Definition of multidisciplinary teams (MDTs)
Healthcare professionals are increasingly appreciating the concept of teamwork in an effort to deal with the complex problems that they face in the course of providing care to patients (Foyle & Hostad 2004). One of the areas where the concept of teamwork is increasingly being integrated relates to cancer care. Bruner (2001) asserts that cancer is a chronic and multisystem disease. This makes its treatment to be very complex. Consequently, it is imperative for a multidisciplinary team approach to be adopted in providing care to patients. Dziegelewski (2013) defines a multidisciplinary team as “a mix of health and social welfare professionals, with each discipline in most part working to an independent basis” (p.117). This means that MDTs are comprised of different healthcare professionals. The duties and responsibilities of each team member are clearly outlined. The findings and opinions of individual members are consolidated in an effort to improve the quality of support and care offered to patients (Mauk 2010).
Decision making in cancer MDTs
Multidisciplinary teams are increasingly being integrated with the process of making decisions on how to treat and manage cancer. This trend is evident in both developed and developing countries. In the UK, the integration of MDTs in the process of making cancer decisions was motivated by the need to provide standardized and optimum care to patients. Additionally, the rationale for the integration of MDTs in the decision-making process emanated from the increment in the degree of complexity on how to treat and take care of cancer patients. As a result, various key professionals are incorporated into the decision-making process.
Some of the key professionals who constitute the multidisciplinary team in cancer treatment include medical oncologists, surgeons, clinical nurse specialists, radiologists, physicians, and pathologists (Mileshkin & Zalcberg 2009). All these parties work in collaboration with one another in the process of making decisions on the most effective plan to treat a particular type of cancer. Before making the treatment decision, multidisciplinary team members engage in intensive discussions on the holistic treatment plan to administer to the patient. The decision is based on a number of factors such as the type of cancer, the patients’ co-morbidities, biological makeup, and social circumstances. The MDT must take into account these elements so as to ensure that the treatment plan developed contributes towards improvement in the patient’s quality of life and hence survival (Mileshkin & Zalcberg 2009).
The decision-making process in MDTs
A comprehensive review of the problem
The first step involves a comprehensive analysis of the problem faced (Jalil 2012). The peer-review phase provides healthcare professionals with an opportunity to understand and focus on the subject under investigation. As a result, deviation from the subject matter is limited. Marchington and Wilikinson (2006) assert that the peer review process aids in establishing checks and balances on the healthcare problem faced thus increasing the effectiveness with which decisions are made.
Additionally, peer reviews play an essential role in nurturing a high degree of cohesion amongst the team members. Jalil (2012) asserts that this arises from the fact that the team members develop a positive perception and value for each other.
The peer-review phase also leads to the development of mutual appreciation amongst the team members. This culminates in a high level of trust between the team members hence enhancing information sharing. Jalil (2012) opines that it is important for the team leader to provide adequate support to team members during the peer review phase. This enhances their commitment to the predetermined goal (Jalil 2012)
Presentation of information gathered
The second step in the decision-making process entails the presentation of information gathered during the multidisciplinary care meetings (Jalil 2012). Some of the information collected relates to the patients’ pathological and radiological information and the patients’ medical history. The information enables healthcare professionals to develop effective treatment plans that suit the patients. The presentation phase also enables healthcare professionals to determine the nature and quality of information gathered. Consequently, information gaps that might affect the decision-making process are identified. Moreover, psychosocial aspects that might have been neglected in the peer review phase such as the patient’s co-morbid conditions are identified. In summary, this step presents a unique opportunity for healthcare professionals to seal information gaps that might exist. As result, the likelihood of developing an effective treatment plan is increased. Moreover, the information gathered ensures that the treatment plan developed is aligned to the patient’s needs. This leads to an improvement in the patients’ level of confidence regarding the treatment plan.
A comprehensive discussion of the treatment plan
In this step, the various allied healthcare professionals and support staff are incorporated into the decision-making process. This aids in gathering diverse viewpoints. To ensure that the opinions of all healthcare professionals are taken into account, it is important for the team members to be provided with adequate time. Additionally, team members’ opinions should be respected. This aids in the creation of an effective collaborative environment between the various team members (Chandrasekar 2011). Moreover, the inclusion of the team members plays a critical role in eliminating fragmentation of the care process due to lack of coordination in the treatment plan. Additionally, the discussion process aids in creating a unity of purpose and clarity with regard to the problem faced.
Factors that impede the decision making in cancer MDTs
Jalil (2012) is of the opinion that “it is becoming a standard practice for cancer patients to be discussed by a multidisciplinary team in order to formulate an expert-derived management plan” (p.389). However, MDTs are not always very effective. Consequently, not all multidisciplinary team decisions are implemented in the process of providing care (Jalil 2012). Some of the factors that hinder decision making in cancer MDTs are evaluated herein.
Lack of adequate clinical information
Information is one of the most important elements in the process of making complex decisions (Shaw 2008). Deb (2006) asserts that healthcare professionals should be provided with sufficient background information about patients. These sentiments are further echoed by Mileshkin and Zalcberg (2009) who assert that adequate clinical information is paramount in the process of making decisions on how to treat and manage cancer. The availability of such information enables healthcare professionals to understand the patients’ needs (Mileshkin & Zalcberg 2009).
Some of the clinical information that must be availed to the multidisciplinary team relate to psychological morbidity. According to Roy-Byrne & Silver (2012), cancer patients experience various forms of psychological complications such as anxiety, loss of self-esteem, and depression. Such types of psychological co-morbidity may interfere with cancer patients’ ability to deal with the symptoms of the disease and the complications associated with the treatment (Roy-Byrne & Silver 2012). Consequently, cancer patients should be screened for psychological distress.
However, making such a diagnosis is very difficult. Roy-Byme and Silver (2012) assert that “psychiatric symptomatology may be mimicked by treatment side effects or symptoms of cancer” (2). Moreover, information about the patients’ social circumstances, preferences, and other concerns must be available to the MDTs. However, patients may be hesitant to reveal psychosocial issues with healthcare.
Lack of investigation results
Biomedical imaging is a critical component in the treatment of cancer. Jalil (2012) proposes that biomedical imaging enables healthcare providers to diagnose cancer symptoms at an early stage. As a result, they are able to reduce the rate of mortality. Biomedical imaging is increasingly playing a fundamental role in various phases of cancer management. Some of these phases include prediction, staging, prognosis, therapy planning and guidance, therapy response, and palliation. Results from the above investigative processes should be presented to the MDTs in order to improve their decision making capability. According to Wheless, McKinney, and Zanation (2011), MDTs have a significant influence on the quality of decisions made. However, MDTs do not always access the necessary information.
Non-attendance of key members
The success of MDTs in making decisions emanates from the contribution of all the team members. Consequently, the core disciplines should be integrated into the decision-making process in order to provide adequate care (Jalil 2012). The composition of MDTs is determined by the type of cancer. According to (Jalil 2012), some cancer patients may require additional expertise or specialist. MDTs are comprised of a core and non-core team members. The MDTs in treating and managing lung cancer varies from that of breast cancer. Some of the core team members involved in making decisions on how to treat lung cancer include; medical oncologist, respiratory medicine specialist, pathologist, and radiation oncologist. On the other hand, the core team members in the treatment of breast cancer include surgeon, pathologist, medical oncologist, pathologist, supportive care specialist, and a radiologist (Jalil 2012).
The absence of one of the core team members may hinder the MDTs’ decision making capability. This arises from the lack of the member’s expert input which may be integral in the decision-making process. According to Rosman, Shah, and Hussain (2013), it is important for the chairman of the MDT to determine whether there is sufficient member representation prior to making decisions on how to treat and manage cancer patients. Jalil (2012) asserts that making decisions in the absence of core and non-core members may lead to ineffective care for cancer patients.
One of the factors that increase the non-attendance of team members is lack of time. According to Smit (2007), adequate protected time is crucial in order for MDT meetings to be held successfully.
Jalil (2012) affirms that team members should have adequate time to enable them to attend and discuss various clinical aspects. This increases their contribution to the decisions on how to treat and manage cancer. On the other hand, lack of time limits the effectiveness with which multidisciplinary teams make decisions. A study conducted by Wheless, McKinney, and Zanation (2011) on the impact of MDT on head and neck cancer treatment shows that MDTs impact the diagnosis, treatment, and cancer staging. Sixty-eight (68%) of the patients considered in the study had their treatment plans changed.
Ineffective group dynamics
Grange (2008) defines group dynamics as “the area of social science that focuses on advancing knowledge about the nature of group life, group development and the interrelations between groups and individuals” (p.15). Team dynamics are an integral element in MDT’s decision-making process. However, the effectiveness with which decisions are made in multidisciplinary teams is affected by a lack of mutual trust and respect, the existence of personal interests, and conflicts amongst team members (Khastar, Kalhorian, Khalouei & Maleki 2011). Moreover, the lack of equality during team discussions affects the quality of decisions made. A report by the Victorian Government (2012) asserts that “nurses in the UK reported feeling marginalised if their contribution of patient-centred information was ignored” (p.9).
Poor team leadership
According to Burkus (2011), poor leadership is one of the major hindrances in MDT’s decision-making processes. MDTs are comprised of members from diverse professional backgrounds. This presents a major challenge in ensuring that team members work harmoniously. Wheless, McKinney, and Zanation (2011) assert that lack of cooperation limits information sharing amongst team members. As a result, the effectiveness and efficiency with which the team makes the decision is adversely affected. To operate efficiently, MDTs must have mature leadership that promotes democracy within the team. This will enhance open and creative discussion amongst team members (Wheless, McKinney & Zanation 2011). To achieve this, multidisciplinary team leaders must possess a number of leadership skills and qualities. First, the leader must encourage inclusiveness. This means that he or she should involve all the team members in the decision-making process (Carmeli, Atwater & Levi (2010). This will result in the development of a sense of belonging amongst the team members hence improving the level of collaboration and the quality of decisions made (Holbeche 2009). Moreover, the team leader must be able to communicate and negotiate effectively so as to enhance interaction within the team (Kawatra & Krishnan 2004).
Lack of patient involvement
Fabbro (2010) is of the opinion that cancer patients should be involved in the MDTs decision making process. Nevertheless, most healthcare professionals do not include patients in the decision making process. According to the European Commission (2012), patient involvement increases the amount of time need to make a decision. This arises from the fact that patients may disagree with the healthcare professional’s opinion. Some healthcare professionals are of opinion that involving the patient may lead to patients bypassing them (European Commission 2012). Moreover, their inclusion may lead to a reduction in the level of trust developed between the doctor and the patient (Victorian Government 2012). Despite these challenges, failure to include patients in the decision-making process may limit MDTs’ ability to make effective decision. For example, the MDT may not understand the patients’ choices and preferences. Moreover, practitioners may not acquire personal information that may be beneficial in the decision-making process (European Commission 2012).
The benefits of involving patients in cancer treatment decisions can be well illustrated by a study conducted in the US. In the study, 269 patients suffering from different forms of urological cancer were considered. The following are the findings of the study.
Type of cancer Percentage of patients diagnosed
- Prostate cancer 34%
- Testicle cancer 5%
- Bladder cancer 23%
- Kidney cancer 35%
Healthcare professionals from different specialties reviewed all the four types of urological cancer through MDTs. Abdulrahman (2011) asserts that as a result of the meeting, diagnosis in 23% of cancer cases reviewed was adjusted while 17% of renal cancer cases reviewed were adjusted. This led to a significant change in the respective treatment plan. For example, the treatment plan adopted for bladder cancer cases was changed with a margin of 44% while that of testicle cases was adjusted with a margin of 29%. Moreover, the treatment plan with regard to renal cancer was also adjusted with a margin of 36% (Abdulrahman 2011). This shows that involving patients in MDTs has a significant impact on cancer treatment and management decisions.
Poor infrastructure
A number of tools and equipment are essential in order for multidisciplinary team meetings to be conducted successfully (Kandula 2007). First, the meeting room should be fitted with effective projection equipment. This provides the multidisciplinary team members with an opportunity to display various results such as medical imaging results. Additionally, the room must be fitted with secure interactive computer systems. Examples of such interactive facilities include videoconferencing and teleconferencing technologies. Such infrastructure increases the rate of attendance by the team members. In the absence of such facilities, the multidisciplinary team decision making capability is adversely affected. Effective infrastructure also increases the effectiveness and efficiency with which MDTs present and share various types of information. According to a study conducted by Jalil (2012), non-attendance, lack of imaging results, and pathology results are cited as the main barriers that hinder MDTs’ decision-making process. The findings of the study are illustrated in the chart below.
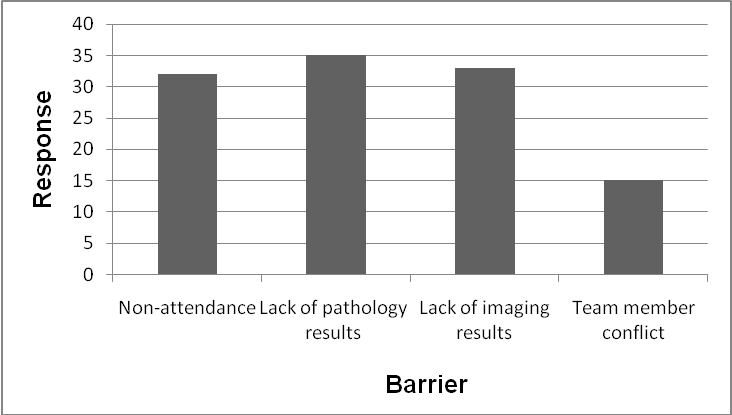
From the chart above, it is imperative for multidisciplinary team leaders to incorporate effective team leadership skills. This will improve the effectiveness with which the teams formulate optimal treatment plans. Considering the information challenges faced by MDTs in making cancer treatment decisions, it is imperative for healthcare professionals to integrate emerging clinical decision support systems. This will enhance the effectiveness with which MDMs are conducted (Patkar & Acosta 2011). The involvement of family members is also cited as another element that healthcare professionals should integrate into the MDTs. According to Hubbard (2010), family members can enable MDTs to access personal information regarding the patient. As a result, the likelihood of MDTs formulating optimal treatment plans is increased. Information sharing is also identified as a critical aspect that should be ensured in MDTs. According to Monaghan and Sharma (2005), the success of MDTs emanates from the cooperation of all the team members. An effective communication mechanism should be integrated in order to enhance information sharing.
Teleconferencing failures
Communication is paramount in the treatment and management of patients. Gurses and Xiao (2006) assert that the communication process is usually challenged by a number of aspects such as fragmentation in the healthcare processes. Gurses and Xiao (2006) are of the opinion that the integration of well-designed information communication tools can improve the reliability, efficiency, and consistency of the communication process. This can be achieved by integrating effective Information Communication Technology (ICT). According to Jalil (2012), ICT is increasingly being adopted by healthcare professionals in an effort to provide optimal care to cancer patients (Jalil 2012). Mileshkin and Zalcberg (2009) further assert that “the use of teleconferencing for multidisciplinary teams is common across the UK, especially in the areas of cancer treatment” (p.171).
According to Latifi (2009), the new technology enhances the effectiveness with which MDTs make decisions with regard to tertiary, secondary, and primary care. This arises from the fact that healthcare professionals are able to share expert knowledge on how to treat and to manage cancer. Moreover, teleconferencing technology increases the effectiveness of communication and collaboration between multidisciplinary team members in different locations (Al-adaileh 2008). Thus, healthcare professionals do not have to be physically present during MDT meetings. However, they can participate in the meeting through videoconferencing and teleconferencing technologies. Davies and Brown (2008) are of the opinion that the professionals’ contribution to the decision-making process may be hindered by technological failure.
Moreover, technological failure may limit the effectiveness and efficiency with which patient information is analyzed. As a result, the amount of time required to make cancer treatment decisions may increase. To eliminate this challenge, it is imperative for multidisciplinary teams to ensure that the information technology adopted is effectively designed in order to meet the teams’ information needs.
Lack of effective administrative and support processes
Burkus (2011) asserts that effective coordination is integral in the operation of MDTs. In order for decision-making to be effective in MDTs, a high level of coordination should be ensured before, during, and after the MDTs’ meetings. Booth, Edmonds, and Kendall (2009) assert that “palliative care MDM needs effective administrative support in order to function effectively” (p.45). Administrative support should not only be limited to facilities and personnel. However, adequate resources should also be provided to the team. According to Booth, Edmonds, and Kendall (2009), there are instances whereby MDTs struggle to access resources such as the MRI. As a result, the team’s operational efficiency is adversely affected. Additionally, the lack of committed non-clinical support staff to manage the team’s operations may affect the team’s cohesiveness (Mileshkin & Zalcberg 2009). The coordinator should ensure that the MDTs’ meetings are held successfully. In order to achieve this, multidisciplinary team meetings should be comprised of a number of palliative care interventionists (Booth, Edmonds & Kendall 2009). Some of the coordinators’ duties include facilitating communication, ensuring the availability of the essential clinical information, arranging meetings, and recording decisions.
Methodology
The objective of this study is to explore the decision-making process in multidisciplinary teams. The report focuses on the decision-making process in managing cancer. As a result, the study is descriptive in nature. In an effort to develop a comprehensive understanding of the MDTs’ decision-making process, an effective research design is integrated. Maxwell (2005) defines research design as the approach used in order to order to ensure that the findings are logical. The decision to incorporate this approach was informed by the qualitative nature of the research. According to Maxwell (2005), qualitative research design enables the research to undertake a comprehensive review of the issue under investigation. As a result, a wide volume of data is gathered.
Maxwell (2011) further asserts that it is important for adequate and reliable data to be collected in order to reinforce the findings of a particular study. Thus, an effective method of data collection has to be integrated. In conducting this study, the researcher relied on secondary data. This entailed collecting data from published reports, journals, and other articles on decision making in cancer MDTs. To ensure ease of access to the data, the research relied on online sources. It was ensured that only credible articles were used. This played a significant role in enhancing the credibility of the study. A form illustrating a review of the core articles used in preparing this report is illustrated in appendix 1.
Analysis and discussion
The literature review above shows that the MDT model is increasingly being endorsed by numerous healthcare systems. In an effort to increase the likelihood of success amongst multidisciplinary teams, various healthcare systems are appreciating the contribution of multidisciplinary meetings in the decision-making process. According to Patkar and Acosta (2011), one of the reasons that explain this trend is the effectiveness and efficiency with which MDMs enable healthcare professionals to deal with complex situations. However, various challenges have been cited with regard to the decision making process in MDTs. Lack of adequate support is one of the challenges that MDTs are facing in their decision making processes. Moreover, MDTs are characterized by a lack of commitment among team members. This limits the platform’s ability to deal with complex situations.
Currently, the healthcare sector in the UK is faced with numerous challenges. Some of these challenges emanate from new diseases and conditions that require specialized treatment. The study shows that healthcare systems are integrating the concept of teamwork in an effort to deal with such situations. According to Patkar and Acosta (2011), there are two main approaches that organizations can adopt in the process of developing teams. These approaches include forming homogeneous or heterogeneous teams. The nature of the team formed depends on the complexity of the challenge faced and hence the need to make effective decisions. However, it is imperative for policymakers and managers to ensure that MDTs function effectively (Wasbeek 2004). However, Blazeby and Wilson (2006) assert that “not all MDTs decisions are implemented” (p.457). The study cites the existence of conflict amongst team members as one of the factors that limit the implementation of decisions made by MDTs. As a result, the opportunity created by MDTs in solving complex healthcare problems is not fully exploited.
Implications to managers
Currently, organizations are increasingly facing intense competition as a result of the high rate of globalization (Abdullah, Ahsan & Allam 2009). To increase the likelihood of success, managers should make effective operational and management decisions. The quality of decisions made influences the effectiveness with which an organization achieves and sustains the desired competitive advantage. In an effort to attain the desired level of competitiveness, organizations in different economic sectors are incorporating the concept of project management. However, Al-adaileh (2011) asserts that the success of a particular project depends on the effectiveness with which the project manager constitutes the project team. This study shows that it is important for managers to adopt the concept of multidisciplinary teams. In order to achieve this, managers should develop to ensure that the project team is comprised of members from a different professional backgrounds. This will play a critical role in balancing the level of expertise amongst the team members hence improving the teams’ ability to deal with complex situations (Deb 2006).
The study highlights a number of issues that organizational managers should take into account in the process of making decisions in multidisciplinary teams. To ensure that projects are completed successfully and within the set timeframe, the project manager should convene multidisciplinary team meetings occasionally. Such meetings will aid in assessing the progress of the project. This arises from the fact that the meeting will provide the team members with an opportunity to discuss various issues associated with the project. For example, the team members will be able to determine the challenges that might hinder the completion of the project.
The study has also shown that it is imperative for organizational managers to integrate good team leadership and team dynamics. Some of the issues that managers should consider include good communication and cooperation amongst team members (Deb 2006). Moreover, managers should ensure that all the project team members are involved in the decision-making process (Ryan, Windsor, Ibragimova & Prybutok 2010). This will develop a perception of being valued hence increasing their contribution to the team. The study also highlights the importance of providing sufficient administrative support to the team and time.
The implication to policy makers
The study illustrates the importance of integrating stakeholders from different functional and disciplinary backgrounds in the decision-making process. In the process of formulating policies, it is imperative for policymakers to seek the experience and skills of diverse experts (DuBrin 2012). This increases the likelihood of solving complex problems. Moreover, MDTs increases the policymakers’ level of knowledge. This arises from the fact that the policymaker gains insight on various issues that must be taken into account before a particular decision is arrived at. According to Taylor (2010), a number of core and non-core members must be included in the MDT when making decisions on the most effective treatment plan to adopt in treating a particular type of cancer.
Academic implications
The study cites cancer as one of the major challenges facing the healthcare industry. This arises from the fact that cancer presents itself in different forms which might limit individual doctors’ ability to effectively treat the disease. As a result, it is important for healthcare professionals to collaborate in order to develop effective treatment plans. This will improve the effectiveness with which the disease is diagnosed and treated hence increasing the rate of survival from various forms of cancer. To achieve this, healthcare professionals should appreciate the role of multidisciplinary teams in the decision-making process.
The study has cited a number of challenges that healthcare professionals experience in their quest to make decisions through multidisciplinary teams. Some of these challenges include lack of cooperation amongst team members, poor leadership, ineffective communication, and lack of optimal administrative support. This presents a unique research opportunity to academicians with regard to the modalities that should be ensured in order to improve the multidisciplinary team decision making capability.
Conclusion
The study highlights the significance of MDMs in improving the effectiveness with which MDTs in cancer treatment can deal with complex situations by making effective decisions. The study shows that decision making in cancer MDTs is faced with a number of challenges. However, MDTs can be effective if a number of aspects are taken into account. Some of these aspects include good team leadership, communication, and cooperation. The paper cites the benefits associated with MDMs. Some of the benefits include the elimination of inequality, optimizing resource utilization, improved cancer treatment, and planning, improved communication and coordination of services, and effective evaluation of cancer clinical trials.
The report also outlines the challenges encountered in the process of making decisions on how to treat cancer through MDTs. The heterogeneous nature of MDTs is cited as one of the sources of the challenges faced by MDTs. This arises from the fact that MDTs are composed of members from diverse professional backgrounds. For example, treatment and management of cancer require the cooperation of healthcare professionals from diverse disciplines. Consequently, it is imperative for effective team leadership skills to be integrated.
Some of the hindrances in MDTs decision making process cited in the report include lack of adequate clinical information, non-attendance of key members, technological failures, ineffective team leadership, lack of effective administrative support and processes, failure to involve patients in the decision making process, lack of investigation results and ineffective group dynamics. Such knowledge is of great significance to healthcare professionals in their quest to improve the operation of MDTs hence enhancing the decision-making process. To achieve this, multidisciplinary team leaders must integrate effective team dynamics. This can be achieved by nurturing the culture of teamwork amongst the various healthcare professionals. Through teamwork, the level of commitment towards achieving the set goal is increased. As a result, the likelihood of success in the decision-making process will be increased.
From the study, it is evident that MDMs are very effective with regard to planning the treatment, improving communication and coordination of services, increasing the knowledge of the multidisciplinary team members on the disease, and improving equality with regard to cancer treatment. Consequently, the significance of MDMs in the decision-making process cannot be underestimated. In summary, one can assert that the likelihood of healthcare professionals succeeding in treating chronic diseases such as cancer through MDTs is very high.
Learning statement
As a management student, the course has been of great importance in my personal and academic development. One of the areas that the module has been of great significance relates to a team working. First, the course has provided me with an opportunity to appreciate the importance of multidisciplinary teams in the process of making a decision to solve complex problems. Through the study, I have appreciated the importance of integrating various parties in the decision-making process. Such inclusion in the team increases the likelihood of making effective decisions that improve the outcome of a particular aspect. This arises from the fact that the team members possess diverse knowledge and expertise.
The course has provided great insight into the qualities that I should nurture as a team leader. For example, I have appreciated the importance of including all the team members in the decision-making process. By including all the members in the decision-making process, I will be able to nurture information and knowledge sharing amongst various departments. This will culminate in the development of an effective working relationship and collaboration amongst the various departments. As a result, the likelihood of attaining the desired synergy will be increased. The course has also been of great insight with regard to the various challenges that hinder the decision-making process in multidisciplinary teams. As a team leader, I will be able to eliminate such hindrances hence increasing the likelihood of success in the decision-making process.
Reference List
Abdullah, Z, Ahsan, N & Allam S 2009, ‘The effects of human resource management practices on business performance among private companies in Malaysia’, International Journal of Business and Management, vol. 4, no. 6, pp. 65-72.
Abulrahman, O 2011, ‘The effect of multidisciplinary team care on cancer management’, The Pan African Medical Journal, vol. 9, no. 20, pp. 1-5.
Al-adaileh, R 2008, Essentials of management information systems, Yazeed Publications, Karak-Jordan.
Al-adaileh, R 2011, ‘The impact of organizational culture on knowledge sharing: the context of Jordan’s phosphate mines company’, International Research Journal of Finance and Economics, vol. 63, no.5, pp. 24-35.
Blazeby, J & Wilson, L 2006, ‘Analysis of clinical decision making in multidisciplinary cancer teams’, Annals of Oncology, vol. 17, no. 3, pp. 457-460.
Burkus, D 2011, ‘Building the strong organisation; exploring the role of organisational design in strengths based leadership’, Journal of Strategic Leadership, vol. 3, no. 1, pp. 54-66.
Booth, S, Edmonds, P & Kendall, M 2009, Palliative care in the acute setting: a practical guide, Oxford University Press, Oxford.
Bruner, D 2001, Outcomes in radiation therapy: multidisciplinary management, Jones and Bartlett, Sudbury.
Cancer Research UK: Cancer mortality in the UK 2010, Web.
Carmeli, A, Atwater, L & Levi, A 2010, How leadership enhances employees’ knowledge sharing: the intervening roles of relational and organizational identification, Springer, London.
Chandrasekar, K 2011, ‘Workplace environment and its impact on organizational performance in public sector organizations’, International Journal of Enterprise Computing and Business Systems, vol. 1, pp. 1-19.
Chew J 2004, The influence of human resource management practices on the Retention of core employees of Australian organizations; an empirical study, Murdoch University, Sydney.
Deb, T 2006, Strategic approach to human resource management, Atlantic Publishers & Dist, New York.
Devvit, B 2010, ‘ Team dynamics, decision making and attitudes towards multidisciplinary cancer meetings: health professionals’ perspectives’, Journal of Oncology, vol. 6, no. 6, pp. 17-20.
DuBrin, A 2012, Essentials of management, Thomson Learning, Ohio.
Dziegielewski, S 2013, Changing face of health care social work; opportunities for professionals, Springer Publishers, New York.
European Commission: Patient involvement. 2012. Web.
Fabbro, E 2010, Nutrition and the cancer patient, Oxford University Press, Oxford.
Fawcett, J & McQueen, A 2011, Perspectives on cancer care, Wiley Blackwell, London.
Fayle, L & Hostad, J 2004, Delivering cancer and palliative care education, Radcliffe Medical, Abingdon.
Gopal, N 2009, Business communication, New Age International, New Delhi.
Grange, G 2008, Effectiveness of multidisciplinary team dynamics on treatment in a behavioural health environment, Oxford Press, London.
Holbeche, L 2009, Engaging leadership creating organisations that maximise the potential of their people, CIPD, London.
Hubbard, G 2010, ‘Treatment decision making process in cancer care: the role of the carer’, Journal of Clinical Nursing, vol. 19, no. 19, pp. 2023-2031.
Gurses, A & Xiao, Y 2006, ‘A systematic review of the literature on multidisciplinary rounds to design information technology’, Journal of the American Medical Informatics Association, vol. 13, no. 3, pp. 267-276.
Jalil, R 2012, ‘The cancer multidisciplinary team from the coordinators’ perspective; results from a national survey in the UK’, Health Services Research, vol. 3, no. 2, pp. 1-6. Web.
Kandula, S 2007, Human resource management in practice: with 300 models, techniques and tools, Prentice-Hall, New Delhi.
Kawatra, S & Krishnan, V 2004, ‘Impact of gender and transformational leadership on organisational culture’, NMIMS Management Review, vol. 16, no. 1, pp. 1-6.
Khastar, H, Kalhorian, R, Khalouei, G & Maleki 2011, ‘Levels of analysis and Hofstede’s theory of cultural differences: the place of ethnic culture in organizations’, International Journal on Financial Management and Economics, vol. 11, no. 2, pp. 320-324.
Latifi, R 2009, Telemedicine for trauma, emergencies and disaster management, Chicago Press, Chicago.
Lee, J & Ok, C 2007, Effects of workplace friendship on employee job satisfaction, organisational citizenship behaviour, turnover intention, absenteeism, and task force performance, Kansas State University, Kansas.
MacMillan Cancer Support: Improving cancer patient experience. 2012. Web.
Marchington, M & Wilikinson, A 2006, Human resource management at work; people management and development, Chartered Institute of Personnel and Development, London.
Mauk, K 2010, Gerontological nursing: competencies for care, Jones and Bartlett Publishers, Boston.
Maxwell, J 2005, Qualitative research design: an interactive approach, New Jersey, Sage Publications.
Mileshkin, L & Zalcberg, J 2009, ‘The multidisciplinary management of patients with cancer’, Annals of Oncology, vol. 17, no. 8, pp. 1337-1338.
Ministry of Health: Guidance for implementing high quality multidisciplinary meetings. 2012. Web.
Monaghan, J & Sharma, A 2005, ‘Improving patient care and communication, multidisciplinary team working and goal setting in stroke rehabilitation’, Journal of Oncology, vol. 19, no. 2, pp. 194-199.
Nutt, P & Wilson, D 2010, Handbook of decision making, Wiley, New York.
Patkar, V & Acosta, D 2011, ‘Cancer multidisciplinary team meetings: evidence, challenges, and the role of clinical decision support technology’, International Journal of Breast Cancer, vol. 4, no. 4, pp. 76-87.
Rosman, Y, Shah, F & Hussain, A 2013, ‘Factors affecting the role of human resource department in private healthcare sector in Pakistan; a case study of Rehman Medical Institute’, Research Journal of Recent Sciences, vol. 2, no. 1, pp. 84-90.
Roy-Byrne, P & Silver, J 2012, ‘Diagnosis of psychiatric and psychological disorders in patients with cancer’, Journal of Oncology, vol. 2, no. 5, pp. 1-9.
Ryan, S, Windsor, J, Ibragimova, B & Prybutok, V 2010, ‘Organizational practices that foster knowledge sharing across distinct national cultures’, International Journal of Emerging Trans-discipline, vol. 13, no.7, pp. 131-158.
Schmitt, N 2012, The oxford hand book of personnel assessment and selection, Oxford University Press, New York.
Shaw, P 2008, Making difficult decisions: how to e decisive and get the business done, Capstone Publishers, Chichester, UK.
Smidts, A, Pruyn, A & Riel, C 2001, ‘The impact of employee communication and perceived external prestige on organizational identification’, Academy of Management Journal, vol. 44, no. 5, pp.1051-1062.
Smit, P 2007, Management principles: a contemporary edition for Africa, Juta Press, Cape Town.
Sondak, V 2011, Merkel cell carcinoma; a multidisciplinary approach, Imperial College Press, London.
Tanfani, E & Testi, A 2012, Advanced decision making methods applied to healthcare, Springer, London.
Taylor, C 2010, ‘Multidisciplinary team working in cancer; what is the evidence’, BMJ Journals, vol. 7, no. 4, pp. 1-3.
Ueno, T & Cristofanilli, M 2012, Inflammatory breast cancer; an update, Springer, Dordrecht.
Victorian Government: Multidisciplinary cancer care. 2012. Web.
Wasbeek, D 2004, Human resource management practices in selected private companies, Universal Publishers, London.
Wheless, S, McKinney, K & Zanation, A 2011, ‘A prospective study of the clinical impact of a multidisciplinary head and neck tumour board’, Journal of American Academy of Otolaryngology-Head and Neck Surgery, vol. 143, no. 5, pp. 650-654.